Vasorenal hypertension (also vasorenal arterial hypertension , renovascular hypertension ) is a fairly common syndrome of high blood pressure among all age groups of both sexes, caused in most cases by disturbances of normal blood flow in the renal arteries (renal ischemia).
The processes of arterial stenosis due to atherosclerosis or fibromuscular dysplasia, arteriovenous fistulas, nonspecific aortoarteritis, thromboembolism and other diseases, complicating the normal flow of blood through the renal arteries, prevent the enzyme renin, secreted by the kidneys, from entering the arteries. This enzyme is responsible for regulating blood pressure; a decrease in its amount in the blood leads to hypertension.
Caused by hereditary or acquired arterial diseases, renovascular hypertension is usually very resistant to the effects of drugs and is usually permanent. Based on this collective characteristic, it can be distinguished from other types of arterial hypertension (high blood pressure).
1
Ultrasound in MedicCity
2 Consultation with a phlebologist in MedicCity
3 Vascular surgery in MedicCity
Regular examination by a phlebologist or vascular surgeon will help you avoid serious complications if vascular pathology is detected. Delay in treating vascular diseases is life-threatening! Trust your health to the MedicCity professionals!
Causes
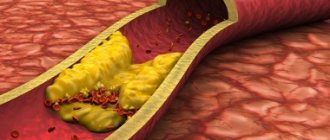
- A common cause of renovascular arterial hypertension is plaque in the arteries - atherosclerosis. Cholesterol plaques accumulate in the main vessels, preventing normal blood flow or completely blocking it. The separated fragments form blood clots, which cause arterial stenosis. As a result, the kidney tissue experiences oxygen deficiency and ischemia develops in them.
- Contributing to renovascular hypertension is fibromuscular dysplasia, a condition in which the muscle and fibrous connective tissue in the wall of the renal arteries thicken and harden into a ring shape.
- The narrowing of the lumen of the renal artery or its branches is caused by the development of an aneurysm. Local expansions of the vascular walls are dangerous because they impede blood flow and pose a threat of rupture and hemorrhage. Find out more about the treatment of aneurysms by clicking on the link.
Publications in the media
Vasorenal arterial hypertension (AH, renovascular hypertension) is symptomatic (secondary) hypertension caused by ischemia of the kidney(s) due to narrowing of the renal artery or its branches, rarely due to bilateral damage. Statistical data. The prevalence is 1–2% (up to 4–16% according to specialized clinics) among all types of hypertension.
Etiology
• The most common cause of renal artery stenosis is atherosclerosis (reported among all types of renal artery stenosis in 62%). Localization of atheromatous plaques •• Proximal segments of the renal artery near the aorta (74% of cases) •• Middle segments of the renal artery (16% of cases) •• Near the bifurcation of the renal artery (5% of cases) •• Distal branches of the renal artery (5% of cases).
• Less commonly (in 24% of patients), a congenital disease is noted - fibromuscular dysplasia. The lesion is localized in the middle third of the renal artery. The following types of process are distinguished: •• Proliferation of the inner membrane ••• Primary ••• Secondary •• Dysplasia of the middle layer ••• Hyperplasia of the middle layer ••• Perimedial fibrous dysplasia ••• Dysplasia with the formation of microaneurysms ••• Dissection of the middle layer •• Subadventitial fibroplasia.
• Other types of stenotic lesions of the renal arteries are observed in 6% of cases •• Congenital artery stenosis (the most common cause of hypertension in children) •• Renal artery aneurysm •• Traumatic thrombosis and embolism •• Coarctation of the aorta with renal artery stenosis •• Nonspecific aortoarteritis •• Compression of the vascular pedicle of the kidney from the outside by a tumor or foreign body.
Pathogenesis
• Constriction of the renal artery activates the juxtaglomerular apparatus due to a decrease in blood pressure in the poststenotic segment, which leads to the release of renin, and a decrease in sodium concentration in the nephron loop.
• Renin converts angiotensinogen coming from the liver into angiotensin I, which is converted under the influence of ACE into angiotensin II, which directly affects systemic arterioles and sharply increases peripheral resistance.
• Indirectly through the adrenal cortex, angiotensin II leads to hyperaldosteronism, sodium retention in the body and an increase in extracellular fluid volume.
