Treatment of stage 2 hypertension, symptoms and causes
Stage 2 hypertension is arterial hypertension in moderate form. The upper blood pressure (systolic) is 160 - 179 mm Hg, and the lower blood pressure (diastolic) is 100 - 109 mm Hg. At this stage of the disease, periods of increased pressure are longer than with stage 1 hypertension. Arterial blood pressure in grade 2 hypertension rarely returns to normal.
Depending on the rate of change in the degree of hypertension, we can talk about normal and malignant arterial hypertension. In the second case, the disease progresses so quickly that it is often fatal. Hypertension is dangerous because an increase in the speed of blood movement through the vessels leads to thickening of their walls and an even greater narrowing of the arteries.
Risks of developing hypertension
The risk of developing hypertension or arterial hypertension - high blood pressure - consists of a number of factors. Accordingly, the more there are, the greater the likelihood that a person will become hypertensive.
Risk factors for developing hypertension:
- stress (stress hypertension) and mental stress. The stress hormone adrenaline increases your heart rate. It instantly constricts blood vessels;
- taking certain medications, for example, oral contraceptives, and various dietary supplements (iatrogenic hypertension);
- male gender;
- age over 35 years;
- pregnancy;
- diabetes;
- endocrinopathy of the adrenal glands, thyroid gland or pituitary gland;
- diseases of the hypothalamus;
- pyelonephritis;
- renal failure (nephrogenic hypertension);
- inactivity. Physical inactivity is accompanied by a slow metabolism - metabolism - and gradually weakens the body as a whole;
- excess salt in food. Table salt provokes arterial spasm and retains fluid in the body;
- excess body weight. Each extra kilogram increases blood pressure by 2 millimeters of mercury - mmHg;
- sudden change in weather;
- hereditary predisposition. The risk of getting sick is higher for those who have hypertension among first-degree relatives: father, mother, grandmothers, grandfathers, siblings. The more close relatives suffer from high blood pressure, the greater the risk;
- bad habits: smoking or drinking alcohol. Components of tobacco provoke spasms of blood vessels - involuntary contractions of their walls. This narrows the blood flow;
- atherosclerosis – blockage of blood vessels with plaques. Total cholesterol should not exceed 6.5 mmol/l of blood;
- chronic lack of sleep and other “provocateurs”.
Depending on the combination and degree of manifestation of the above factors, as well as the likelihood of cardiovascular complications in the next decade, there are 4 types of risk of developing arterial hypertension:
- low (risk less than 15%);
- average (from 15 to 20%);
- high (more than 20%);
- very high (more than 30%).
Risk factors for the appearance of arterial hypertension are also divided into 2 types based on the possibility of their elimination: correctable (correctable) and not. For example, a person may well quit smoking, but he is not able to change his ancestry. The amount of risk is summed up from a number of indicators. A patient with stage 1 hypertension who begins to abuse alcohol will significantly increase the percentage chance of developing complications.
Principles for choosing antihypertensive drugs
A.A.
UPNITSKY ,
Russian National Research Medical University named after. N.I. Pirogova, Moscow Arterial hypertension (AH) and its complications are widespread in the population today and carry a high risk of disability and death among the population, mainly of working age (cerebral stroke, myocardial infarction, chronic heart failure, end-stage renal failure, cardiac arrhythmias, etc.) .
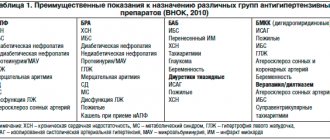
At the same time, the effectiveness of blood pressure control in patients with hypertension remains unacceptably low for various reasons. This article presents an attempt to streamline the prescription of antihypertensive drugs by applying a specific algorithm for their prescription, including adequate monitoring of the ongoing antihypertensive therapy. The article uses the latest ESC/ESH-2013 recommendations, as well as the American JNC-8 of December 2013 for the treatment of hypertension (JAMA-2014, December, online). The work provides an original algorithm for choosing antihypertensive therapy, including methods and timing for assessing both the effectiveness and safety of antihypertensive therapy. At the beginning of the article, it is appropriate to provide a classification of arterial hypertension according to blood pressure level ( Table 1
).
Table 1. Classification of arterial hypertension by blood pressure level
| Category | Systolic blood pressure, mm Hg. Art. | Diastolic blood pressure, mm Hg. Art. |
| Optimal | <120 | <80 |
| Normal | <130 | <85 |
| High normal | 130-139 | 85-89 |
| Hypertension 1st degree | 140-159 | 90-99 |
| Hypertension 2nd degree | 160-179 | 100 -109 |
| Hypertension 3rd degree | ≥180 | ≥110 |
Relationship between blood pressure and damage to the cardiovascular system and kidneys
The relationship between blood pressure and cardiovascular and renal complications and mortality has been studied in a large number of observational studies. Their main results are as follows:
1. Office BP is directly associated with the incidence of stroke, myocardial infarction, sudden death, heart failure and peripheral arterial disease (PAD), as well as end-stage renal disease (ESRD). 2. In individuals over 50 years of age, SBP appears to be a better predictor of clinical events than DBP. In elderly and senile people, pulse pressure (the difference between SBP and DBP) plays a possible additional prognostic role. This is also evidenced by a particularly high cardiovascular risk in patients with elevated SBP and normal or low DBP - isolated systolic hypertension (ISAH). 3. Blood pressure values measured outside the office, such as those obtained during ABPM and home blood pressure monitoring (HBP) are also related to clinical events. 4. The relationship between cardiovascular morbidity and mortality varies depending on the presence of other concomitant cardiovascular risk factors listed below.
Risk stratification criteria for arterial hypertension (recommendations of VNOK-2004)
Risk factors
Basic
- Men > 55 years old.
- Women > 65 years old.
- Smoking.
