Rational combinations of antihypertensive drugs
Lecture transcript
XXVI All-Russian Educational Internet Session for doctors
Total duration: 20:10
Oksana Mikhailovna Drapkina, executive director of the Internet Session, secretary of the interdepartmental council on therapy of the Russian Academy of Medical Sciences: - It is with great pleasure that I give the floor to Professor Maria Genrikhovna Glezer. "Rational combinations of antihypertensive drugs"
00:10
Glezer Maria Genrikhovna, Doctor of Medical Sciences:
– Dear colleagues. Arterial hypertension is currently the No. 1 risk factor. In 2010, it was recognized by the World Health Organization as the No. 1 killer. It is high blood pressure that determines more than 50% of all cases of coronary heart disease and strokes.
What are the classes of drugs for long-term treatment of arterial hypertension. 8 classes. But we must first use the first 5 classes:
- diuretics;
- beta blockers;
- ACE inhibitors;
- sartans;
- calcium channel blockers.
Alone or in combination, these drugs are used to reduce the risk of complications.
There is a sufficient evidence base for these first five drugs. These classes of drugs may reduce cardiovascular morbidity and death.
What are the main pathophysiological mechanisms involved in increased blood pressure?
This is the activation of the renin-angiotensin system. Activation of the sympathetic nervous system. Increase in circulating blood volumes (changes in water and electrolyte balance).
Ultimately, these systems will lead to changes in intracellular calcium transport. The drugs that we have affect different stages of pathogenesis.
Beta blockers, sympatholytics, imidazoline receptor agonists - for increased activity of the sympathetic nervous system. Diuretics – for increased circulating blood volume, lipid metabolism disorders. Calcium antagonists – to change intracellular calcium transport. 3 groups of drugs (inhibitors, sartans and direct renin inhibitors) - on the activated rhinin-angiotensin system.
We know well from clinical practice that all patients with arterial hypertension are different. The contribution of each pathogenetic mechanism may vary from person to person. For some, an increase in circulating blood volume prevails. Some people have predominantly increased activity of the renin-angiotensin system. Some people (especially young people) experience an increase in the activity of the sympathetic nervous system.
It is clear that it is most often impossible to solve the problem with one class of drugs.
02:34
Athena Study.
More than 2,000 women in the Russian Federation were analyzed. Where hypertension was controlled, 2-component, 3-component or more drugs were more often used to treat high blood pressure.
Where there was no control (in fact, this was the majority), either these patients were not treated at all, or monotherapy was used. This is further evidence that different classes of drugs need to be combined in order to achieve blood pressure goals.
Categories of patients most likely to require combination therapy:
- persons who have a significant increase in blood pressure (above 160/100 mm Hg);
- patients with diabetes mellitus (DM);
- people who have certain lesions of organ systems. For example, kidney damage;
- left ventricular hypertrophy (LVH);
- people who smoke, are obese, have sleep disordered breathing.
Combination therapy is the key to success in achieving the goal (based on the pathogenetic mechanisms that I have already mentioned and the complications that often occur in patients).
What do we call a goal? The best evidence to date is that the goal is to achieve target blood pressure values.
In September 2010, there were some changes to the target values. Now, regardless of the degree of risk, they try to keep the pressure below 140 and 130. Up to 140 mm Hg. Art. systolic and 90 – 80 mm Hg. Art. by diastolic.
Not a single large study (probably how they were structured) has proven that a decrease of less than 130 and 80 mm Hg. Art. provides an additional reduction in morbidity and mortality. At the same time, a decrease from 130 is a very difficult moment, requiring a lot of effort and financial costs.
In persons over 80 years of age, based on data from the HYVET study, target values for systolic pressure are set at less than 150 mmHg. Art. Low numbers remain with significant proteinuria.
05:04
A meta-analysis of 147 studies in older people aged 60–69 years showed that while one standard-dose drug reduces the risk of coronary heart disease by 25% and stroke by 35%, then a combination of three drugs at half the dosage reduces the risk of developing both coronary heart disease and stroke is almost twice as high.
A very interesting analysis was published in 2009. A 2-drug combination has been shown to be 5 times more effective in lowering systolic blood pressure (SBP) than doubling the dose of either drug class. Be it beta blockers, diuretics, inhibitors, calcium antagonists. This is proof that it is combination therapy that allows you to achieve the desired values.
In addition, combination therapy can undoubtedly lead to a faster, more pronounced reduction in blood pressure.
The VALUE study clearly showed: if during the first month from the start of treatment the pressure decreases by more than 10 mm Hg. Art., then the number of fatal/non-fatal cardiovascular events, strokes and death from all causes becomes significantly less than in those people who did not achieve a reduction during the first month.
06:29
The second point that you should pay attention to: you should still strive to achieve the target numbers within 6 months. This is less than 140 mmHg. Art. Then all outcomes, including fatal events, heart attacks, strokes, deaths from all causes, and hospitalization will be significantly lower.
In my opinion, how should the decision-making process proceed when treating patients with arterial hypertension.
Certainly. We can start with monotherapy. This ensures the safety of treatment for our patients. If you see a person for the first time and you do not know what the reaction will be to antihypertensive therapy, you can start with monotherapy.
But you don’t need to go further in this vicious circle: you reached the maximum increase in dose, you became convinced that it was ineffective, you changed the drug, and so on. Patients stop this treatment, they leave the doctor.
Correct decision-making process: Tried monotherapy. We realized that it was quite effective and safe, and switched to combination therapy. We are moving further along the path of increasing doses of combination drugs. This is the principle I preach.
Plus one: the patient came - the treatment was not effective enough - the next class of drugs was added. If something else doesn’t suit you, the next class is added. Then you will be more likely to succeed.
When it comes to combination therapy, they always say: “This is polypharmacy, it is bad for patients, and so on.” Correct, because combination therapy must undoubtedly be rational.
What is rational therapy? This is when the effectiveness of treatment increases, while the incidence of side effects decreases.
This can lead to an increase in efficiency. We use different classes of drugs, influence different parts of the pathogenesis of the disease and eliminate the activation of counter-regulatory systems. If you use drugs in smaller dosages, then dose-related side effects may, of course, be reduced.
The side effects of one of the components can be eliminated by using another component.
08:51
Recommended combinations of drugs for hypertension.
Diuretics plus inhibitors or sartans. Best time to use: Where there is a high risk of heart failure.
Beta blockers and dihydropyridine calcium antagonists. When is it best to use: for ischemic heart disease.
Metabolically neutral class of drugs, sartan inhibitors, calcium antagonists. In persons at high metabolic risk.
Today, this is probably how one can imagine rational combinations. It's a diuretic plus something. Anything – these are inhibitors or sartans.
Another type of combination. Calcium antagonists plus ACE inhibitor or calcium antagonists plus sartans. Dihydropyridine calcium antagonists are used with beta blockers in patients with coronary artery disease.
Currently, the combination of diuretics plus calcium antagonists is considered irrational because this combination almost doubles the risk of myocardial infarction. Diuretics plus beta blockers had the best effect in this case.
