Renal artery stenosis is a pathology caused by hereditary or acquired changes in arterial vessels, which is a narrowing of one or both renal arteries or their branches. This condition causes a disruption in the process of perfusion - the passage of fluid - through the kidneys, leading to a decline in the blood supply to the kidneys and high blood pressure. In addition, renal artery stenosis can lead to heart failure, kidney failure, stroke and myocardial infarction.
Causes of renal artery stenosis
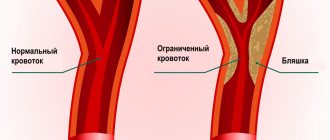
In 70% of cases, the cause of vascular narrowing is atherosclerosis, in which cholesterol deposits accumulate on the vascular walls, forming plaques. In 25% of cases, the pathology is caused by fibromuscular dysplasia. Occasionally, provoking factors include thrombosis and embolism of the renal arteries, aneurysms, nonspecific aortoarteritis, vasculitis, nephroptosis, benign and malignant tumors.
Increase the risk of developing stenosis:
- hereditary predisposition;
- smoking;
- excess weight;
- chronic kidney pathologies;
- increased concentrations of cholesterol and glucose in the blood;
- abuse of fatty foods and sweets;
- elderly age.
Preparing for treatment
If your stent surgery is scheduled for the morning, do not eat or drink after midnight (you can take the medicine with a sip of water in the morning). If the procedure takes place in the afternoon, do not eat after 10 am.
Tell your doctor about all the medications you take; about pregnancy; about allergies and sensitivities to medications, local anesthesia, latex, contrast dye, or iodine.
You may have a blood test to determine how long it takes for your blood to clot.
Diagnostic tests should be performed to determine whether renal artery stenting is required in this case. Among these tests:
- Angiography. During this test, a catheter is inserted through the groin into the aorta. The study allows you to see how well blood flows through the renal vessels and detect any other vascular pathology.
- Magnetic resonance angiography. This test is similar to a regular magnetic resonance imaging scan, which uses a large magnet to create images inside the body. In magnetic resonance angiography, contrast dye is injected into the blood to better visualize the vessels.
- Computed tomographic angiography. Uses a series of cross-sectional X-rays to create a three-dimensional image of the inside of the body. In our clinic, this is an indispensable method of accurate diagnostics, allowing us to accurately diagnose the pathology of the renal vessels and determine the indications for stenting.
- Duplex Doppler ultrasonography. This test uses sound waves to measure the size of the narrowed area and the speed of blood flow in the renal arteries.
Symptoms of renal artery stenosis
Stenosis is accompanied by:
- dizziness;
- pain in the lower back and abdomen;
- decreased urination or complete absence of urine;
- blood inclusions in the urine;
- rapid heartbeat;
- shortness of breath;
- muscle weakness;
- swelling of the legs;
- nausea, vomiting;
- fever;
- the appearance of “flies” before the eyes;
- sleep disturbance;
- memory impairment;
- emotional instability.
Due to the narrowing of the lumen, blood flows to the cells in insufficient quantities, which causes filtration to worsen, blood pressure to increase, kidney and heart failure to develop, and edema to form in the lungs. If left untreated, the kidney shrinks and ceases to perform its functions.
Clinical picture
Renal vascular pathology is accompanied by a clear clinical picture, including one or more symptoms:
- pain in the lumbar region;
- pain in the legs and under the ribs;
- swelling of the face and limbs;
- painful urination during a descending acute process;
- increased body temperature, fever;
- enlargement of the diseased kidney, which is noticeable upon palpation;
- vomiting, nausea, lack of appetite;
- shortness of breath, tachycardia, increased blood pressure.
Treatment of renal vessels begins after collecting the entire clinical picture, laboratory and instrumental diagnostics. The kidney vessels are checked using ultrasound and Dopplerography. Studies show the presence, structure, location of arteries, allow you to assess blood flow and detect pathological abnormalities.
Treatment of renal artery stenosis
Until recently, when there was stenosis of the renal arteries, the organ was removed. Now there are effective treatment methods (both surgical and conservative).