- Cholesterol > 6.5 mmol/L, or low-density lipoprotein cholesterol >.4.0 mmol/L, or high-density lipoprotein cholesterol < 1.0 mmol/L.
- Family history of early CCP (women <65 years, men <55 years).
- AO (OT ≥ 102 cm for men or ≥ 88 cm for women).
- CRP ≥ 1 mg/dl.
Additional
- NTG.
- Low physical activity.
- Increased fibrinogen.
Target organ damage (stage II hypertension) Left ventricular hypertrophy (ECG, echocardiography, radiography).
Microalbuminuria (30-300 mg/day). Ultrasound signs of thickening of the arterial wall (thickness of the intima-media layer of the carotid artery ≥ 0.9 mm) or atherosclerotic plaques of the great vessels. A slight increase in serum creatinine 115-133 µmol/l for men or 107-124 µmol/l for women. Associated clinical conditions (stage III hypertension)
Cerebrovascular diseases
- Ischemic stroke.
- Hemorrhagic stroke.
- Transient ischemic attack
Heart diseases
- Myocardial infarction.
- Angina pectoris.
- Coronary revascularization.
- Congestive heart failure
Kidney diseases
- Diabetic nephropathy.
- Renal failure (creatininemia > 2.0 mg/dL).
- Proteinuria (>300 mg/day).
Peripheral artery diseases
- Dissecting aortic aneurysm.
- Symptomatic peripheral artery disease
Hypertensive retinopathy
- Hemorrhages or exudates.
- Swelling of the optic nerve nipple.
Thus, to reduce cardiovascular risk and prevent the above-mentioned consequences of hypertension, along with a number of non-drug measures (control of body weight, metabolic profile, smoking control, limiting salt intake, cyclic aerobic exercise of sufficient intensity and duration, a full night’s sleep), it is necessary to achieve target blood pressure levels using primarily antihypertensive drugs.
So, how to choose them correctly? Requirements for the treatment of hypertension [1]:
- Smooth decrease in blood pressure.
- Patient compliance.
- Regression of target organ damage.
- Increasing life expectancy and improving its quality.
- Stable maintenance of blood pressure at the target level.
Target blood pressure is the blood pressure level at which the minimum risk of cardiovascular morbidity and mortality is recorded ( Table 2
).
Table 2. Target blood pressure levels
| Patient group | Target BP |
| General population of patients with hypertension | <140/90 mmHg Art. |
| Hypertension + diabetes, proteinuria <1 g/day | <130/85 mmHg Art. |
| AH + DM, proteinuria > 1 g/day | <125/75 mmHg Art. |
| AH + chronic renal failure | <125/75 mmHg Art. |
| Patients over 60 years of age | <150/90 mmHg Art. * |
| * JNC-8, JAMA, December 2014, online. | |
We propose to select antihypertensive drugs according to a certain scheme - an algorithm consisting of three main fundamental stages. The use of such an algorithm should help the doctor treating such patients to achieve maximum effectiveness and at the same time minimize the risk of side effects of the pharmacotherapy.
The first stage of choosing an antihypertensive drug is pathogenetic ( Fig. 1
). In a patient with hypertension, we suggest two steps at this stage. The first is compiling a list of drugs that effectively affect the pathogenesis of the symptom - high blood pressure. In other words, the doctor should try in each specific case to determine which hemodynamic factor “warms up”, so to speak, increased blood pressure [1-3].
Figure 1. Pathogenetic stage of selection of antihypertensive drugs
Selection of drugs depending on the cause of increased pressure
| Increased cardiac output | Increased peripheral resistance | Increased circulating blood volume |
|
|
|
Selection of drugs in accordance with their organoprotective properties
| Cardioprotective drugs | Cerebroprotective drugs | Nephroprotective drugs |
|
|
|
This factor may be, for example, increased cardiac output (in the “hyperkinetic” version of hypertension, as in hyperthyroidism, or in the early stages of hypertension in young and sometimes middle-aged people).
In patients with “experienced” hypertension, cardiac output is extremely rarely increased, and increased peripheral resistance comes to the fore in maintaining elevated blood pressure. First, it is caused by transient increases in peripheral arterial vascular resistance in response to increases in blood pressure (the meaning of this phenomenon is the protection of peripheral organs and tissues from hyperperfusion). Over time, hypertrophy of the middle muscular layer of arterioles—resistance vessels—develops, and increased peripheral resistance is fixed at the organic level. Another component of this “equation” may be an increased circulating blood volume (CBV), the so-called. volume-dependent hypertension. As a rule, these are patients with obesity (there are many small vessels in the adipose tissue with additional blood volume), with swelling or pastiness of the legs, if they are not caused by chronic venous insufficiency.
According to the assessment of the hemodynamic variant of hypertension by the attending physician, in the first case, the list of effective drugs will include those that reduce cardiac output (beta-blockers, centrally acting drugs, “rhythm-slowing” calcium antagonists) [1, 4]
In the second, this will be a list of drugs that reduce total peripheral vascular resistance (TPVR): ACE inhibitors, angiotensin II receptor antagonists of the 1st subtype (sartans), calcium antagonists (all), centrally acting drugs (I1 receptor agonists - rilmenidine, moxonidine etc.), sympatholytics (dopegit), beta-blockers with a vasodilating effect (carvedilol, nebivolol, etc.), long-acting alpha-blockers (doxazosin, terazosin, etc.), diuretics (with regular use for at least 2-3 weeks .). The latter reduce OPSS due to the removal of sodium from the vascular wall, which leads to a decrease in OPSS both by reducing its edema and by reducing its response to vasoconstrictor stimuli.
In the third case, preference will be given to diuretics. It should be remembered that mixed hemodynamic options are possible, and in such cases, drugs are combined [5].