The final picture looks like this: 1) calcium antagonists plus inhibitors or sartans and 2) diuretics, inhibitors and sartans.
The slide shows the recommended combinations of antihypertensive drugs in a trapezoid.
This trapezoid is considered the most rational today.
I took the liberty of slightly modifying the picture shown in the European recommendations. I drew a triangle. At the top I put a group of drugs that inhibit the activity of the renin-angiotensin system (RAS) plus diuretics or plus calcium antagonists. Or the three of us together in the center of the class. There will be effective treatment.
What is the rationale for saying that a combination of diuretics, inhibitors or sartans is an effective and rational combination. It is known that diuretics and inhibitors (sartans) are powerful antihypertensive drugs with pronounced organoprotective properties that can reduce the incidence of morbidity and mortality in arterial hypertension (AH).
The enhancement of the hypotensive effect is due to the fact that conditions are created for the most pronounced action of both components. The activation of counter-regulatory mechanisms is eliminated: diuretics reduce sodium levels, thereby stimulating the production of renin. This leads to a more pronounced antihypertensive effect of drugs that inhibit the activity of the angiotensin system.
At the same time, inhibitors or sartans, by reducing the production of aldosterone, reduce the excretion of potassium from the body, which is always not good when prescribing diuretics. In addition, inhibitors and sartans have a beneficial effect on purine metabolism and reduce the severity of hyperuricemia.
11:50
The combination with diuretics allows you to achieve the same reduction in blood pressure 4 weeks earlier compared to monotherapy with any of the drugs. This leads to the fact that better treatment results can be achieved.
ACE inhibitors (in general, probably the same with sartans) are drugs with pronounced organotensive properties. They influence vascular remodeling, reducing or normalizing the ratio between the lumen of blood vessels and the intima-media complex. This is very important for persistently maintaining blood pressure at normal levels and avoiding crises. The data are given for one of the long-acting ACE inhibitors - the drug Lisinopril. In our country it is often used in the form of the drug “Diroton”. Normalization of the vascular ratio in arterial hypertension.
Indicators related to heart function improve. In particular, improving the diastolic function of the heart. The ratio of peak E to peak A returns to almost normal. The time of isovolumic relaxation improves, the diameter of cardiomyocytes decreases. It is very important that myocardial fibrosis is reduced in patients with arterial hypertension. This is one of the first steps to developing a particular form of heart failure. Heart failure, which is caused by hypertension with preserved ejection fraction.
13:27
ACE inhibitors are known to work very well in obesity because the activity of the renin-angiotensin system is increased in obesity. Each fat cell produces the angiotensin gene in an amount equal to 70 liver cells.
One of the first studies that was conducted demonstrated that lisinopril was effective in approximately 60 patients. Hydrochlorothiazide (HTC) is less effective. The most important thing is that this effect is detected at doses of “Lisinopril” of 10 mg, and “Hydrochlorothiazide” - 50 mg. The side effects of Hydrochlorothiazide may already be quite pronounced.
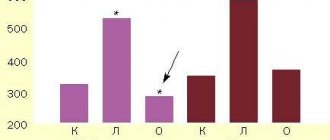
A very interesting study was conducted in Russia - the Desire study. This study showed that the use of lisinopril can normalize the abnormal daily blood pressure profile. In particular, Lisinopril in women halved the night-picker type when there is a sharp increase in blood pressure at night.
Another achievement that was shown in this study. The use of the drug in the evening allows to normalize blood pressure to a greater extent and reduce the disturbed profile. This is important because night-pickers have a higher incidence of strokes, adverse events, and so on.
Combination with diuretics. Diuretics are one of the most important classes of drugs for the treatment of arterial hypertension. Returning to the Athena study, I would like to say that the difference is in the prescription of drugs where it was ineffective: diuretics were used less often. All other classes were used approximately equally. If diuretics are not prescribed, then it is even difficult to say that something is effective or ineffective.
15:22
Two studies: UKPDS and LIFE. In the UKPDS study, the target blood pressure was 160/90 mmHg. Art. 60% of patients were already on diuretics. In the LIFE study, where the target numbers were 140/90 mmHg. Art. 90% of patients required diuretics.
In our country, the use of diuretics is somewhere around 30%. This is not a sufficient purpose. According to the LIFE study, people who received diuretic drugs had a 30-40% lower risk of various adverse events (cardiovascular death, heart attack, stroke), and a 45% lower overall mortality rate. This is a very important class of drugs that should be used in combination therapy.
I'll say it again. We can say that hypertension is resistant to treatment if a combination of three antihypertensive drugs prescribed in adequate dosages does not reduce blood pressure, but one of these drugs is a diuretic. Thus, this is a very important way to achieve target blood pressure values.
The use of ready-made combination forms is an easier path to success in treating patients with arterial hypertension.
Where hypertension was controlled, a higher percentage of cases used preformed combination dosage forms than in groups where there was no sufficient effect.
I want to show you one more study. Where a combination of Lisinopril and Hydrochlorothiazide was used (in our country, the drug Co-Diroton), patient adherence to treatment was higher than when Lisinopril and Hydrochlorothiazide were used in 2- x different tablets.
The creation of finished dosage forms follows the path of rational combinations, that is, a diuretic plus an ACE inhibitor, or a diuretic plus sartan. Or a combination based on calcium antagonists, to which inhibitors, sartans or beta blockers are added in the treatment of patients with coronary heart disease.
Now a drug has been released that contains a combination of 3 groups. This is Amlodipine plus Valsartan plus Hydrochlorothiazide. This is the right direction: when you have selected certain dosages, then you can already use ready-made combined forms.
In a nutshell about the combination of calcium antagonists with inhibitors or sartans. Calcium antagonists are good at reducing the risk of stroke, inhibitors are good at reducing the risk of myocardial infarction. This provides a reduction in the risk of major cardiovascular events.
18:14
Advantages and disadvantages of mono- and combination therapy for arterial hypertension.
Of course, if you use combination therapy, there is always a higher response rate. This is a very high possibility of dose titration, because you can take a quarter of a tablet from one package, a full tablet from another, and so on. The incidence of side effects is lower if we use rational combinations.
But it becomes difficult to accept. Patients with hypertension will not use anything that is complicated. As soon as the necessary dosages have been selected, you need to switch to fixed combinations, which has an advantage in absolutely all positions.
In conclusion, I want to say what rational combination antihypertensive therapy is. This is an impact on different parts of the pathogenesis of hypertension and elimination of the activation of counter-regulatory mechanisms. Based on this, the effectiveness of treatment increases. When it is effective, people will be more committed (commitment increases).
A good combination is a decrease in the frequency of side effects - which means an increase in adherence. Increasing adherence means increasing the effectiveness of treatment.
Let's look at the second part of this circle. Increasing efficiency, increasing adherence means decreasing cost. Any change in therapy entails, of course, an increase in the cost of treatment. And when it’s not so expensive, people will be more committed. They will better follow the doctor's orders. You should always think about this.
Thank you for your attention.
Oksana Drapkina: Thank you very much, Maria Genrikhovna.