With drug therapy, the choice of drugs depends on the stage of the disease. The doctor may prescribe diuretics, antihypertensive drugs, anticoagulants, statins, fibrinolytics, ACE inhibitors and angiotensin receptor blockers.
Changing your lifestyle is important - quitting smoking and drinking alcohol, following a low-carbohydrate diet, losing excess weight.
In difficult cases, surgery is indicated:
- endarterectomy – blood clot is removed;
- angioplasty - dilates the artery using a balloon;
- stenting - a stent is placed inside the vessel to expand and strengthen the walls;
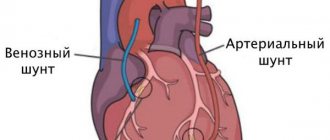
- shunting - with the help of shunts they create a bypass for blood;
- prosthetics – part of the renal artery is removed and replaced with a prosthesis;
- nephrectomy – kidney resection.
Primary appointment (examination, consultation) with a cardiovascular surgeon
1850 rub.
Sign up
Possible complications
Restenosis is more common in people whose renal vessels were very narrow to begin with, in patients over 65 years of age, women and smokers. Sometimes another stenting procedure may be needed to re-unblock the artery.
Risks of renal artery stenting include:
- Bruising in the area where the catheter was inserted
- Bleeding at or around the injection site,
- Damage to the vessel
- Thrombosis,
- An allergic reaction to the dye used during the procedure,
- Stent displacement
- Kidney failure
- Urinary tract infection.
Why is it better to treat renal artery stenosis at Major Clinic?
In our medical center, consultations are conducted by experienced doctors who in their work use high-tech equipment from leading manufacturers, which ensures highly informative diagnostics and maximum accuracy of surgical interventions.
Based on the examination results, our doctors will individually select a comprehensive treatment that will restore blood circulation, eliminate spasms, normalize kidney function and allow you to return to normal life.
The Major Clinic medical center is located in the center of the capital. It is easily accessible from any district of Moscow.
Types of vascular kidney diseases
Diseases of the vessels of the kidneys and urinary system are classified into groups:
- atheroembolic disease;
- thrombosis of renal vessels, stenosis;
- arterial blockage;
- cortical necrosis;
- nephrosclerosis;
- vascular tumors of the kidney;
- developmental anomalies.
Congenital anomalies in the development of kidney vessels include an extra, accessory vessel. Changes in the number of arteries interfere with the blood flow necessary for proper functioning.
Symptoms
Signs of arterial pathologies may vary for different anomalies.
For example, the main signs of stenosis (the most common pathology of the artery in the kidney - up to 2/3 of all cases of such kidney diseases), in addition to high blood pressure, are:
· Pain: headache, behind the sternum, in the lower back, in the eyes.
· Feeling of noise in the ears.
· Shortness of breath.
· Tachycardia.
· Presence of a small amount of protein in the urine.
· Uneven pressure on the right and left sides of the body.
The presence of aneurysm may have no symptoms at all until the dilation becomes very large or the aneurysm ruptures. If the dilatation is large, the ureter is compressed, the functioning of the kidney is significantly impaired, and infection with urinary toxins occurs. There is weakness, headache, and the smell of acetone.
When an aneurysm ruptures, the renal artery becomes blocked. If the patient is not immediately taken to the vascular surgery department, there is a high risk of death.
Atherosclerosis
Most often, renal artery stenosis provokes atherosclerosis. This term refers to the process of accumulation of plaque from cholesterol, fats and calcium on the renal arteries, which causes them to narrow. The risk of getting this disease increases with age. At risk are patients with damage to the aorta, arterial hypertension, and damage to the iliac arteries. This pathology is characterized by damage to one group of vessels due to stenosis, sclerosis, obliteration of arteries, and atherothrombotic disorders. Often, stenosis is located in the proximal segments of the renal arteries near the aorta, in the middle segments, at the bifurcation of the arteries, in the distal branches of the renal arteries.
Symptoms of the disease
If the kidneys are in the ischemic stage, it means they are not receiving enough blood and the body activates the RAAS (renin-angiotensin-aldosterone) system. With the help of enzymes and hormones renin, angiotensin and aldosterone, blood pressure begins to increase, and small vessels spasm. Due to the production of aldosterone, fluid is retained in the body. As a result, the patient develops secondary hypertension of renal origin.