• The results of surgical treatment are largely determined by whether one or both renal arteries are affected •• With unilateral stenosis, the cause of hypertension is the renopressor mechanisms of the ischemic kidney. However, over time, the contralateral intact kidney will switch to a new blood pressure regime and will maintain hypertension even when the original source of hypertension is removed or revascularized •• With bilateral renal artery stenosis, its gradual elimination usually leads to a decrease in blood pressure. The same is observed during revascularization of a single kidney.
Clinical manifestations
• Renal artery stenosis can be suspected when hypertension occurs unexpectedly or when previously benign hypertension suddenly worsens. Arterial hypertension occurs before age 30 or after age 50, usually in the absence of a family history of hypertension. Characterized by rapid progression of hypertension, high blood pressure, rapid target organ damage, and resistance to treatment.
• Complaints •• Characteristic of cerebral hypertension - headaches, a feeling of heaviness in the head, hot flashes, tinnitus, pain in the eyeballs, memory loss, poor sleep, irritability, flashing “floaters” before the eyes •• Associated with overload of the left parts of the heart and relative or true coronary insufficiency - pain in the heart, palpitations, shortness of breath, a feeling of heaviness in the chest •• Caused by urological pathology - a feeling of heaviness, or dull pain in the lumbar region, and in the case of a kidney infarction - hematuria •• Caused by ischemia of others organs, the main arteries of which can be affected simultaneously with the renal arteries ••• Symptoms of ischemia of the gastrointestinal tract ••• Ischemia of the upper or lower extremities ••• Signs of cerebral atherosclerosis •• Signs of an inflammatory reaction (with nonspecific aortoarteritis) •• Complaints typical for secondary hyperaldosteronism - muscle weakness, paresthesia, attacks of tetany, isohyposthenuria, polydipsia, nocturia.
• As with any renal hypertension, high levels of diastolic blood pressure are characteristic, reaching in some cases 170 mm Hg.
• Systolic murmur in the right or left upper quadrant of the abdomen and along the posterior wall of the chest. The murmur is usually low-intensity, in contrast to the murmur heard with arteriovenous fistula of the kidney or atherosclerosis of the abdominal aorta (rough and prolonged).
Laboratory and instrumental data
• Hypokalemia (due to excessive secretion of aldosterone).
• Determination of plasma renin activity, especially in combination with the captopril test (100% sensitivity and 95% specificity): an increase in plasma renin activity after taking captopril by more than 100% of the initial value indicates pathologically high renin secretion, and is a sign of renovascular hypertension
• X-ray contrast angiography is the “gold standard” in the diagnosis of renal artery stenosis. The transfemoral Seldinger method is preferable: stenosis of the renal artery and (distal to it) its fusiform expansion are detected •• With nephroptosis, the renal artery is tense, it departs from the aorta at an acute angle, its diameter is narrowed •• With atherosclerosis of the renal artery, the filling defect is most often located near the mouth renal artery. Often, an angiogram reveals signs of atherosclerosis of the aorta •• With fibromuscular dysplasia, a multifocal narrowing of the renal artery is determined, in most cases starting at a distance of 2 cm distal to the origin of the artery from the aorta •• With nonspecific aortoarteritis, weaselation of the walls of the abdominal aorta is found along with narrowing of the renal artery. Stenotic lesions of other branches of the aorta are often determined •• In case of thrombosis or embolism of the renal artery, the symptom of a “blind ending” of the trunk of the renal artery or one of its main branches is determined •• In case of an aneurysm of the renal artery, its saccular or fusiform expansion is located mainly in the area of the renal hilum. The walls of the aneurysm often become calcified.
• Asymmetry of the kidneys on ultrasound.
• Doppler study of the renal arteries - acceleration of blood flow and its turbulence.
• Renal scintigraphy - decreased drug absorption, decreased drug delivery to the affected kidney, asymmetry of renographic curves. The optimal combination of renal scintigraphy and captopril at a dose of 25–50 mg orally. When taking captopril, the entry of the isotope into the kidney tissue decreases. A normal renal scintigram after taking captopril excludes hemodynamically significant renal artery stenosis.