The Recommendations retain the approach to determining the overall cardiovascular risk using SCORE, taking into account the fact that in patients with hypertension, this risk increases significantly in the presence of target organ damage associated with hypertension (especially left ventricular hypertrophy, CKD). Among the factors influencing the cardiovascular prognosis in patients with hypertension, the level of uric acid was added (more precisely, returned), early menopause, psychosocial and economic factors, and a resting heart rate of 80 beats/min or more were added. Asymptomatic target organ damage associated with hypertension includes moderate CKD with a glomerular filtration rate (GFR) <60 ml/min/1.73 m2, and severe CKD with a GFR <30 ml/min/1.73 m2 (calculated using the formula CKD-EPI), as well as severe retinopathy with hemorrhages or exudates, swelling of the optic nerve nipple. Asymptomatic kidney damage is also determined by the presence of microalbuminuria or an increased albumin/creatinine ratio in the urine. The list of established diseases of the cardiovascular system is supplemented by the presence of atherosclerotic plaques in imaging studies and atrial fibrillation.
An approach has been introduced to classify hypertension according to the stages of the disease (hypertension), taking into account the level of blood pressure, the presence of risk factors affecting the prognosis, target organ damage associated with hypertension, and comorbid conditions (Table 3).
The classification covers the range of blood pressure from high normal to grade 3 hypertension.
There are 3 stages of hypertension (hypertension). The stage of hypertension does not depend on the level of blood pressure, but is determined by the presence and severity of target organ damage.
Stage 1 (uncomplicated) - There may be other risk factors, but there is no end-organ damage. At this stage, patients with grade 3 hypertension are classified as high risk, regardless of the number of risk factors, as well as patients with grade 2 hypertension with 3 or more risk factors. The moderate-high risk category includes patients with stage 2 hypertension and 1-2 risk factors, as well as stage 1 hypertension with 3 or more risk factors. The moderate risk category includes patients with grade 1 hypertension and 1-2 risk factors, grade 2 hypertension without risk factors. Patients with high normal blood pressure and 3 or more risk factors correspond to low-moderate risk. The remaining patients were classified as low risk.
Stage 2 (asymptomatic) implies the presence of asymptomatic target organ damage associated with hypertension; CKD stage 3; DM without target organ damage and assumes the absence of symptomatic cardiovascular diseases. The state of target organs corresponding to stage 2, with high normal blood pressure, places the patient in the moderate-high risk group, with increased blood pressure of 1-2 degrees - in the high-risk category, 3 degrees - in the high-very high risk category.
Stage 3 (complicated) is determined by the presence of symptomatic cardiovascular diseases, CKD stage 4 or higher, and diabetes with target organ damage. This stage, regardless of blood pressure level, places the patient in the very high risk category.
Assessment of organ damage is recommended not only to determine risk, but also for monitoring during treatment. Changes in electro- and echocardiographic signs of left ventricular hypertrophy and GFR during treatment have a high prognostic value; moderate - dynamics of albuminuria and ankle-brachial index. Changes in the thickness of the intima-medial layer of the carotid arteries have no prognostic significance. There is insufficient data to conclude on the prognostic value of pulse wave velocity dynamics. There is no data on the significance of the dynamics of signs of left ventricular hypertrophy according to magnetic resonance imaging.
The role of statins has been emphasized to reduce cardiovascular risk, including greater risk reduction while achieving BP control. Antiplatelet therapy is indicated for secondary prevention and is not recommended for primary prevention in patients without cardiovascular disease.
Combined antihypertensive therapy: current status
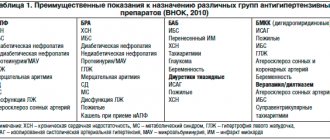
Hypertension is a hemodynamic disorder by definition, and increased peripheral vascular resistance is a distinctive hemodynamic feature of elevated blood pressure. Understanding of this fact led to the discovery and development of a special class of vasodilators with a targeted mechanism of action, although many of the previously used antihypertensive drugs also had a vasodilating effect, for example, by blocking the activity of the sympathetic nervous system. The first nonspecific vasodilator was hydralazine, followed by vasodilators blocking calcium channels of vascular smooth muscle cells (calcium antagonists - AK), postsynaptic α-adrenergic receptors of peripheral neurons of the sympathetic nervous system (α-blockers) and blockers of the renin-angiotensin-aldosterone system (RAAS) ( angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs); finally, the latest to appear are direct renin inhibitors (DRIs). The vasodilating effect is also inherent in thiazide diuretics (TD), which, by reducing the sodium content in vascular smooth muscle cells, reduce their sensitivity to vasopressors - catecholamines, etc. When using antihypertensive drugs in a heterogeneous population of patients with hypertension, the selectivity of the active substances and their other features lead to an unpredictable decrease in blood pressure in each individual patient. For example, prescribing an ACE inhibitor to a patient with hyperactivation of the RAAS due to renal artery stenosis will lead to a significant decrease in blood pressure and renal dysfunction [2]. In turn, the prescription of ACE inhibitors to elderly people and people of the black race (who in most cases have a reduced level of RAAS activity) will lead to only a slight decrease in blood pressure [3]. Most often, the “phenotype” of hypertension in a particular patient remains unspecified. A recent meta-analysis of 354 placebo-controlled studies of different antihypertensive monotherapy regimens in unselected hypertensive patients (n=56,000) showed a mean (placebo-adjusted) reduction in systolic blood pressure of 9.1 mm Hg. and diastolic blood pressure – by 5.5 mm Hg. [4]. These average values hide a wide range of individual responses to antihypertensive therapy - from a decrease in SBP by 20–30 mmHg. and until there is a complete lack of effect, and sometimes even a slight increase in blood pressure [5]. The second factor that determines the individual response to antihypertensive monotherapy is individual differences in blood pressure counter-regulation systems activated in response to a decrease in its level. In some cases, such a reaction can completely compensate for the decrease in blood pressure. Thus, the use of antihypertensive monotherapy does not always give a satisfactory result. What should be the next step in a situation like this? Should the dose be increased, the drug changed, or a combination of antihypertensive agents used? Rationale for the use of combination antihypertensive therapy The rationale for the use of combination therapy for hypertension is quite obvious. Firstly, in contrast to blindly prescribed monotherapy, a combination of drugs acting on different blood pressure regulation systems significantly increases the likelihood of its effective reduction. Secondly, prescribing a combination of drugs can be regarded as an attempt to block the activation of counter-regulatory