But, given the importance of target organ damage in hypertension and organ protection, the doctor must identify in each patient with hypertension his version of target organ damage: this could be the brain and its vessels (“cerebral” version according to the old classification), the heart - in the form changes in the left sections (hypertrophy or dilatation of the left atrium and ventricle), as well as damage to the coronary arteries with an obvious or latent form of myocardial ischemia (cardiac form of hypertension); kidneys (microalbuminuria); hyperazotemia indicates advanced stages of kidney damage in hypertension. It is also possible to detect changes in the vessels of the retina or arteries of the lower extremities (also often asymptomatic, but detected during a targeted examination).
In accordance with the identified “target” organ (“targets”), the doctor compiles, still at the same first stage, a list of antihypertensive drugs that have appropriate organoprotective properties for hypertension (cardio-, cerebro- or nephroprotective).
ACE inhibitors, angiotensin II receptor antagonists of the 1st subtype (sartans), beta-blockers, calcium antagonists (to varying degrees), indapamide have proven cardioprotective properties; centrally acting antihypertensive drugs have moderate effects [1, 6–8].
Calcium antagonists (nimodipine) have cerebroprotective properties in hypertension, although this issue is not yet completely clear.
Nephroprotective properties in hypertension have been proven for ACE inhibitors, especially with a combination of hypertension and diabetes mellitus, angiotensin II receptor antagonists of the 1st subtype (sartans), as well as calcium antagonists.
Having now compared both lists (“hemodynamic” and “organoprotective”), the doctor should leave in the final list of the 1st stage only those drugs that are present in both lists simultaneously. This will be the final list of the 1st stage - a list of drugs that are effective in this particular case, but not yet taking into account their safety for the patient.
This aspect of drug selection is the subject of the second stage, in which the list of antihypertensive drugs that are effective for a given patient in a given situation, compiled at the first stage, should be considered from a different angle, namely: whether all effective drugs from this list will be safe for this patient. To solve this problem, we must return to the anamnesis (indications in the anamnesis of intolerance or unsatisfactory tolerability of certain drugs, including those related to those prescribed). Next, you should review the list of concomitant diseases in this patient - contraindications to taking certain medications may also be identified here. For example, if you have a history of bronchial asthma, drugs from the group of beta-blockers are contraindicated. These same drugs, with the exception of beta-blockers, which have vasodilating properties, are contraindicated in patients with stenosing atherosclerosis of the arteries of the lower extremities, with intermittent claudication. Beta-blockers are also contraindicated in cases of atrioventricular block above degree I/bradycardia less than 50 per minute. Alpha-blockers are contraindicated in case of concomitant angina pectoris, as they can cause an increase in anginal attacks. Sympatholytics, which have recently been used extremely rarely, are contraindicated in persons with peptic ulcer disease. Calcium antagonists are contraindicated in patients with gastroesophageal reflux disease (GERD) because they cause relaxation of the lower esophageal sphincter and thereby may worsen the symptoms of GERD. Calcium antagonists, primarily verapamil, can significantly aggravate constipation and are therefore contraindicated in this category of patients. Diuretics can increase the level of uric acid in the blood, and therefore hyperuricemia and gout are contraindications for them. For carbohydrate metabolism disorders, the only safe diuretic is indapamide. A number of antihypertensive drugs can have a negative effect on the course and outcome of pregnancy. Therefore, a limited range of antihypertensive drugs is prescribed for it [1, 6, 7]:
- Methyldopa.
- Labetolol.
- Pindolol.
- Oxprenolol.
- Nifedipine SR.
- Hydralazine.
- For kidney disease - diuretics.
Thus, after the 2nd stage of selection, only drugs that are effective and at the same time safe for a patient with hypertension will remain on the list.
The third and final stage of choosing an antihypertensive drug is the stage of individualization of pharmacotherapy.
The first step is to decide what pharmacotherapy is indicated for this patient (mono-or combined). When resolving this issue, one should proceed from the degree of increase in blood pressure and the duration of hypertension. With long-term hypertension, with high numbers, you should start with a combination of antihypertensive drugs from the very beginning. At the same time, rational and irrational combinations of antihypertensive drugs are distinguished ( Fig. 2
).
possible combinations (only dihydropyridine calcium antagonists can be normally combined with β-blockers) Red continuous line: not recommended combination |
In cases of mild hypertension, not corrected by non-drug treatment methods (see above), and moderate hypertension, monotherapy is possible in some cases.
However, in the treatment of hypertension there is a rule: combinations of antihypertensive drugs with different mechanisms of action are preferable to high-dose monotherapy. Firstly, in combination, the effect is achieved by influencing different parts of the pathogenesis of hypertension, and secondly, with the right combination, the side effects of the drugs are mutually neutralized. For example, “escape” of the hypotensive effect due to the activation of counter-regulatory mechanisms manifests itself when taking arteriolar vasodilators by increasing cardiac output; when taking all antihypertensive drugs, except diuretics, due to sodium and water retention in the body; when taking diuretics – due to the activation of the body’s neurohormonal systems, in particular the renin-angiotensin-aldosterone system [1, 5, 6]. The choice of method of administration of an antihypertensive drug is determined by the clinical situation: in case of an acute rise in blood pressure, drugs are administered parenterally (intravenously or intramuscularly), as well as sublingually (Capoten, Prazosin, Corinfar, etc.) ( Table 3
). It should be noted that these drugs have a short onset of effect and at the same time a short half-life. That is, they should be used specifically in acute situations, and are much less suitable for long-term use. The fact is that when taking short-acting drugs, there are constant fluctuations in their concentration in the blood, and after them, fluctuations in their hypotensive effect, which is accompanied by significant variability in blood pressure during the day. The latter is an unfavorable factor; in particular, the risk of hypertension complications increases. In addition, when taking the last dose of such a drug, even before bedtime, it still does not prevent the morning rise in blood pressure.
