The diagnosis of dyscirculatory encephalopathy or chronic cerebral ischemia, as it is also called, sounds scary. But what is it and why is it developing?
For our brain to function normally, it must receive adequate nutrition every day.
Our brain is fed by vessels - arteries, which bring to the brain all the necessary amino acids, vitamins, vitamin-like substances, minerals, biologically active substances, oxygen and much more. And the veins carry all the “processed products” out of the brain. When, for one reason or another, the brain “does not get enough food” or is overfilled with “waste” products, discirculatory encephalopathy , in other words, it is the suffering of the brain from improper blood supply and nutrition.
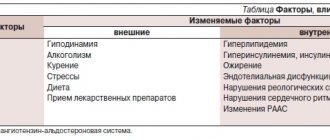
A number of factors aggravate the course and stimulate the progression of dyscirculatory encephalopathy:
- Acute and/or chronic psycho-emotional stress (stressful work, stressful situation in the family, sleep disturbance, night work, daily work without rest, work in extreme conditions). Stress triggers a destructive cascade leading to cerebral vasospasm and poor blood supply, as a result of which various biochemical processes in nerve cells are disrupted
- Hypokinesia (lack of daily dosed physical activity, lack of daily walks in the fresh air, sedentary work). For normal functioning of the cardiovascular system, it is recommended to engage in any dosed physical activity every day (!) for an hour. But this is not house cleaning work, this is not work in the country house/garden. This could be walking, cycling, swimming, dancing, any cardio training, yoga, or sports games. Such loads stimulate blood flow throughout the body and in the brain.
- Overweight and obesity . Absolutely every obese person sooner or a little later develops arterial hypertension and atherosclerotic changes in the blood vessels of the brain. Atherosclerosis was once thought to be a disease of old age. But it has long been known that atherosclerotic lesions of the aorta develop even in infants. And more and more often we see atherosclerotic changes in cerebral vessels by the age of 30. And, as a rule, this develops against the background of excess weight and poor nutrition. Moreover, I have encountered atherosclerotic plaques in the vessels of the brain in patients under 35 years of age and without obesity, and after a full examination it turned out that the only cause was poor nutrition.
- Alcohol abuse . Frequent consumption of alcohol and in large doses disrupts liver function. Namely, the liver synthesizes endogenous cholesterol (produces its own internal cholesterol). And if the liver works “poorly” and does not remove excess cholesterol from the body, then it enters the bloodstream and remains there on the inner walls of our vessels. The arteries become narrower, the blood supply to the brain is worse.
- Smoking . The smoke of one cigarette contains about 200 different compounds that contribute to inflammation of the inner wall of blood vessels. And cholesterol is layered precisely on inflamed vascular changes. The more we smoke, the more atherosclerotic plaques accumulate on the vessels of the brain and beyond. Atherosclerotic deposits in the heart arteries cause the development of myocardial infarction, and in the vessels of the legs such deposits can cause gangrene and further amputation of the leg/legs.
- Diabetes . Sweet blood is another factor in inflammation of the internal vascular wall, where cholesterol will accumulate. In diabetes mellitus, the formation of atherosclerotic plaques in blood vessels is rapidly rapid. In a relatively healthy person, small increases in cholesterol in the blood may not have any effect on the formation of plaques, but in the presence of diabetes, every drop of cholesterol will be deposited on the blood vessels. If you have diabetes, you should control your cholesterol very strictly and strictly adhere to proper diet therapy. A very dangerous combination of diabetes + smoking + arterial hypertension + obesity.
- Thyroid gland dysfunction . The thyroid gland regulates all types of metabolism in the human body, including cholesterol metabolism. With hyperthyroidism and especially hypothyroidism, cholesterol necessarily accumulates on the blood vessels, causing all those disturbances in brain function that will be discussed later. Therefore, for any diseases of the thyroid gland, hormonal status and lipid metabolism should be monitored.
- In diseases of the cervical spine , especially with neck deformities, severe stoop and/or instability of the cervical vertebrae, compression of the vertebral arteries is possible - this impairs blood flow into the vertebrobasilar basin and in the future contributes to the development and progression of discirculatory encephalopathy.
- Blood diseases with an increased level of hematocrit and/or platelets (erythrocytosis, erythremia, thrombocytosis and other related conditions) contribute to the deterioration of cerebral circulation and brain destruction.
- Heart diseases such as atrial fibrillation and other rhythm disturbances increase the risk of developing cerebral artery thrombosis.
- Vasculitis (inflammatory vascular diseases) also contributes to the destruction of brain tissue.
- Night apnea - stopping breathing during sleep - disrupts cerebral circulation and causes the development of vascular encephalopathy.
- Congenital hypoplasia (narrow diameter) of the cerebral arteries (vertebral arteries and others) can also cause the early and rapid development of dyscirculatory encephalopathy.
Disability at the second stage
The third disability group is given to those patients with dyscirculatory encephalopathy who are able to perform everyday and professional activities, but this is difficult for them. At the same time, living with the disease is possible without constant monitoring from loved ones or specialists. In general, each specific case requires an individual approach and consideration.
The second group is given to people whose condition is not limited to cephalgic syndrome (headache, tinnitus, nausea and vomiting). Due to deterioration of memory, attention, and tremors of the limbs, they are unable to maintain their ability to work. Impaired functioning is obvious, but it does not necessarily mean that the patient is completely unable to care for himself.
How does dyscirculatory encephalopathy manifest?