systems that counteract the decrease in blood pressure during the use of monotherapy (Fig. 1). Thirdly, a significant part of the population of patients with hypertension suffers from so-called moderate or severe hypertension (stage 2) [6], this group includes patients with systolic blood pressure more than 160 mm Hg. and/or diastolic blood pressure more than 100 mm Hg, which is about 15–20% of all patients with hypertension. These patients are at the highest risk of cardiovascular events. Increase in blood pressure for every 20 mm Hg. doubles the risk of such events. The risk of hypertension increases with age, and the proportion of patients with stage 2 hypertension also increases. Age is also associated with an increase in the proportion of patients with isolated systolic hypertension, which causes loss of vascular elasticity and an increase in vascular resistance. Despite some differences in recommendations, in some of them combination treatment is considered first-line therapy, although only under certain conditions. Such a place for combination therapy is logical due to the risks of severe hypertension, recognition of the inevitability of using double (and sometimes triple) therapy to achieve target blood pressure values less than 140/90 mm Hg. and the need to quickly reduce blood pressure to a more acceptable level to reduce existing risks. For systolic blood pressure 20 mmHg above target and/or diastolic blood pressure 10 mmHg above target, the US Joint National Committee on the Prevention, Diagnosis and Treatment of High Blood Pressure (JNC–7) recommends start antihypertensive therapy with a combination of two drugs. Similar recommendations are contained in the latest Russian guidelines, and the recommendation for the use of first-line combination antihypertensive therapy also applies to patients with lower blood pressure levels who have multiple risk factors, target organ damage, diabetes mellitus, kidney disease or associated cardiovascular diseases [ 7]. There are concerns that the use of more than one antihypertensive drug at the beginning of treatment may in some cases provoke clinically significant hypotension and increase the risk of coronary events. Analysis of studies on the treatment of hypertension has provided some evidence of the existence of a J-shaped relationship between a decrease in blood pressure and cardiovascular risk, however, apparently, this applies to patients at high risk, including those with known coronary artery disease, when a pronounced decrease in blood pressure may lead to deterioration of myocardial perfusion [8]. Patients with uncomplicated hypertension tolerate low blood pressure values satisfactorily, as, for example, in the Systolic hypertension in Elderly study, where in the active treatment group it was possible to reduce systolic blood pressure to 60 mm Hg. [9]. Ongoing studies designed to compare initiation of antihypertensive therapy with dual and sequential monotherapy will evaluate the safety of the new approach. Fourth, compared to monotherapy, combination therapy can achieve a reduction in blood pressure variability [10]. Additional analysis of several randomized trials showed that visit-to-visit systolic BP variability is a strong and independent of mean BP predictor of myocardial infarction and stroke [18]. It is noteworthy that ACs and diuretics showed the greatest effectiveness in reducing such blood pressure variability and the risk of stroke. β-blockers, on the contrary, increased systolic blood pressure variability in a dose-dependent manner and showed the least effectiveness in preventing stroke. The addition of a calcium inhibitor or, to a lesser extent, a diuretic to a RAAS inhibitor reduces systolic blood pressure variability, which is an additional argument in support of combination therapy. Combinations of drugs There are 7 classes of antihypertensive drugs, each of which includes several representatives, so there are a large number of combinations (Table 1). Combinations will be presented below according to their division into rational (preferred), possible (acceptable) and unacceptable or ineffective. Assignment of a combination to a particular group depends on outcome data, antihypertensive efficacy, safety and tolerability. Rational (preferred) combinations RAAS inhibitors and diuretics. Currently, this combination is most often used in clinical practice. A significant number of studies with a factorial design have shown additional reductions in BP when using a combination of TD and ACEI, ARB or PIR. Diuretics reduce the volume of intravascular fluid, activate the RAAS, which inhibits the excretion of salt and water, and also counteracts vasodilation. Adding a RAAS inhibitor to a diuretic weakens the effect of this counterregulatory mechanism. In addition, the use of a diuretic can cause hypokalemia and impaired glucose tolerance, and RAAS blockers can reduce this undesirable effect. It has been shown that chlorthalidone is more effective in lowering blood pressure than hydrochlorothiazide, because has a longer duration of action, so chlorthalidone should be preferred as the second component in combination with a RAAS inhibitor. Most RAAS inhibitors are available in fixed combination with hydrochlorothiazide. A study of hypertension in elderly patients (over 80 years of age) (HYVET, Hypertension in the Very Elderly) was recently completed, which assessed the effectiveness of the thiazide-like diuretic indapamide. The ACE inhibitor perindopril was added to this diuretic to enhance the antihypertensive effect in 75% of patients. A 30% reduction in stroke and a 64% reduction in heart failure was shown with this combination compared with placebo.
Using a combination of an ACE inhibitor and a diuretic, the EPIGRAF project was carried out under the auspices of the All-Russian Scientific Society of Cardiology. This project consisted of two multicenter studies, EPIGRAPH-1 and EPIGRAPH-2. This project is valuable in that it contributed to the creation of a non-fixed combination of Enzix (“Stada”), containing two drugs in one blister - enalapril (ACE inhibitor) and indapamide (diuretic), which allows, if necessary, to change their dosages and correlate the time of administration with the circadian rhythm of blood pressure , have 2 drugs in one package, rather than using two separate ones. The drug is available in three forms: Enzix - 10 mg enalapril and 2.5 mg indapamide; Enzix Duo – 10 mg enalapril and 2.5 mg indapamide + 10 mg enalapril; Enzix Duo forte – 20 mg enalapril and 2.5 mg indapamide + 20 mg enalapril. Different dosages allow you to adjust therapy depending on the severity and risk of hypertension and drug tolerability. A study conducted in Ukraine examined the effect of long-term therapy with a non-fixed combination of enalapril and indapamide in 1 blister (Enzix, Enzix Duo) on the daily blood pressure profile and parameters of LV remodeling, its systolic and diastolic function, as well as the quality of life of patients with stable hypertension. The results of the study showed that in patients with hypertension, long-term use of a combination of enalapril and indapamide (Enzix, Enzix Duo) significantly improves the magnitude and speed of the morning rise in blood pressure and has a positive effect on blood pressure variability. Also, the data obtained indicated that long-term use of a non-fixed combination of enalapril and indapamide in 1 blister (Enzix, Enzix Duo) has a clear antihypertensive effect, leads to reverse development of LV remodeling and improvement of its diastolic function, improved quality of life along with a good safety profile and portability.