• Excretory urography: the intensity of concentration of the contrast agent and the time of its appearance on the urogram may be reduced, as well as a decrease in the size of the kidney; however, the excretory urogram may remain normal, so the final diagnosis requires confirmation by aortography.
• MRI of the renal arteries is a modern method for verifying renovascular hypertension.
Differential diagnosis • Primary aldosteronism • Pheochromocytoma • Cushing's syndrome • Coarctation of the aorta • Diseases of the renal parenchyma, leading, for example, to chronic renal failure.
TREATMENT
General tactics. First of all, it is necessary to consider the possibility of radical treatment - percutaneous transluminal renal angioplasty, stenting of a stenotic artery, or radical surgical treatment. If such treatment is impossible or there are contraindications to it, drug therapy is prescribed.
Drug therapy is auxiliary, because a decrease in blood pressure with renal artery stenosis is non-physiological (leads to decompensation of blood circulation in the kidney and its shrinkage).
• Indications for long-term treatment are older age and systemic damage to the arterial bed, including the coronary arteries.
• Drugs of choice are ACE inhibitors, such as captopril. Additionally, other antihypertensive drugs are prescribed (see Arterial hypertension). Treatment begins with minimal doses of short-acting ACE inhibitors (for example, captopril at a dose of 6.25 mg). In the absence of collapse, the dose of captopril is increased or long-acting ACE inhibitors are prescribed. Monitoring of creatinine and GFR levels is necessary. ACE inhibitors are contraindicated in bilateral renal artery stenosis.
Balloon dilatation of the renal arteries
• Opinions about its effectiveness are controversial. In any case, this method is a good prognostic criterion for subsequent surgery: if after adequate dilatation even temporary normalization of blood pressure occurs, we can talk about a direct dependence of hypertension on renal artery stenosis.
• Indications •• Therapy-resistant hypertension in patients over 60 years of age with angiographically detected stenosis of the renal arteries •• Risk factors (stenosis of the carotid, coronary arteries, cardiac and respiratory failure) •• Renal failure caused by stenosis of the renal arteries •• Restenosis of the renal arteries after their revascularization or kidney transplantation •• As a diagnostic procedure to determine the relationship between renal artery stenosis and hypertension.
Surgery
• Organ-sparing operations •• Resection of the renal artery with reimplantation into the aorta •• Resection with end-to-end anastomosis •• Transaortic endarterectomy •• Autoplasty of the renal arteries with free grafts •• Creation of a splenorenal anastomosis •• Plastic surgery of the renal artery with synthetic antithrombogenic prostheses.
• Nephrectomy - if it is impossible to perform reconstructive surgery on the artery (the share of nephrectomies in the total number of operations is 16–20%).
• Contraindications •• Bilateral extended damage to the renal arteries •• Shrinkage of both kidneys •• Myocardial infarction and the period up to 6 months after it •• acute cerebrovascular accident •• End-stage chronic renal failure.
• Postoperative complications •• Internal bleeding •• Thrombosis of vascular anastomoses •• AKI.
• Results of operations •• Mortality is 0–6% •• Positive results with atherosclerosis of the renal artery are noted in 63% of patients, with fibromuscular dysplasia - in 73% •• The period of normalization of blood pressure after surgery can last up to 6 months.
• Postoperative management. Dispensary registration is recommended for patients. For residual hypertension, antihypertensive drugs are prescribed.
Reduction. AH - arterial hypertension.
ICD-10 • I15.0 Renovascular hypertension
Symptoms
The fact that arterial hypertension is associated with kidney disease is indicated by:
- young age of the patient;
- absence of hereditary predisposition: immediate relatives did not have vascular diseases or hypertension;
- associated lower back pain;
- ineffectiveness of medications intended to normalize blood pressure.
Symptoms of renovascular arterial hypertension depend on the nature of the disease: malignant and benign.
- In the malignant form, the disease progresses rapidly. In this case, diastolic pressure (lower) rises above 120 mm Hg. Art., accompanied by headaches, nausea, loss of consciousness. Patients experience visual disturbances and swelling.