Table 3. Medicines for self-relief of blood pressure rise (according to M.V. Leonova, 2012, as amended)
| Drug (INN*) | Method of administration | Start of action | Maximum effect | Duration of action | Doses |
| Captopril | Inside, under the tongue | 15 minutes | 1-2 hours | 4-6 hours | 12.5-50 mg |
| Clonidine | Inside, under the tongue | 30 min | 1-2 hours | 8-12 h | 0.075-0.15 mg |
| Nifedipine | Orally or chew | 15 min 5 min | 30 min 15 min | 4-6 hours 4 hours | 10-20 mg |
| Prazosin | Inside, under the tongue | 15-30 min | 1-2 hours | 8 hours | 1-2 mg |
| Nitroglycerine | Under the tongue, lingual spray | 1 min | 15 minutes | 30 min - 1 hour | 0.3-0.5 mg |
| * International nonproprietary name. | |||||
Here it should be recalled that in case of exacerbation of hypertension, one should try to identify its cause.
In this case, we may encounter the patient’s abuse of table salt, alcohol, taking non-steroidal anti-inflammatory drugs to relieve pain (arthrosis, arthritis, sciatica, headaches, etc.), constant lack of sleep for some reason, non-compliance with the recommended pharmacotherapy (skipping medications). Therefore, long-acting drugs with a long half-life are indicated for continuous maintenance antihypertensive therapy. Another important advantage of drugs with a long duration of action is the possibility of taking them once or twice a day, which helps to increase patient adherence to treatment (according to some data, in the treatment of hypertension during the year it is about 40%). Obviously, this does not mean adequate blood pressure control.
In this regard, the antagonist of angiotensin II receptor subtype 1, candesartan, is of interest; it has the longest half-life of all drugs in this group (more than 24 hours), which makes it possible to achieve blood pressure control also in the morning. In addition, candesartan has advantages over other drugs in cases of combination of hypertension with chronic heart failure, type 2 diabetes mellitus, diabetic nephropathy, proteinuria, and left ventricular myocardial hypertrophy.
To date, the results of 14 placebo-controlled studies with candesartan in 3,377 patients with hypertension are available. Daily doses of the drug ranged from 2 to 32 mg with a follow-up period of 4 to 12 weeks. Baseline blood pressure (diastolic) (DBP) ranged from 95 to 114 mmHg. Art. Within this dosage range, 2,350 patients received active candesartan therapy and 1,027 patients received placebo. In all studies, a significant hypotensive effect of candesartan was noted, which was dose-dependent, i.e., it was more pronounced the higher the dose of candesartan.
From a safety standpoint, the absence of a “first dose effect” was demonstrated, i.e., when taking the first dose of candesartan, there was no sharp decrease in blood pressure. As with other antihypertensive drugs, the hypotensive effect of candesartan increased during the first two weeks and by the end of this period was already clearly expressed. Similar to other antihypertensive drugs, the maximum effect was observed at the end of the 1st month of therapy. Moreover, the hypotensive effect of candesartan did not depend on the age or gender of patients, as well as on race and ethnicity. Of particular note is the good tolerability of candesartan even at a daily dose of 32 mg.
As for the stability of the hypotensive effect, in studies lasting up to one year there was no evidence of the hypotensive effect of candesartan.
Comparative studies of candesartan and losartan in hypertension were also conducted (CANDLE, CLAIM I and II studies, meta-analysis by Zhenfeng Zh, Huillan Shi, Junya Jia et al.), which demonstrated the advantage of candesartan in terms of the severity of blood pressure reduction and its tolerability by patients.
Thus, candesartan has a long-term pronounced hypotensive effect, which depends on the dose of the drug.
The intervals between doses of antihypertensive drugs, with the exception of diuretics, are 2-3 half-lives of the drug and are indicated in the instructions for it. At the same time, one should keep in mind the possibility of reducing the duration of action of antihypertensive drugs when they are accidentally simultaneously prescribed with drugs that are inducers of hepatic metabolism, accelerating the metabolism of antihypertensive drugs in the liver and their excretion from the body. Inducers of hepatic metabolism include, in particular, phenobarbital, other anticonvulsants, rifampicin, etc. In such cases, the intervals between doses of antihypertensive drugs should be reduced [1, 6].
Duration of treatment. With a certain “experience” of hypertension in the body, a “reconfiguration” (“resetting”) of blood vessels, kidneys, brain, and heart occurs to work at elevated blood pressure. In addition, the body retains mechanisms that support hypertension (except for rare cases of surgical treatment of arterial stenosis, removal of adrenal aldosteroma, pheochromocytoma, thyroidectomy and some others). That is why, after normalization and stabilization of blood pressure, antihypertensive therapy should not be stopped. Another thing is that over time, especially in the warm season, it is permissible to reduce the dose and amount of antihypertensive drugs under the control of blood pressure and well-being, provided that all non-drug methods of lowering blood pressure are followed. Criteria for assessing the effectiveness and safety of antihypertensive therapy
To assess the effectiveness, along with assessing the dynamics of the patient’s well-being, office BP measurements should be used, as well as additional methods: 24-hour BP monitoring - ABPM, home measurement (HBP) by the patient.
When measuring office blood pressure, this should be done repeatedly at intervals of 2 minutes, following certain rules. In addition, to assess the safety of antihypertensive therapy, especially alpha-blockers, diuretics, ACE inhibitors and their combinations, blood pressure should be measured in clinostasis (lying down, after 5 minutes) and in orthostasis (after 2 minutes in an upright position). A pronounced decrease in blood pressure in orthostasis (by 20 mm Hg or more) increases the risk of cardiovascular complications and may adversely affect the patient’s well-being.