Symptoms of the disease manifest themselves depending on the degree of blockage of the lumen of the arteries. If the diameter decreases by 70%, then the patient begins to worry about such manifestations as:
- Headaches, tinnitus,
- Dizziness
- Insomnia and weakness
- Irritability, hot flashes, facial redness.
- Sweating.
In this case, the processes of filtration and metabolism are disrupted, and the kidney parenchyma gradually becomes sclerotic. If the diameter of the vessels is reduced slightly, then SPA proceeds as a benign disease. The cause of the disease often depends on the age of the patient; in young people, arterial hypertension can be caused by the kidneys, namely dysplasia of the arterial wall.
Kidney anatomy
Later, additional symptoms appear, indicating damage to other organs:
- Cardialgia, feeling of irregular heart rhythm,
- Shortness of breath, appearance of sputum streaked with blood,
- The appearance of blood in the urine,
- Cramps,
- Increased nocturnal diuresis
In the initial stages of the disease, blood pressure numbers are steadily elevated, and the condition can be treated with medications. Indicators of systemic blood pressure can reach 200 mm. rt. Art. As the disease progresses, drug antihypertensive therapy stops working. Chronic renal failure gradually develops. In the terminal stages the disease can end:
- Chronic renal failure and anuria,
- pulmonary edema,
- Myocardial infarction,
- strokes,
- Retinal detachment.
Nephrological pathologies
Nephrological pathologies are the least likely cause of stenosis. Such pathologies include aneurysms, hypoplasia, occlusion and external compression of the renal arteries, vasculitis, thrombosis, nephroptosis, arteriovenous shunts.
Doctors also identify several risk factors that contribute to the disease. Such predisposing factors include:
- smoking;
- poor nutrition (predominance of foods high in sugar, fat and cholesterol in the diet);
- obesity;
- genetic predisposition;
- chronic kidney disease;
- increased blood glucose and cholesterol;
- elderly age.
Treatment of major renal vascular abnormalities
Stenosis, the basic symptom of which is very high blood pressure, requires complex drug therapy. Typically these are blood pressure lowering drugs and diuretics.
The use of medications, as a rule, is additional to surgical techniques , since the very cause of the disease does not eliminate the use of drugs, and the disease progresses. Stenosis confirmed by diagnostic measures is an indication for surgical intervention. Most often these are the following operations:
· Shunting . Shunts create blood flow that bypasses the pathological area of the artery.
· Angioplasty . An inflating balloon is inserted into the artery to widen it.
· Stenting. The vessel is expanded with stents - springy or mesh devices.
· Prosthetics . The operation is performed if it is impossible to perform angioplasty or stenting. The narrowed area is excised and an implant is placed in its place.
· Nephrectomy . During this operation, the indication for which is multiple stenosis, a practically non-functioning kidney is removed.
If stenosis is not treated, a third of patients are likely to die from strokes, heart attacks, and acute renal failure.
If an aneurysm , surgery is usually performed. In the most severe cases, the kidney is removed. But if the aneurysm does not grow, doctors resort not to open traditional operations, but to minimally invasive techniques. For example, during obliteration, a catheter with a special substance is inserted into the aneurysm, which immediately hardens, “bricking up” the pathological section of the artery.
Diagnosis of arterial renal anomalies
To identify the nature of arterial stenosis and the degree of narrowing of the vessel, various methods of examining the kidney are used:
· General blood and urine tests.
· Biochemistry of blood.
· Doppler ultrasound of the kidney (ultrasound studies the blood flow - its acceleration in the stenotic area - using color Doppler mapping).
· Angiography (study of blood flow by injecting a contrast agent into an artery).
· Scintigraphy (radioisotope method for studying the renal vessel).
· CT, MRI.
When using an angiographic technique, the doctor sees the pathological area of the vessel and can assess the degree of narrowing or widening of the artery walls, and determine all the necessary parameters of the renal artery anomalies.
Angiography is a very informative diagnostic method, but today visualization of large renal vessels through the use of multislice CT or MRI is a more informative and less invasive technique.