RAAS inhibitors and calcium antagonists. Combining AK with an ACE inhibitor, ARB or PIR can achieve additional reduction in blood pressure. Peripheral edema is a common dose-dependent adverse event observed with dihydropyridine CB monotherapy. The severity of this adverse effect can be reduced by adding a RAAS inhibitor to the AA. A recent meta-analysis found that ACEIs are more effective in this regard than ARBs [15]. According to the results of the ACCOMPLISH study (The Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension Trial), a fixed combination of the ACE inhibitor benazepril with the AC amlodipine is more effective in reducing morbidity and mortality than the fixed combination of an ACE inhibitor with hydrochlorothiazide [12]. Overall, ACEIs and ARBs showed similar reductions in endpoint rates, although it has been suggested that ACEIs are slightly more cardioprotective and ARBs are better at protecting against stroke. The international INVEST study compared two antihypertensive treatment regimens: verapamil, to which trandolapril was added when necessary, and atenolol, to which hydrochlorothiazide was added when necessary [16]. The study included 22,576 patients with hypertension with an established diagnosis of coronary artery disease; observation was carried out for 2.7 years. The primary composite endpoint of cardiovascular events was achieved in both groups at the same rate. Apparently, this can be explained by the fact that the disadvantages of the treatment regimen, which included a β-blocker for hypertension, were compensated by the advantages of β-blockers for coronary artery disease. b-blockers and diuretics. Not all experts consider this combination to be rational. At the same time, it has been shown that the addition of diuretics to β-blockers causes an increase in the antihypertensive effect in populations with low-renin hypertension. Although both classes of drugs have similar side effects in the form of impaired glucose tolerance, diabetes and sexual dysfunction, the actual clinical significance of “metabolic” side effects has been greatly exaggerated, and endpoint studies have shown that the use of such a combination leads to a decrease in cardiovascular morbidity and mortality [11]. Possible (acceptable) combinations: Calcium channel blockers and diuretics. Most doctors do not always combine AKs with diuretics. However, in the VALUE study (Valsartan Antihypertensive Long-term Use Evaluation Trial), hydrochlorothiazide was added to amlodipine, when it was insufficiently effective, and this combination was well tolerated by patients, although in comparison with the valsartan group, the risk of diabetes mellitus and hyperkalemia increased [13]. However, the reduction in morbidity and mortality in the amlodipine group was no less than in the valsartan group. Calcium channel blockers and β-blockers. The combination of a β-blocker with a dihydropyridine AA has an additional effect on lowering blood pressure and is generally quite well tolerated. Conversely, β-blockers should not be combined with non-dihydropyridine CBs such as verapamil and diltiazem. The combination of the negative chronotropic effect of both classes of drugs can lead to the development of bradycardia or heart block, up to complete transverse, and to the death of the patient. Double blockade of calcium channels. A recent meta-analysis showed that the combination of a dihydropyridine AA with verapamil or diltiazem leads to an additional reduction in blood pressure without a significant increase in the incidence of adverse events [17]. Such combination therapy can be used in patients with documented angioedema while taking RAAS inhibitors, as well as in patients with severe renal failure, accompanied by a risk of hyperkalemia. However, there are currently no data on long-term safety and outcomes with such therapy. Double blockade of the RAAS. The use of this combination is based on enhancing the blood pressure-lowering effect, which has been proven in a number of studies. However, the significance of this combination has diminished due to unconfirmed safety in long-term studies. In the ONTARGET study, patients receiving combination therapy with telmisartan and ramipril experienced more adverse events, and the number of cardiovascular events, despite some additional reduction in blood pressure, did not decrease compared to monotherapy. Thus, such a combination in patients at high risk of adverse events does not make much sense. However, because blockade of the RAAS by ACE inhibitors or ARBs increases plasma renin activity, the addition of a direct renin inhibitor has been suggested to be effective. A double-blind study of the combination of aliskiren and ARBs, conducted in 1797 patients, revealed a small but statistically significant decrease in blood pressure. It is noteworthy that in an open-label, prospective, crossover study of patients with resistant hypertension, the aldosterone antagonist spironolactone was more effective in lowering blood pressure than dual blockade of the RAAS [18]. The use of a combination of PIR with an ACE inhibitor or ARB in the ALTITUDE (Aliskiren Trialin Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints) study, based on the results of an interim analysis in 2012 . turned out to be inappropriate due to an increased risk of adverse events, and the study was stopped early. Apparently, it is advisable to transfer combinations of ACE inhibitors with ARBs to the group of non-recommended combinations. Unacceptable and ineffective combinations RAAS blockers and β-blockers. A combination of these classes of drugs is often used in patients who have had a myocardial infarction, as well as in patients with heart failure, because they have been shown to reduce the incidence of reinfarction and improve survival. However, this combination does not provide any additional reduction in blood pressure compared to monotherapy with these drugs. Thus, using a combination of a RAAS inhibitor and a β-blocker for the treatment of hypertension as such is inappropriate. β-blockers and drugs with central antiadrenergic action. Combining beta blockers with centrally acting antiadrenergic drugs such as clonidine provides little or no additional blood pressure reduction. Moreover, when using such a combination, reactions with an excessive increase in blood pressure were even observed [19]. Other classes of drugs in combination therapy: α-blockers and spironolactone α-adrenergic receptor antagonists are widely used as adjunctive therapy to achieve target blood pressure values. The advent of extended-release dosage forms has improved the tolerability profile of these drugs. Data from an observational analysis of the ASCOT study (the Anglo-Scandinavian Cardiac Outcomes Trial) showed that doxazosin in the gastrointestinal therapeutic system, used as third line therapy, lowers blood pressure and causes a moderate decrease in serum lipids [20 ]. In contrast to earlier data from the ALLHAT (Antihypertensive and Lipid–Lowering Treatment to Prevent Heart Attack Trial), doxazosin use in the ASCOT trial did not show an association with an increased incidence of heart failure. Therapy consisting of 4 antihypertensive drugs is often required in patients who are resistant to treatment with drugs at maximum doses or triple antihypertensive therapy, including a RAAS blocker, a calcium antagonist and a thiazide diuretic, hypertension (inability to achieve target values <140/90 mmHg). Recent reports demonstrate the effectiveness of adding spironolactone to triple therapy, reducing blood pressure by an average of 22/9.5 mmHg. Thus, spironolactone can be recommended as a component of antihypertensive therapy in patients with resistant hypertension. Adverse events. There is evidence that the severity of edema associated with the use of dihydropyridine OCs may be reduced by the addition of RAAS blockers, which may also reduce the incidence of hypokalemia caused by TDs. On the other hand, the use of β-blockers is associated with an increase in the incidence of diabetes mellitus (DM), and when using a combination of TD with β-blockers, a more significant increase in the incidence of newly diagnosed DM is likely, but paradoxically this does not increase the incidence of diabetes-related heart disease. –vascular endpoints, as shown in the ALLHAT study. The NICE recommendations provide data from a meta-analysis that revealed an increase in the incidence of newly diagnosed diabetes with the use of β-blockers and TDs in comparison with newer drugs [11]. The findings are based on the assumption that there are no differences in long-term morbidity and mortality between drugs within the same class. Among AKs, amlodipine has the largest evidence base. In studies examining ACEIs and ARBs as part of combination therapy in patients with hypertension and other cardiovascular diseases, various representatives of these classes were studied, and no differences were found between them. It is believed that among thiazide and thiazide-like diuretics, chlorthalidone in moderate doses has the greatest evidence base for long-term benefits (compared to other TDs in lower doses). Unfortunately, further studies comparing drugs in this class seem unlikely. The most frequently used β-blocker drug in trials was atenolol, and it was repeatedly stated that if other members of this class had been used in trials, the results would have been different. This seems unlikely, because The adverse events identified in the ASCOT study, which included an effect on blood pressure variability and an increase in central intra-aortic pressure compared with amlodipine (both associated with increased cardiovascular risk), most likely occur with the use of most beta-blockers [14]. . There have been no studies examining the effects of β-blocker therapy with additional pharmacological properties (eg, β-1, β-2 and α-blocker carvedilol) on long-term outcomes in patients with hypertension. Fixed-dose combinations and their benefits on prognosis A recent review of the potential benefits of fixed-dose combinations (FDCs) over corresponding drugs taken alone found that FDCs are associated with significant improvements in adherence and a small increase in duration of dosing. The degree of adherence to treatment using FDCs, according to a meta-analysis of 9 studies, is 26% higher compared to taking the same medications separately [23]. According to studies containing information on blood pressure values, the use of FDC is associated with a slight additional decrease in systolic and diastolic blood pressure (4.1 and 3.1 mm Hg, respectively) [22]. If maintained over the long term, such differences in blood pressure may translate into real benefits in cardiovascular outcomes. Conclusion The majority of patients with hypertension require treatment with two or more drugs from different classes of antihypertensive drugs to achieve target blood pressure values. Combination antihypertensive therapy should be prescribed to patients with blood pressure above target values by more than 20/10 mmHg. Rational (preferred) and possible (acceptable) combinations of drugs should be used. Fixed combinations increase adherence to therapy, which increases the frequency of achieving target blood pressure values.