Additional methods of blood pressure control (ABPM and DMBP) make it possible to avoid unnecessary and unsafe therapy for the patient in the case of “white coat hypertension”, to identify patients with a predominantly nocturnal rise in blood pressure or with an insufficient or excessive decrease in blood pressure at night. The information obtained is valuable for the correct selection and evaluation of antihypertensive therapy [1, 2, 6–8].
To help the practitioner, we provide a list of some fixed combinations of antihypertensive drugs ( Table 4
).
Table 4. Fixed combinations of antihypertensive drugs
| Angiotensin-converting enzyme inhibitor + calcium antagonist |
| Enalapril 5 mg + felodipine 5 mg Benazepril 10/20 mg + amlodipine 2.5/5 mg Perindopril 5/10 mg + amlodipine 5/10 mg Trandolapril 1/2/4 mg + verapamil SR 180/240 mg Enalapril 10 mg + diltiazem 180 mg Lisinopril 10/20 mg + amlodipine 5/10 mg Ramipril 5 mg + felodipine retard 5 mg |
| Angiotensin II receptor antagonist + calcium antagonist |
| Valsartan 80 mg + amlodipine 5 mg |
| Angiotensin-converting enzyme inhibitor + diuretic |
| Lisinopril 10/20 + hydrochlorothiazide 12.5/25 mg Captopril 25/50 + hydrochlorothiazide 12.5/25 mg Enalapril 20 mg + hydrochlorothiazide 12.5 mg Enalapril 10 mg + hydrochlorothiazide 25 mg Enalapril 10 mg + hydrochlorothiazide 12.5 mg Quinapril + Hydrochlorotiazide 12.5/25 mg Lisinopril 10 mg + hydrochlorotiazide 12.5 mg ramipril 5 mg + hydrochlorotiazide 12.5 mg fosinopril 20 mg + hydrochlorotiazide 12.5 mg moexipril 15 mg + hydrochlorotiazide 25 mg cylized 5 mg + hydrochlorotiazide 12.5 mg Perindopril 2 mg + indapamide 0.625 mg Perindopril 4 mg + indapamide retard 0.5 mg |
| Angiotensin II receptor antagonist + diuretic |
| Losartan 50 mg + hydrochlorothiazide 12.5 mg Valsartan 80 mg + hydrochlorothiazide 25 mg Eprosartan 600 mg + hydrochlorothiazide 12.5 mg Irbesartan 150/300 mg + hydrochlorothiazide 12.5 mg Telmisartan 80 mg + hydrochlorothiazide 12.5 mg Telmisartan 40/8 0 mg + hydrochlorothiazide 12.5 mg Candesartan 8 mg + hydrochlorothiazide 12.5 mg |
| β-blocker + diuretic |
| Pindolol 10 mg + clopamide 5 mg Bisoprolol 2.5 mg + hydrochlorothiazide 12.5 mg Propanolol 40/80 mg + hydrochlorothiazide 12.5 mg Bisoprolol 2.5/5/10 mg + hydrochlorothiazide 6.25 mg Metoprolol 50/100 mg + hydrochlorothiazide 25/50 mg Atenolol 100 mg + chlorthalidone 25 mg Atenolol 50/100 mg + chlorthalidone 12.5/25 mg Calcium antagonist + |
| β-blocker |
| Felodipine retard 5 mg + metoprolol succinate 50 mg Amlodipine 5 mg + atenolol 50 mg |
In conclusion, we urge all doctors involved in the treatment of hypertension in outpatient and inpatient settings to approach the diagnosis and treatment of patients with hypertension thoughtfully, clearly understanding the sequence of actions for diagnosis and selection of antihypertensive therapy, and we wish them good luck on this thorny path.
BIBLIOGRAPHY
1. Recommendations for the treatment of arterial hypertension. ESH/ESC 2013. Russian Journal of Cardiology, 2014, 1: 5-92. 2. VNOK. Prevention, diagnosis and treatment of arterial hypertension. Russian recommendations (fourth revision). M., 2010. 3. Recommendations of VNOK. Diagnosis and treatment of arterial hypertension. M., 2009: 5-34. 4. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: Recommendations, review, and responsibility. JAMA, 2013, December 18. 5. James PA, Oparil S, Carter BL et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA, 2013, December 18. 6. Peterson ED, Gaziano JM, Greenland P. Recommendations for treating hypertension: What are the right goals and purposes? JAMA, 2013, December 18. 7. Sox HC. Assessing the trustworthiness of the guideline for management of high blood pressure in adults. JAMA, 2013, December 18. 8. Wood S. JNC 8 at Last! Guidelines Ease Up on BP Thresholds, Drug Choices. Medscape, December 18 (https://www.medscape.com/viewarticle/817991).
The danger of high blood pressure
The main danger of hypertension is its complications, leading to disability and death.
The most severe complications:
- from the heart - heart attack, development of arrhythmia, heart failure;
- in the brain - stroke, loss of memory and intellectual abilities (dementia);
- from the eyes - severe vascular disorders in the retina;
- kidney – the occurrence of failure;
- vessels - aneurysm (sac-like expansion) of the aorta, the rupture of which leads to almost instant death.
Characteristic symptoms
Symptoms develop in isolation only in the case of the primary origin of the pathology. If hypertension is a complication of other diseases, the symptoms develop nonspecific.
General symptoms of stage 3 arterial hypertension:
- A sharp, unbearable headache localized in the occipital, temporal and parietal areas.
- Disorientation in space. An increase in blood pressure leads to dysfunction of the vestibular apparatus, as a result of which it is difficult for the patient to navigate in space.
- Ringing, noise in the ears.