Its manifestations/neurological symptoms are very varied. And they are combined in an arbitrary way and always in different ways. I will only describe the sensations (complaints), there is no need to describe the symptoms of the neurological status. Your task is to catch the first symptoms by your inner sensations.
It all starts with a decrease in the level of attention and increased irritability. Then comes a feeling of discomfort in the head, anxious thoughts, and headaches. Dizziness and staggering when walking are possible. Performance and the ability to remember new information decrease, increased mental and physical fatigue appears, first at the end of the working day, then constant. Possible depressive disorders, lack of desire to do anything, lack of inspiration to live and work.
Without treatment, discirculatory encephalopathy develops into serious coordination disorders with falls and severe walking impairments, and varying degrees of severity of thinking and memory disturbances occur, up to the development of dementia (severe impairments in memory and ability to care for oneself). Possible hand tremors.
According to statistics, the initial manifestations of cerebrovascular accidents occur more often in men and appear at the age of 20-50 years. And at the age of 60-90 years, vascular encephalopathy affects 95% of people!!!
But we can protect ourselves! If you do not get rid of vascular encephalopathy completely, then at least delay its onset and stop its uncontrolled progression, leading to a significant impairment in the quality of life and decreased performance.
Who's at risk
It was previously thought that older people were more susceptible to DEP. Currently, the disease has become significantly “younger” and quite often it is diagnosed in patients who are under 50 years of age. In most cases, these are people of creative professions and mental work. The most severe consequences of discirculatory encephalopathy include senile dementia and ischemic stroke.
Factors that provoke the disease are: poor diet with a predominance of fatty and smoked foods, alcohol abuse, smoking, excess weight, hormonal disorders, high blood pressure, head injuries.
Approximate examination plan for diagnosing dyscirculatory encephalopathy:
- Complete blood count (determines the number of red blood cells, hemoglobin, platelets and other blood parameters that affect blood supply to the brain)
- Liver and kidney tests (allows you to evaluate the functioning of the liver and kidneys)
- Coagulogram (necessary to assess the risk of thrombosis and blood density)
- Lipidogram (will show cholesterol level, the ratio of “bad and good” cholesterol
- Blood glucose/glycated hemoglobin (assessment of diabetes mellitus)
- ECG (to determine heart function, detect arrhythmias)
- MRI of the head (will show the presence of dyscirculatory encephalopathy itself)
- MRI of the cervical spine (to evaluate cervical deformity and possible causes of compression of the vertebral arteries)
- Doppler ultrasound of the head and neck vessels with functional tests (will allow you to assess the presence of atherosclerotic plaques, arterial spasm and venous disorders, compression of the vertebral arteries)
- Consultation with a cardiologist (necessary for high blood pressure, heart rhythm disturbances and other diseases of the cardiovascular system)
- Consultation with an ophthalmologist with examination of the fundus (retinal vessels are a reflection of the vessels in the brain; by examining the retinal vessels, the condition of the small vessels of the brain can be assessed)
- Consultation with an endocrinologist (necessary for the treatment of diabetes mellitus, hypothyroidism, hyperthyroidism and other endocrine disorders)
- Consultation with a hematologist (for blood diseases)
- Consultation with a nutritionist (to correct nutrition and get rid of obesity)
- Psychotherapy (necessary in the presence of stress factors, anxiety and depressive disorders).
- Kinesiology and physical therapy with an instructor (if necessary, restore posture)
Treatment of DEP
The main goal of drug therapy is to restore vascular function, improve blood flow to the brain and normalize the functioning of the nervous system. For this purpose, the patient is prescribed beta-blockers, calcium antagonists, vasodilators, neuroprotectors, and anticoagulants. This is general therapy. Symptomatic treatment is aimed at eliminating individual clinical manifestations, namely depression and behavioral lability.
Surgical intervention is recommended for severe progressive DEP (the degree of vasoconstriction is more than 70%).
Causes of the disease
The primary role in pathogenesis is played by pathologies of cerebral vessels and disruption of the hemodynamic process. These factors lead to the development of ischemia of brain tissue, which occurs in acute or chronic form. Chronic ischemia in brain tissue develops due to polymorphic (various) causes.
Diagnosed arterial hypertension is considered the main risk factor that contributes to the occurrence and rapid progression of DEP. According to statistics, arterial hypertension is the main cause of cerebral ischemia, which occurs in a chronic form, and vascular dementia (dementia). Deterioration of cognitive abilities (memory and mental activity) occurs due to pathological conditions:
- Multiple cerebral infarctions with localization of foci in cortical and subcortical structures.
- Cortical or subcortical localization of ischemic foci.
- Lacunar cerebral infarctions with single foci of different localization (cortical part of the mediobasal part of the temporal lobe, angular gyrus, thalamus, white matter in the frontal lobes).
The severity of leukoaraiosis (a pathological process of damage to blood vessels located in the white matter) is closely associated with the degree of dementia. The rate of disease progression correlates with the accumulation of degenerative changes.
Classification
Taking into account the cause of development, the disease can be atherosclerotic, venous, hypertensive and mixed. Depending on the characteristics of the course, classic, galloping (rapidly progressing) and remitting varieties of the disease are distinguished. To clarify the severity of the process, a general three-stage classification is used, where:
- Stage 1 (initial). There are minor disorders of the emotional sphere and cognitive activity, there is no neurological deficit.
- Stage 2 (moderate). Cognitive-emotional dysfunction worsens and is accompanied by motor symptoms.
- Stage 3 (decompensation). The ability to work and the ability to self-care are lost, and dementia develops.