References 1. Page IH The MOSAIC theory // Hypertension Mechanisms. – New York: Grune and Stratton, 1987. P. 910–923. 2. Mimran A., Ribstein J., Du Cailar G. Converting enzyme inhibitors and renal function in essential and renovascular hypertension // Am. J. Hypertens. 1991. Vol. 4 (Suppl. 1). 7S–14S. 3. Dickerson JE, Hingorani AD, Ashby MJ et al. Optimization of antihypertensive treatment by cross–over rotation of four major classes // Lancet. 1999. Vol. 353. P. 2008–2013. 4. Law MR, Wald NJ, Morris JK, Jordan RE Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomized trials // BMJ. 2003. Vol. 326. P. 1427–1435. 5. Attwood S., Bird R., Burch K. et al. Within–patient correlation between the antihypertensive effects of atenolol, lisinoprill and nifedepin // Hypertens. 1994. Vol. 12. P. 1053–1060. 6. Chobanian AV, Bakris GL, Black HR et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh Report of the joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure // Hypertens. 2003. Vol. 42. P. 1206–1252. 7. Russian Medical Society for Arterial Hypertension (RMAS), All-Russian Scientific Society of Cardiologists (VNOK). Diagnosis and treatment of arterial hypertension. Russian recommendations (fourth revision) // Systemic hypertension. – 2010. – No. 3. – P. 5–26. 8. Messerli FH, Mancia G, Conti CR et al. Dogma disputed: can aggressively lower blood pressure in hypertensive patients with artery disease be dangerous? //Ann. Intern. Med. 2006. Vol. 144. P. 884–894. 9. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP) // JAMA. 1991. Vol. 265. P. 3255–3264. 10. Rothwell PM, Howard SC, Dolan E. et al. Prognostic significance of visit–to–visit variability, maximum systolic blood pressure, and episodic hypertension // Lancet. 2010. Vol. 375. P. 895–905. 11. Nice guidelines. Management of hypertension in adults in primary care. 2007. www.nice.org.uk. 12. Jamerson K, Weber MA, Bakris GL et al. ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients /// NEJM. 2008.Vol. 359. P. 2417–2428. 13. Julius S., Kjeldsen SE, Brunner H. et al. VALUE Trial. VALUE trial: Long–term blood pressure trends in 13,449 patients with hypertension and high cardiovascular risk // Am. J. Hypertens. 2003. Vol. 7. P. 544–548. 14. Williams B, Lacy PS, Thom SM et al. CAFE Investigators; Anglo–Scandinavian Cardiac Outcomes Trial Investigators; CAFE Steering Committee and Writing Committee. Differential impact of blood pressure–lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study // Circulation. 2006. Vol. 113. P. 1213–1225. 15. Makani H., Bangalore S., Romero J. et al. Effect of rennin–angiotensin–system blockade on calcium channel blockers associated peripheral edema // Am. J. Med. 2011. Vol. 124. P. 128–135. 16. Pepine CJ, Handberg EM, Cooper–DeHoff RM et al. INVEST Investigators. A calcium antagonist vs. a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil–Trandolapril Study (INVEST): a randomized controlled trial // JAMA. 2003. Vol. 290. P. 2805–2819. 17. Alviar CL, Devarapally S, Romero J. et al. Efficacy and Safety of Dual Calcium Channel Blocker Therapy for the Treatment of Hypertension: A Meta-analysis // ASH. 2010. 18. Alvares–Alvares B. Management of resistant arterial hypertension: role of spironolactone versus double blockade of the rennin–angiotensin–aldosterone system // J. Hypertens. 2010. Jul 21. . 19. Bailey RR, Neale TJ Rapid clonidine withdrawal with blood pressure overshoot exaggerated by beta-blockade // BMJ. 1976. Vol. 6015. P. 942–943. 20. Chapman N., Chang CL, Dahlof B. et al. For the ASCOT Investigators. Effect of doxazosin gastrointestinal therapeutic system as third–line antihypertensive therapy on blood pressure and lipids in the Anglo–Scandinavian Cardiac Outcomes Trial // Circulation. 2008. Vol. 118. P. 42–48. 21. Chapman N., Dobson J., Wilson S. et al. On behalf of the ASCOT Trial Investigators. Effect of spironolactone on blood pressure in subjects with resistant hypertension // Hypertens. 2007. Vol. 49. P. 839–845. 22. Gupta AK, Arshad S., Poulter NR Compliance, safety and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis // Hypertens. 2010. Vol. 55. P. 399–407. 23. Bangalore S., Kamalakkannan G., Parkar S., Messerli FH Fixed-dose combinations improve medication compliance: a meta-analysis // Am. J. Med. 2007. Vol. 120. P. 713–719.
Complex therapy of arterial hypertension
“Arterial hypertension” (AH) refers to the syndrome of increased blood pressure (BP). A distinction is made between primary hypertension (“hypertension”—GB) and secondary (“symptomatic” hypertension).
Hypertension is usually understood as a chronic disease, the main manifestation of which is a persistent increase in blood pressure, not associated with the presence of pathological processes in which the increase in blood pressure is caused by known, often remediable causes of “symptomatic” hypertension in modern conditions. Due to the fact that hypertension is a heterogeneous disease that has quite distinct clinical and pathogenetic variants with significantly different development mechanisms at the initial stages, hypertension is often used in the scientific literature instead of designating hypertension.
It is well known that hypertension is the most common cardiovascular disease, dangerous primarily due to its complications. Data from a number of large epidemiological studies clearly indicate that the risk of developing coronary heart disease (CHD), cerebral stroke, heart failure, and peripheral arterial diseases in the population increases significantly (sometimes several times) in individuals with elevated blood pressure compared to individuals with normal blood pressure. HELL.
The prevalence of hypertension is very high in any developed country in the world. Russia, unfortunately, is no exception in this regard. A study by S. A. Shalnova and others showed that among the adult population of Russia, 39.3% of men and 41.1% of women suffer from hypertension (Table 1).
The high prevalence of hypertension in Russia is largely the reason for the extremely high mortality rates in our country. According to the information contained in the Demographic Yearbook of Russia, in 2001, 1,253,103 people died from diseases of the circulatory system, including 475,163 people from cerebrovascular diseases (for comparison: 294,063 people died from cancer in 2001) .
