What is this?
The symptoms and treatment of kidney pressure depend on many factors. Even young people are susceptible to this pathology. Only a doctor can find out the cause and eliminate the disease itself; it will not be possible to cope with the situation on your own.
Arterial hypertension is considered one of the most common ailments, but few people know that the kidneys are often involved in the occurrence of the disease. Malfunctions of this organ directly affect blood pressure. Doctors call this disease “renal hypertension.” The relationship between kidneys and blood pressure is very close. The job of the kidney is to regulate fluid levels in the body, as well as remove harmful and toxic substances from the body. If the kidneys do not do their job well, pressure increases in the circulatory system.
In addition, renal pressure may be below normal, which also indicates the presence of pathology in this area of the body. In this case, the water level in the body is below normal, and a mild degree of dehydration is observed.
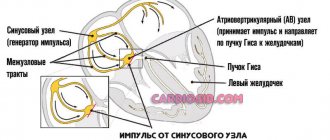
Renal hypertension is not considered an independent disease. This condition develops under the influence of certain pathological factors that have a destructive effect on the kidneys. This situation provokes a malfunction of the organ, as a result of which there is a decrease in blood flow, sodium and water retention in the kidneys, resulting in swelling. The accumulation of sodium ions leads to swelling of the vascular walls, increasing their sensitivity.
For this reason, the organ's receptors actively produce an enzyme called renin. After certain pathological transformations, this substance affects the tone of blood vessels, reducing their patency, which will inevitably lead to an increase in pressure in this area.
Treatment for renal hypertension depends on the type of the disease. With one course, medications can help, but with another, only surgical intervention is necessary.
Classification of renal hypertension:
- Parenchymatous. Appears as a consequence of nephrogenic pathologies that cause damage to the vascular tissue of the kidney parenchyma, as well as the glomeruli of the organ.
- Vasorenal. It occurs when the arteries of the kidneys are destroyed, which causes poor blood supply to the area. It can be acquired and congenital.
- Mixed. It is diagnosed by a combination of the first two types of pathology and is considered the most dangerous form of the disease.
Half of the patients have parenchymal renal hypertension; this type of disease is the most common. The consequence of this disease can also be its progression, as a result of which the tissue of the kidney itself dies, and substances that regulate vascular tone are synthesized in smaller quantities. However, more often this development of the situation concerns elderly and senile people.
Hypertension and kidney disease
Let us dwell on the second variant of arterial hypertension as concomitant, secondary to kidney disease, or as a symptom of kidney disease. In the general population of people with high blood pressure, such hypertension is represented in less than 10% of cases. Such hypertension is divided into two parts: associated with the pathology of the large vessels of the kidneys, and associated with the kidney tissue itself. Speaking about the first option, we highlight renovascular hypertension, namely hypertension associated with decreased blood flow in the renal arteries.
This condition can be either congenital, which is more typical for patients with “young”, early hypertension, or acquired. The more common acquired pathology is, first of all, atherosclerosis of the renal arteries by analogy with the coronary arteries: plaque - stenosis - decreased blood circulation, in the case of the kidney - the entire organ. The kidney responds to “insufficient nutrition” by producing substances that increase blood pressure (BP). If a person already has arterial hypertension, it will become more severe, and medications will no longer help. Here we need to think about what caused the severity of hypertension. Laboratory tests come to the aid of the doctor and the patient, revealing a decrease in the function of a kidney suffering from insufficient blood supply, in which the processes of sclerosis develop - that is, the replacement of active kidney tissue with an analogue of scar tissue that does not fulfill the tasks assigned to this important organ. The way out of this situation is to find and confirm the cause of decreased blood circulation and apply surgical or conservative treatment of renovascular hypertension. To some extent, timely detected renovascular hypertension is more positive, since by eliminating the cause, we can hope for a favorable course of the disease, if not with a complete recovery, then with a significant improvement.
Causes
The causes of this disease directly affect the therapy that the doctor chooses. Without eliminating provoking factors, it will not be possible to improve the prognosis of such patients.
Why does it occur:
- Inflammatory pathologies (pyelonephritis, glomerulonephritis).
- Anomalies in the development of the organ and urinary tract, of congenital origin (hydronephrosis, polycystic disease, kidney dystopia and others).
- Diabetes mellitus, in which the microcirculatory system of the organ is damaged.
- Systemic diseases that cause kidney damage (SLE - systemic lupus erythematosus, vasculitis).
- Atherosclerotic changes in the organ, narrowing of the arteries of the kidney, congenital or acquired.
- Large stones in the kidneys and urinary tract, tumor processes in this area.