- Weakness, drowsiness or, conversely, hyperactivity. In the latter case, the patient is very overexcited, it is difficult for him to relax and fall asleep even if he is very tired and feels unwell.
- Memory loss, slow thinking. The patient cannot always follow the meaning of the conversation and often forgets recent events.
- Arrhythmia. It manifests itself as a rapid or, conversely, pathologically rare heartbeat.
In the chronic course of hypertension, the symptoms are blurred. The pain in the head almost disappears and makes itself felt only periodically. Other suspicious symptoms may be completely absent.
What is stage 2 hypertension
Stage 2 hypertension is a condition characterized by a persistent increase in blood pressure to 160/100 and above. However, blood pressure rarely returns to normal on its own; drug treatment is required to correct the patient’s condition.
Stage 2 hypertension is more common in patients over 50 years of age and this is understandable. With age, changes occur associated with the deposition of cholesterol plaques and narrowing of the lumen of blood vessels, the load on the heart increases, which has to make more efforts to pump blood, and conditions arise for increased blood pressure.
general information
Blood pressure is one of the main indicators of cardiac activity, which is determined by two quantities:
- systolic value (upper pressure) - occurs during systole (contraction) of the left ventricular myocardium and the release of a portion of blood into the aorta;
- diastolic value (lower pressure) - depends on the tone of the vascular wall in the diastole (relaxation) phase of the ventricle.
The value of blood pressure is influenced by such indicators as:
- the volume of blood circulating in the vessels - as the volume of blood volume increases, the pressure increases and vice versa;
- condition of the vessels - the smaller the diameter or the more narrowed the lumen, the greater the resistance and the higher the pressure;
- heart rate - the faster the heart works, the more blood is pumped per unit time and the higher the blood pressure.
The norm for an adult is considered to be values that range from 100/60 to 139/89 mm Hg. Art. During the day, blood pressure values change many times; jumps upward can occur after physical activity, with excitement, after a cup of coffee or a cigarette. Such temporary changes have nothing to do with hypertension.
A single detection of elevated blood pressure cannot indicate that a person has this diagnosis. The setting and circumstances in which the procedure is carried out must be taken into account. To confirm the presence of a disease in a patient, for example, stage 2 hypertension, it is necessary to carry out regular measurements of blood pressure over time. Based on a series of consistently elevated numbers, a preliminary conclusion can be made; the final diagnosis is made after examination and clarification of the cause of the development of the pathology.
Symptoms of stage 2 hypertension
Stage 2 hypertension has ambiguous symptoms and treatment. Increased blood pressure may be accompanied by the following symptoms:
- Throbbing pain in the temporal region;
- Swelling of the face, especially the eyelids;
- The facial skin is hyperemic, and spider veins appear over time;
- Hands swell;
- It gets dark in the eyes, “spots” periodically flicker;
- At the same time, there is aching pain in the back of the head;
- After waking up, there is no cheerfulness, fatigue and apathy persist throughout the day;
- Periodic noise in the head;
- Emotional lability – low threshold of excitability;
- Dilated blood vessels of the eyes (sclera);
- Compaction of the ventricular wall (resistance to blood flow is compensated);
- Involuntary urination due to renal failure;
- Heart rate increases with the slightest exertion;
- There are problems with remembering.
Hypertension of the 2nd degree, symptoms can change depending on its characteristics: a primary independent form or a secondary one, as a complication of another disease.
Diagnostic measures
A treatment regimen is drawn up by a cardiologist after a comprehensive examination, identifying pathologies in target organs, determining the form of the disease and the causes that led to the disorder. But the main sign remains the indicators of systolic and diastolic pressure. To determine these data, studies are carried out on:
- pressure stability throughout the day;
- degree of risk of developing complications of the disease;
- exclusion or confirmation of increased blood pressure as a complication of other ailments;
- identification of factors contributing to hypertension;
- identification of pathological changes in other organs and systems.
The first thing the doctor does is measure your blood pressure and give recommendations for self-diagnosis at home. For hypertension, blood pressure is measured 2-3 times a day for a week, recording all data in a special diary. This allows the doctor to make an accurate diagnosis and take into account the peculiarities of the course of the disease. The physical examination is complemented by the collection of data obtained from a patient interview.
Additionally, daily blood pressure monitoring is prescribed using a special device in a hospital setting. An obligatory part of the diagnosis is an electrocardiogram and ultrasound of the heart. The techniques help to see any type of tacharrhythmia and assess the thickness of the ventricular walls. If abnormalities in the functioning of the internal organs are suspected, a magnetic resonance therapy study is carried out, and ultrasonography is prescribed to determine the size of the kidneys.
Risk 2 for stage 2 arterial hypertension
When establishing the risk of a characteristic illness, doctors take into account the age, gender, and presence of chronic diseases in the body of a clinical patient. This information helps predict clinical outcome and reduce the likelihood of serious health complications and disability. Risk 2 for arterial hypertension of the 2nd degree means that irreversible processes in internal organs under the influence of surges in blood pressure are observed only after 10 years, the probability of stroke and heart attack is 20%.
Treatment methods
To stabilize blood pressure, the following groups of drugs are prescribed:
- calcium channel blockers;
- α and β-blockers;
- ACE inhibitors;
- diuretics;
- sedatives;
- medications that have a blood-thinning effect;
- vitamin and mineral complexes that strengthen the immune system.
In advanced cases, surgical intervention is performed. Indications for surgery for stage 3 hypertension:
- acute vascular stenosis;
- advanced atherosclerosis;
- renal pathologies;
- heart disease;
- aortic aneurysm.
Arterial hypertension 2 degrees risk 4
Risks of arterial hypertension 2 degrees The presence of a “bouquet” of diseases (atherosclerosis, diabetes, ischemia) allows us to state that the patient has acquired a diagnosis of hypertension 2 degrees, 4 risk. Arterial hypertension at this stage only complicates the situation. This diagnosis is given to patients who have survived 1-2 heart attacks, regardless of the affected area.