Hypertension plays a special role in the pathogenesis of all types of cerebral stroke. It is believed to be the underlying cause in about 70% of cases of this disease. The Framingham Study demonstrated that the age-standardized risk of stroke among patients with hypertension (systolic blood pressure above 160 mm Hg and/or diastolic blood pressure above 95 mm Hg) was 3.1 for men and 2.1 for men. 9 for women. There is a fairly clear direct and statistically significant connection between mortality from cerebral stroke and the prevalence of hypertension in a particular country (correlation coefficient 0.78).
It can be said without exaggeration that mortality from cerebrovascular diseases in our country has become catastrophic. Thus, in data on cardiovascular mortality in various countries of the world recently published in the journal Heart (in total, data are provided for 48 countries from different parts of the world), Russia consistently ranked first in the number of deaths from cerebrovascular diseases among both men and women. Moreover, the absolute mortality rates in Russia are several times higher than in other countries. So, in 1995–1998. The age-standardized mortality rate from cerebrovascular diseases in men in Russia was 203.5 cases per 100,000 people, while in the USA it was 29.3, and in Canada it was 27.8.
All modern recommendations for the treatment of hypertension clearly define the main goal of therapy as reducing cardiovascular and renal morbidity and mortality. To achieve this goal, first of all, it is necessary to reduce blood pressure to a normal level, as well as correct all modifiable risk factors: smoking, dyslipidemia, hyperglycemia, obesity - and treatment of concomitant diseases: diabetes mellitus, etc.
Reduction of systolic and diastolic blood pressure to <140/90 mm Hg. Art. helps reduce the likelihood of developing cardiovascular complications. This has been clearly demonstrated by some studies, in particular MRFIT (Fig. 1). That is why the target blood pressure level for the treatment of hypertension is considered <140/90 mmHg. Art. Data from a number of recent studies indicate that if therapy is well tolerated, it is advisable to achieve a reduction in blood pressure to certain values, but not lower than 110/70 mm Hg. Art. In patients with hypertension and diabetes mellitus or kidney disease, the target blood pressure is <130/80 mmHg. Art.
The need to lower blood pressure can be convincingly illustrated by the fact that over the past 20 years, the implementation of a set of measures to combat hypertension in the United States has led to the disappearance of malignant hypertension, a reduction in mortality from cerebral stroke by 60%, and a 2-fold reduction in cardiovascular mortality.
Ways to achieve target blood pressure levels
Non-medicinal. Lifestyle changes are recommended for all patients with hypertension, including those receiving drug therapy, especially in the presence of risk factors. These measures include: quitting smoking, normalizing body weight (body mass index < 25 kg/m2), reducing alcohol consumption < 30 g/day in men and < 20 g/day in women, regular dynamic physical activity of 30– 40 minutes at least 4 times a week, reducing the consumption of table salt to 5 g/day, changing the diet with increasing the consumption of plant foods, reducing the consumption of animal fats, including foods rich in potassium, calcium (vegetables, fruits, grains) and magnesium (dairy products).
The recently completed Oxford Fruit and Vegetable Study and TOHP-II further clearly demonstrated the effect of a diet high in fruits and vegetables on blood pressure levels. The Oxford Fruit and Vegetable Study included 670 individuals with normal blood pressure. Everyone in the study group was required to follow a diet enriched with vegetables and fruits, while the control group was not given any dietary recommendations. The observation period was 6 months. Daily consumption of vegetables and fruits in the main group increased by 112 g, in the control group - by 8 g. Compliance with the diet was associated with a decrease in systolic blood pressure by an average of 2.0 mm Hg. Art., and diastolic - by 1.6 mm Hg. Art. (p < 0.05), while in the control group the first indicator increased by 1.4 mm Hg. Art., and the decrease in diastolic blood pressure was only 0.3 mm Hg. Art. However, no dynamics associated with cholesterol levels were noted in any of the groups.
Drug therapy. The main indication for prescribing antihypertensive therapy is the degree of cardiovascular risk (Table 2).
For grade I and II hypertension in patients with a high or very high risk of developing cardiovascular complications, antihypertensive drugs should be prescribed immediately. With a moderate risk, observation for 3 months with regular blood pressure monitoring is acceptable before deciding to start therapy. Treatment is prescribed for a sustained increase in blood pressure > 140/90 mmHg. Art.
In the low-risk group, a 3- to 12-month observation period and non-pharmacologic therapy are recommended before initiating drug treatment. The indication for starting such treatment is a stable blood pressure level in the range of 140–159/90–99 mmHg. Art.
In case of grade III hypertension, antihypertensive drug therapy should be immediately prescribed.
In addition to therapy with antihypertensive drugs, patients at high risk of cardiovascular complications are prescribed therapy aimed at preventing other risk factors, primarily impaired lipid metabolism. Reducing the risk of complications is achieved by prescribing anticoagulants, primarily acetylsalicylic acid.
Main groups of antihypertensive drugs
In the Russian recommendations for the treatment of hypertension, the second revision, presented at the Russian National Congress of Cardiologists in 2005, the group of drugs recommended for the treatment of hypertension, in addition to diuretics, β-blockers, calcium antagonists (CA), angiotensin-converting enzyme inhibitors (ACE inhibitors), receptor blockers angiotensin I (ARB), α-blockers, I1-imidazoline receptor agonists (AIR) are included. The latter play a certain role in the treatment of patients with metabolic syndrome and diabetes mellitus; it is noted that they can be prescribed as monotherapy or in combination with other antihypertensive drugs if other drugs are ineffective.
Monotherapy or combination therapy
When choosing between monotherapy and combination therapy, the doctor should focus primarily on the initial level of blood pressure, the presence of complications or their absence. Based on the results of multicenter international studies, it can be assumed that monotherapy will be effective mainly in patients with stage I hypertension. Thus, according to the ALLHAT study, monotherapy was effective in only 60% of patients with stage I and II hypertension; in the HOT study, only 25–50% of patients with stage I and III hypertension remained on monotherapy: in studies that included patients with diabetes, the vast majority of patients received at least two drugs, whereas in diabetic nephropathy, to achieve the target blood pressure level on average, two to three drugs were required in addition to basic therapy.
In accordance with the initial blood pressure level, the presence of complications and risk factors, it is advisable to start therapy with either a low dose of one drug or a low-dose combination.
The advantage of monotherapy is that if treatment is ineffective at the initial stage, the doctor can either change the class of the drug or increase the dose of the previously taken drug, this will make it possible to select the drug individually for each patient. However, in most cases, such a procedure is labor-intensive, in addition, it often leads to a loss of trust not only in the therapy being performed, but also in the attending physician, which, in turn, does not contribute to increasing compliance.
An obvious disadvantage of a treatment regimen that involves starting treatment with two drugs at once, even in low doses, is the danger of prescribing an “unnecessary” drug to the patient. However, combination therapy still has more advantages: firstly, the use of drugs with different mechanisms of action makes it possible to more effectively control hypertension and its complications; secondly, when using combination therapy, it becomes possible to prescribe drugs in low doses, while reducing the likelihood of developing undesirable effects; thirdly, fixed drug combinations have now become available, allowing two drugs to be prescribed in one tablet, which significantly increases compliance.