Narrowing of the arteries leads to increased pressure in the organ, since insufficient volumes of blood are delivered. If such a problem occurs, the kidneys begin to store water, which increases the amount of circulating blood, and hence an increase in pressure. Stenosis of the renal vessels and arteries often provokes the appearance of atherosclerosis, and this directly affects the patency of the coronary arteries, so a heart attack can be a consequence of such a pathology.
Treatment of hypertension
Treatment of almost any hypertension, whether essential or secondary, is always long-term, often lifelong. Considerable time may pass from the onset of the disease to diagnosis. And this time without treatment is time lost for the human body. The very fact of increased blood pressure contributes to the development of pathological processes in the heart and vascular wall. This is why it is so important to start drug therapy early, no matter what the cause of hypertension. Patients often avoid taking pills that they feel are unjustified. In the case of arterial hypertension, treatment at any stage of the disease is justified. This is especially true for patients with kidney disease. The speculative opposition to “pill chemistry” is countered by the possibility of living longer, and without heart attack, stroke due to renal failure, or retinal detachment.
However, it is worth emphasizing the possibilities of non-drug effects on hypertension. Significant weight loss, regular physical activity (walking, cycling, fitness, outdoor games) sometimes bring enormous success, allowing you to reduce drug doses and, in especially successful cases, abandon drug therapy. This applies primarily to patients with “young” essential hypertension.
Symptoms
Manifestations of renal hypertension are not always noticeable, especially if the disease is in the first stage of its development. Sometimes a person may feel minor ailments, but does not associate them with an illness. When blood pressure readings begin to rise significantly, the symptoms also become more pronounced. This:
- Dizziness.
- Head pain, frequent migraines.
- Excessive sweating.
- Pain in the lumbar region.
- Increased body temperature.
- Tachycardia.
- Increased fatigue, loss of strength, weakness.
- Frequent urge to urinate.
- Double the volume of urine excreted.
The main symptom of this pathology is a constant increase in blood pressure, which is almost impossible to bring down completely. The drugs usually prescribed for hypertension do not help much. Therefore, the doctor raises the question of kidney pressure.
When, under the influence of this disease, the kidney tissue is significantly destroyed, more severe symptoms may appear: clouding and loss of consciousness, disruptions in the functioning of the gastrointestinal tract, diarrhea, vomiting. Among other things, hemorrhages in the retina of the eyes are often observed, which can lead to serious visual impairment. All signs of increased renal pressure are similar to the manifestations of arterial hypertension, so it is important for a doctor to correctly diagnose the disease.
Diagnostics
In most cases, patients complain of high blood pressure. If the condition is accompanied by lesions of the renal parenchyma or its vessels, the doctor raises the question of the renovascular nature of the disorder. For diagnosis, the specialist prescribes the following studies:
- clinical blood test;
- general urine analysis;
- blood biochemistry;
- Reberg's test;
- excretory urography;
- Ultrasound of the kidneys;
- Dopplerography of renal vessels;
- arteriography and aortography of the renal vessels;
- spiral CT or MRI.
If kidney cancer is suspected, the specialist will insist on a biopsy and histological examination.
Types of renal arterial hypertension
The causes of hypertension associated with renal pathologies may be a narrowing of the lumen of the renal artery and problems with the outflow of urine that arise from urolithiasis or due to inflammatory processes in the kidneys.
Based on the causes of development, renal arterial hypertension can be:
- Renoparenchymatous – with damage to kidney tissue;
- Vasorenal – with damage to the renal arteries;
- Mixed – with combined lesions.
Basically, the disease progresses due to narrowing of the artery through which blood flows to the kidneys. This mechanism is often found in older people; it is a consequence of the formation of atherosclerotic plaques.
Association between hypertension and CKD
Arterial hypertension and CKD have close and complex relationships with each other. Hypertension is often considered both a cause and a consequence of chronic kidney disease. It is widespread and rarely controlled. The complex interaction of these dangerous pathologies with each other provokes unfavorable outcomes of diseases of the heart, blood vessels and brain.
The pathophysiological mechanisms of increased pressure in renal pathology are complex and are the consequences of many factors such as:
- decrease in kidney cell mass;
- delays in sodium excretion from the body;
- increased activity of the sympathetic nervous system;
- increase in extracellular volume;
- activation of hormonal activity.
Patients with CKD often have high blood pressure with high risks. Hypertension may have:
- hidden form;
- resistant course.
Sometimes it occurs at night.
Hypertension and CKD should be carefully studied to slow the development of cardiac and renal dysfunction.
Stages of the disease
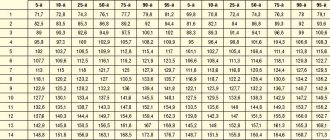
Normal blood pressure is 120/80 mm Hg. Increasing the indicator to 139/89 mm Hg. is considered as a borderline condition, and the pressure is above 140/90 mm Hg. is a sign of arterial hypertension. It is worth noting that the first number indicates the degree of pressure in the arteries when blood is pushed into them during contraction of the heart muscle. The second number refers to the pressure at the moment the heart relaxes.