It should be clarified that one hundred risk is a predictable concept, not an absolute one. It only indicates the likelihood of a complication developing. If the patient understands the danger of his situation and takes appropriate measures, the diagnosis can be corrected. Hypertensive patients who adhere to a healthy lifestyle and constantly monitor their condition can live a long and fulfilling life.
While with a burdened anamnesis and high risk, life expectancy is significantly shorter. Timely diagnosis and adequate treatment aimed at reducing blood pressure can extend your life and improve your quality of life.
Diagnostics
Diagnosis of arterial hypertension includes several stages:
- Collection of complaints and medical history.
- Repeated blood pressure measurements at least 2 times during different visits to the doctor.
- Physical examination.
- Laboratory and instrumental examination.
At the first stage, the doctor will find out what symptoms are bothering you and how long ago they appeared. Find out whether you smoke, whether you drink alcohol and in what doses, and whether your relatives have cardiovascular diseases.
Keep a blood pressure diary for 10 days. To do this, it is necessary to measure blood pressure at least 3 times a day. Show your doctor your notes at your next appointment. He will analyze the results obtained and, based on this, decide on the tactics for further examination and treatment.
Physical examination includes auscultation of the heart, determination of its boundaries, and heart rate. The doctor will definitely check your pulse and its tension. Measure your waist circumference, weigh you, and determine your body mass index.
Laboratory diagnostics:
- general blood and urine analysis;
- level of proteinuria and microscopy of urinary sediment;
- biochemical blood test - sugar, ALT, AST, creatinine, K, Na ions, total cholesterol and lipid profile.
Instrumental diagnostics:
- ECG;
- ECG with stress;
- EchoCG;
- Ultrasound of the brachiocephalic arteries;
- Ultrasound of the kidneys;
- chest x-ray;
- Holter monitoring ECG;
- daily blood pressure monitoring;
- consultation with an ophthalmologist, endocrinologist.
Additional examinations that are not included in the standard may be required, for example, a hormonal mirror. In rare cases, hospitalization in a hospital may be required. This is necessary for a more accurate diagnosis. As a result of examinations, the doctor makes a diagnosis and prescribes treatment.
And also read on our website: What to do if you don’t know how to write a thesis on the treatment of hypertension?
Treatment of stage 2 hypertension
How to treat stage 2 hypertension? The scheme is drawn up by the local therapist. If necessary, a consultation with a cardiologist and neurologist is scheduled. Traditional methods of treating stage 2 hypertension include:
- To eliminate blood thickness (thin the blood flow), you should take Aspirin, Cardiomagnyl, Heparin, Aspicard.
- To normalize blood pressure, diuretics (diuretics) are prescribed, such as Diuver, Furosemide, Piretanide, Torasemide, Veroshpiron, Ravel.
- For this diagnosis, thiazides (thiazide drugs) such as Arifon, Chlorthalidone, Indapamide are recommended.
- To reduce blood cholesterol, you should take lipid-lowering drugs such as Atorvastatin, Atoris, Liprimar, Zovasticor.
- In order to dilate blood vessels, antihypertensive drugs of different groups are prescribed, such as Physiotens, Artil, Bisoprolol, Lisinopril.
It is important to consider that the quality of treatment largely depends on compliance with the instructions for their use. Self-medication for hypertension is dangerous. Such experiments can result in disability. The therapist selects the treatment regimen individually, taking into account the age, build and other health characteristics of the individual patient.
Stages of the disease
Advertising:
When making a diagnosis, it is also important to find out at what stage the pathological process is in a given patient. This characteristic reflects the presence and degree of damage to vulnerable organs. There are three stages of the disease.
- First
– it is not characterized by the presence of changes in other organs. - The second
is that there are signs of changes in one or several organs due to a prolonged increase in pressure. This can be manifested by a violation of the structure of the vessels of the fundus of the eye, hypertrophy of the myocardium of the left parts of the heart, the presence of atherosclerotic damage in large vessels, coronary arteries, albuminuria within 300 mg per day, an increase in the level of creatinine in the blood to 20 mg/l (signs of developing renal failure). - Third stage
– along with the changes listed above, revealed by the results of instrumental and other studies, there are also such phenomena as angina pectoris, disturbances of conductivity and heart rhythm, chronic circulatory failure, nutritional disorders in the brain (transient or stroke), the development of encephalopathy, decreased intellectual functions , visual impairment associated with retinal hemorrhages. On the part of the kidneys, there may be signs of renal failure, and on the part of large vessels - the presence of a dissecting aortic aneurysm, signs of arterial occlusion, which is manifested by intermittent claudication, the development of gangrene of the fingers of the lower extremities, intestinal ischemia and other pathologies.
When a diagnosis is made, the stage of arterial hypertension can only be increased. For example, if there are positive results from drug therapy or surgical treatment of vascular lesions, the stage of the disease will not decrease, but will remain at the same level.
Diet for hypertension
In order for the kidney vessels to function normally, hypertensive patients with any stage of the disease must adhere to certain nutritional rules. For example, it is important to control the water and salt balance of the body, to prevent the formation of stagnation and, as a consequence, stage 2 hypertensive crisis. Fatty, fried, sweet and smoked foods are prohibited.
Seven foods that lower blood pressure:
- Blueberries – Blueberries are rich in natural substances called flavonoids.
- Fresh leafy greens such as fenugreek leaves, kale, mint leaves, patchouli, dill greens, mustard leaves, curry leaves, beet greens, Swiss chard, arugula, broccoli, celery and spinach are high in potassium
- Potatoes - contain a lot of potassium and magnesium
- Beets – Nitrates in beet juice are known to lower blood pressure
- Skim milk is an excellent source of calcium plus low fat levels
- Oatmeal is a high-fiber, low-fat, low-sodium food.