- In the benign form of renovascular hypertension, consistently high diastolic pressure is observed. Overall health is satisfactory, although weakness, nausea, and chest pain are noted.&
Development mechanism
In the first stage, the immediate increase in blood pressure is a direct consequence of the increase in renin levels in response to impaired renal blood flow. For several weeks, blood pressure remains elevated, but the effect of increased renin levels depends on the function of the contralateral kidney.
Normal functioning of the contralateral side avoids an increase in circulating blood volume despite increased renin levels. Both kidneys are in opposition: the stenotic kidney retains sodium and releases excess renin in response to renal ischemia, while the unaffected kidney excretes excess sodium and water to maintain normal body fluid volume. Thus, there are symptoms of hypertension and elevated renin levels without a significant increase in circulating blood volume (CBV).
In the second stage, ischemia of the affected kidney leads to the retention of sodium and water, which increases the volume of blood volume and allows maintaining perfusion pressure in the kidney. Hypertension becomes less dependent on angiotensin II and is associated with increased sodium and water levels. Renin levels may decrease at this stage.
If blood circulation in the kidneys can be restored during these two stages, then blood pressure soon returns to normal levels.
In the third phase of development of vasorenal hypertension, changes develop in the renal parenchyma, so even elimination of renal artery stenosis no longer leads to complete normalization of systemic blood pressure.
An increase in blood pressure with narrowing of the renal artery is a compensatory mechanism that allows maintaining the filtration and excretory function of the kidney in conditions of reduced perfusion. Therefore, the use of drugs that block the production of angiotensin II (ACE inhibitors) to lower blood pressure can lead to the development of renal failure.
Diagnostics
If renovascular arterial hypertension is suspected, blood pressure measurement and auscultatory examination are performed. Changes in the vessels of the fundus are assessed. Next, the patient is prescribed diagnostics of blood vessels and kidneys:
- Ultrasound examination of the kidneys. Makes it possible to assess the size of the kidneys, see inflammatory processes and neoplasms.
- Ultrasound Dopplerography method. With its help, an image of the arterial network of the kidney is created, up to the interlobular arteries, and vascular stenosis is detected.
- Urine and blood tests.
- Renal angiography. Provides maximum information about the structure of the renal arteries, stenoses or occlusions, the nature and localization of the pathology.
- Urography helps determine the speed at which the contrast agent is distributed in the kidneys.
- Magnetic resonance imaging and CT.
Complications of renovascular hypertension
Renovascular hypertension leads to both complications characteristic of arterial hypertension and specific problems associated with poor blood flow in the renal arteries. If blood pressure is poorly controlled, the following complications may develop:
- Aortic aneurysm
- Myocardial infarction
- Heart failure
- Chronic kidney disease
- Stroke
- Vision problems (retinopathy)
- Poor blood supply to the legs - critical ischemia.
Treatment
When it comes to treating cardiovascular diseases, therapeutic methods are preferred. However, in the case of renovascular arterial hypertension, drug therapy alone is ineffective, and any delay is fraught with irreversible health problems.
- Drug therapy. Drugs are prescribed to treat hypertension and the underlying disease.
- Angioplasty. This is a minimally invasive type of intervention, which belongs to the methods of endovascular surgery. Using a small balloon inserted into the affected renal artery, the lumen of the vessel is restored.
- Stenting. Usually performed in conjunction with angioplasty. To prevent repeated narrowing of the vessel, a special metal prosthesis is inserted into the walls of the affected artery, which acts as a frame - a stent.
- Surgical operations. They are performed for serious damage to the kidneys and renal arteries, when the above methods have no effect. Depending on the indications, surgical treatment includes bypass surgery or even kidney removal.
Forecast
The prognosis in patients with renovascular hypertension is difficult to determine, and it depends on the degree of atherosclerotic lesions in other areas, individual sensitivity to antihypertensive therapy, and the effectiveness of surgical intervention. In patients with arterial hypertension, the presence of renal artery atherosclerosis is a factor in a significant increase in mortality compared with the general population. As kidney failure develops, the risk of death increases even more.
Surgery of the renal arteries (angioplasty and stenting) provides a very good prognosis for patients with renal vasoretension. In more than 70% of patients, blood pressure is normalized, without the need to take medications. In another 25%, the level of hypertension decreases, but still requires some drug therapy. Thus, in less than 5% of patients, restoration of blood flow through the renal artery is ineffective.