The degree of chronic renal failure is assessed by glomerular filtration rate (GFR):
- Zero degree – GFR ˃ 90 ml/min;
- Grade I – GFR 60–89 ml/min;
- Grade II – GFR 30–59 ml/min;
- III degree – GFR 15–30 ml/min;
- IV degree – GFR ˂ 15 ml/min.
In addition, there are 4 stages of the disease based on clinical manifestations. The latent stage is the stage at which the disease does not manifest itself in any way. This is followed by the compensated and intermittent stages. The terminal stage is characterized by irreversible changes.
Problems of chronic kidney disease
Now CKD represents a real epidemiological problem, since the number of patients suffering from it is increasing. Prolonged and recurrent course of the disease leads to the development of end-stage renal failure, resulting in huge costs for the healthcare system.
As kidney function gradually decreases, arterial hypertension also increases, which, as a rule, always accompanies CKD.
Hypertension is an equally serious medical problem, since it is the main cause of the development of:
- all types of strokes;
- pathologies of the heart and blood vessels.
In this case, chronic kidney disease can act both as a cause of arterial hypertension and as its complication if the disease proceeds uncontrolled.
The prevalence of hypertension and CKD among adult patients looks something like this:
- AH - from 25 to 30%;
- CKD - about 15%.
If a person already suffers from chronic kidney disease, he is also diagnosed with arterial hypertension. Conducted epidemiological studies indicate that from 67 to 71% of patients suffer from hypertension, and the percentage of elderly people makes up 82% of the total number of clinical cases. When CKD progresses to the later stages of its course, hypertension is observed in 90% of patients.
When a patient is on dialysis, the frequency of hypertension changes, since the methods of controlling blood pressure are different (pre-, post-dialysis, outpatient, etc.). However, research shows that hypertension affects:
- from 50 to 80% percent of patients undergoing hemodialysis;
- about 30% of those undergoing peritoneal dialysis.
It has been said many times that arterial hypertension can be both a cause and a result of the development of chronic kidney disease.
The prevalence, severity level and ability to control the disease are influenced by:
- causes of renal pathology;
- albumin level in urine;
- hereditary factor;
- socioeconomic reasons.
Ethnic and racial factors should also be taken into account.
Treatment of renal arterial hypertension
The treatment strategy for renal arterial hypertension is developed taking into account the causes of the disease, its duration, symptoms, and the presence of other chronic diseases in the person. The key role is played by the treatment of kidney disease, which is the main pathology.
Particular attention is paid to normalizing blood pressure. To do this, it is recommended to adhere to the optimal combination of work and rest, do not forget about physical activity, lose excess weight, balance the diet by removing foods high in salt and cholesterol, and also reduce alcohol consumption to a minimum.
Symptoms indicating kidney pressure
- Weakening the effect of antihypertensive drugs . The medications that patients previously took for blood pressure stop working.
- Nocturia is an increase in urine production at night. Sometimes patients get up to go to the toilet several times a night. Lack of proper sleep leads to headaches and heart problems.
- Swelling that appears in the morning . At the beginning of the disease, swelling decreases during the day or even disappears completely. When kidney function deteriorates, this condition persists permanently. Renal edema is loose, so after pressing with a finger, a hole remains that does not disappear for a long time. Fluid excretion worsens after consuming salty, smoked and alcoholic foods.
- Decreased amount of urine excreted . Patients feel a false urge that is not accompanied by urination.
If measures are not taken, renal failure will develop, which will “tie” the patient to a hemodialysis machine (artificial kidney).
Blood pressure control and its targets
Despite the high level of awareness of patients with CKD about hypertension, it is not always possible to control blood pressure. For diagnostic purposes, blood pressure is most often measured either randomly or in an outpatient setting. Thanks to ambulatory blood pressure measurement, it is possible to further evaluate its variability during the day. Unfortunately, not all patients with CKD regularly monitor their blood pressure; therefore, from 30 to 60% of patients cannot achieve its target values. It is their target organs that may be damaged in the future.
Thus, regular blood pressure monitoring ensures:
- reducing the risk of complications from the heart and blood vessels;
- reduced risk of cerebral complications;
- reduction in mortality rate;
- prevention of irreversible processes associated with kidney failure.
The optimal blood pressure values for people suffering from chronic kidney disease still remain controversial among specialists, despite the fact that clinical studies have already made it possible to give specific and clear recommendations:
- upper “digits” of blood pressure - 140/90 (albuminuria - less than 30 g daily);
- 130/80 (albuminuria - more than 30 mg daily).
For patients with CKD and a high level of cardiovascular risk, the optimal target blood pressure for them is 130/80.