- Bananas – Adds potassium to your diet.
Therapeutic nutrition for stage 2 hypertension allows boiled lean meats, cereals, vegetables and fruits on the menu. Green tea and diuretic herbal decoctions have beneficial properties.
Gradation of risk of complications
Depending on the presence of certain factors, four degrees of risk of hypertension are distinguished, according to which the likelihood of developing fatal complications of the disease in the next ten years
.
Advertising:
Table. Gradation of risks
| Other risk factors, asymptomatic end organ damage or associated diseases | High normal pressure | AH 1st degree | AH 2 degrees | AH 3 degrees |
| No other risk factors | Low risk | Medium risk | High risk | |
| 1-2 risk factors | Low risk | Medium risk | Medium and high risk | High risk |
| 3 or more risk factors | Low to medium risk | Medium and high risk | High risk | High risk |
| Target organ damage, stage 3 CKD. or diabetes | Medium and high risk | High risk | High risk | High and very high risk |
| Cardiovascular disease, CKD 4 or higher, diabetes with end-organ damage/risk factors | Very high risk | Very high risk | Very high risk | Very high risk |
A low risk of fatal complications is established when the patient does not have the factors listed above. When there are no more than two risk factors, the probability is set as average. Risk 3 is determined in patients with three harmful factors, and risk 4 is established in the presence of four or more.
Based on the information listed above, we can say that second-degree hypertension with a risk of 2 will mean that the patient has an increase in blood pressure in the range from 160 to 176 mm Hg, and there are one or two risk factors for severe complications.
Folk remedies
When treating illness at home, many people prefer to use folk remedies. This therapy involves the use of medicinal plants that have a positive effect on the cardiovascular system.
You can treat the disease with the following recipes:
- Treatment can also be carried out with peppermint, cinquefoil, chamomile, and yarrow. These herbs go well together.
- Prepare a decoction of motherwort, horsetail, marsh cudweed, and valerian root. All plants must be taken in the same quantity. This remedy has diuretic effects and allows you to cope with single surges in blood pressure.
- Bee products and citrus fruits are actively used in the treatment of hypertension.
- You can treat with viburnum juice. To reduce blood pressure, it should be consumed three times a day, a quarter glass.
Folk remedies help cope with unpleasant symptoms of the disease and speed up the effectiveness of traditional therapy. Such recipes have proven their benefits over many centuries. People whose bodies do not tolerate medications well turn to this type of therapy. But it is important to remember that treatment of the disease with traditional recipes can only be carried out after consultation with a doctor.
Diagnosis and treatment of hypertension
Diagnosis of the disease
Diagnosis of hypertension at the A-Media clinic is carried out using the following methods:
- blood pressure measurement
- ECG
- 24-hour ECG monitoring with blood pressure (Holter monitoring)
- echocardiography (echocardiography or ultrasound of the heart)
- Ultrasound of the abdominal cavity with kidneys
- Ultrasound Dopplerography of the BCA (ultrasound Dopplerography of brachiocephalic arteries and veins).
Treatments for hypertension
Treatment of hypertension in our clinic is planned by a qualified cardiologist only after an accurate diagnosis has been made.
First step: Our doctor will take measures to lower the patient's blood pressure.
Further therapy is planned individually based on the type of hypertension. Mild and moderate forms of the disease can be treated with medications. For severe hypertension, antihypertensive drugs are always prescribed. Lifestyle modification is a prerequisite.
Prevention
Your healthcare provider will likely also suggest a variety of lifestyle changes, including:
- Maintaining a healthy weight;
- A diet rich in fruits, vegetables and low-fat dairy products;
- To give up smoking;
- Limiting salt intake in the diet;
- Limit alcohol consumption. For most adults, this means that it is normal to drink up to one drink per day for women of all ages and men over the age of 65, and up to two drinks per day for men 65 or younger;
- Exercise at least 30 minutes a day. These include walking, jogging, strength training, yoga, and cardio exercises such as cycling.
On your part, methodical adherence to medical recommendations and organization of the correct regimen are required. A healthy lifestyle is the path to recovery. Remember this.
At President-Med clinics you can
- undergo examination and treatment in more than 30 medical specialties, rehabilitation after strokes, surgeries, injuries,
- pass various types of tests (more than 5,000 types of tests and laboratory tests),
- undergo functional diagnostics (ultrasound, endoscopy: gastroscopy), ECG, installation and interpretation of ABPM and Holter ECG and others,
- pass a medical examination in one day, undergo a medical examination (for both organizations and individuals), undergo a medical examination (for both organizations and individuals),
- obtain all kinds of certificates - certificates from the traffic police and for admission to sports, to purchase weapons, to a sanatorium,
- if there is evidence, issue a certificate of temporary incapacity for work,
- draw up and receive other types of medical documentation,
- make any injections,
- use the services of one-day surgery or day hospital.
Forecast
Arterial hypertension is a progressive pathology. Over time, it leads to the development of severe complications that can cause the death of the patient. Among the most common lethal complications are myocardial necrosis, decompensated heart and vascular failure, hemorrhagic stroke, and impaired renal excretory function.
A persistent increase in blood pressure greatly increases the risk of cardiovascular complications. The mortality rate among patients with this disease in the second stage compared to the rest of the population is on average four times higher. First of all, this applies to patients who do not control their blood pressure. People who regularly take antihypertensive medications and follow their doctor's recommendations have a much lower risk of such complications, resulting in a significantly lower mortality rate.
These severe consequences of the disease can only be avoided by paying close attention to your health, visiting a doctor on time and following his recommendations regarding treatment and lifestyle changes.