Currently, the following combinations of drugs are considered effective and safe: ACE inhibitors + diuretics; diuretics + β-blockers; diuretics + ARBs; calcium antagonists (CA) (dihydropyridine) + β-blockers; AA (dihydropyridine) + ARB; AA + ACEI; AA (dihydropyridine) + diuretics; α-blockers + β-blocker (Fig. 2).
| Figure 2. Possible combinations of different classes of antihypertensive drugs. (From European guidelines for the treatment of hypertension) |
Guided by numerous studies demonstrating the positive effects of individual drug combinations on endpoints, leading pharmaceutical companies began to offer combination antihypertensive drugs. Thus, in recent years, combinations of long-acting drugs with fixed dosages have appeared on the pharmacological market: diuretic + ARB (co-diovan, gizaar); ACE inhibitor + diuretic (co-renitec, noliprel, renipril GT); AK (dihydropyridine) + β-blocker (Lomax); diuretic + β-blocker (atehexal compositum); today the only combination of AK + ACEI (Tarka).
The question of the benefits of using one or another group of antihypertensive drugs, one or another combination is quite complex and ambiguous, however, the results of multicenter randomized studies generally prove that the appointment of any of the existing treatment regimens for hypertension reduces the overall risk of cardiovascular events, and the lower the blood pressure , the lower the above-mentioned risk.
In all cases, it is recommended to use long-acting drugs that provide an effect throughout the day; this reduces blood pressure variability and, possibly, provides better organ protection and a reduction in the number of cardiovascular complications. In addition, due to the convenience of a single dose of drugs, patient adherence to treatment increases.
Modern international recommendations for the treatment of hypertension clearly define when and which drugs the doctor should give preference to. The main argument in favor of prescribing a specific group of drugs are the so-called additional indications. Thus, additional indications for the prescription of dihydropyridine ACs are old age, isolated systolic hypertension, the presence of angina pectoris, atherosclerosis of the peripheral arteries, in particular atherosclerosis of the carotid arteries. Pulse-lowering non-dihydropyridine AKs, diltiazem and verapamil-SR, are advisable to use in patients with supraventricular tachycardia. It has been proven that ARBs slow down the progression of chronic renal failure in hypertension in combination with diabetes mellitus, and also ensure the reverse development of left ventricular hypertrophy. An aldosterone receptor blocker (spironolactone) has been effective in patients with chronic heart failure and patients who have had myocardial infarction.
All these additional indications arise from the results of specific controlled studies that have demonstrated the benefits of dihydropyridine AKs in these categories of patients. It should be remembered that dihydropyridine AKs are one of the few groups of drugs that a doctor can prescribe to pregnant women with hypertension.
When selecting therapy for hypertension, practicing physicians do not always follow international recommendations and often determine treatment priorities themselves. Interestingly, AKs are the most commonly prescribed drugs worldwide: the AK market accounts for about 35%, which is significantly larger than that of other groups of antihypertensive drugs; Thus, the market for ACEIs and ARBs combined accounts for only 39% of the global market (16 and 23%, respectively). In Russia, the situation is fundamentally different: in terms of frequency of use, ACEIs and ARBs confidently lead, occupying 47% of the market, while ACs account for only 13.9%, which practically coincides with the frequency of use of diuretics. However, what is even more alarming is the fact that we are still mainly prescribing first-generation AKs, regular treatment of which, as noted in a number of studies, cannot be considered either sufficiently effective or safe. A striking example of this is the analysis of the sales structure of AKs in one of the pharmacies in the center of Moscow, carried out in the second quarter of 2003, which showed that 48% of sales of all dihydropyridine AKs still account for short-acting first-generation drugs.
Speaking about the effectiveness and safety of long-term use of antihypertensive drugs used for the treatment of hypertension, it is necessary to recall that all large studies examining the effect on “endpoints” have been and are being conducted only with original drugs. The only drawback of original drugs is their high cost, which often limits the possibilities of complex therapy. The creation of generics - copies of original drugs - significantly reduces the cost of treatment, but raises the problem of assessing the equivalence of generics to original drugs. Today, about 60 generics of enalapril, about 30 generics of amlodipine, more than 10 generics of indapamide are registered in Russia, and recently the first generic fosinopril, bioequivalent to the original drug, has appeared
It is clear that it is difficult for a practicing physician to understand such a variety of drugs, especially since manufacturing companies in most cases do not provide data on pharmaceutical and pharmacokinetic equivalence to the original drug. Familiarization of doctors with such data could significantly ease the problem of choosing a drug. In the absence of such information, specialists can only rely on personal experience, as well as the results of a few clinical studies comparing original drugs and generics or different generics with each other.
Literature
- Shalnova S. A., Deev A. D., Vikhireva O. V. et al. Prevalence of arterial hypertension in Russia. Awareness, treatment, control // Disease prevention and health promotion. 2001. No. 2. P. 3–7.
- Demographic Yearbook of Russia - 2002. M., 2002.
- D'Agostinio RB, Wolf PA, Belanger AJ, Kannel WB Stroke risk profile: adjustment for antihypertensive medication: the Framingham Study//Stroke. 1994; 25:40–43.
- Mancia G. Prevention and treatment of stroke in patients with hypertension//Clin. Therapeutics. 2004; 26:631–648.
- Levi F., Lucchini F., Negri E., La Vecchia C. Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world//Heart. 2002; 88: 119–124.
- Opie LH, Schall R. Evidence-based evaluation of calcium channel blockers for hypertension: equality of mortality and cardiovascular risk relative to conventional therapy//J. Am. Coll. Cardiol. 2002; 16: 39 (2): 315-22. Erratum in: J. Am. Coll. Cardiol. 2002; 17:39(8):1409–1410.
- Staesssen J., Ji-Guang Wang, Thijs L. Calcium-channel blockade and cardiovascular prognosis: recent evidence from clinical outcome trials // Am. J. Hypertens. 2002; 15:85–93.
- Poole-Wilson P., Lubsen J., Kirwan B. et al. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): a randomized controlled trial//Lancet. 2004; 364:849–857.
- Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension//J. Hypertension. 2003; 21: 1011–1053.
- Martsevich S. Yu., Kutishenko N. P., Dmitrieva N. A. The problem of choosing a drug in the treatment of arterial hypertension // Cardiovascular therapy and prevention. 2004. No. 3.
- VNOK Expert Committee. Prevention, diagnosis and treatment of arterial hypertension. Russian recommendations (second revision) // appendix to the railway. "Cardiovascular therapy and prevention." 2004.
- Schrader J., Luders S., Kulschewski A. et al. MOSES Study Group. Morbidity and Mortality After Stroke, Eprosartan Compared with Nitrendipine for Secondary Prevention: principal results of a prospective randomized controlled study (MOSES)//Stroke. 2005; 36(6):1218–1226.
V. A. Egorov Yu. E. Semenova, Candidate of Medical Sciences Yu. V. Lukina, Candidate of Medical Sciences State Research Center for Preventive Medicine, Moscow