Vein thrombosis is a serious and dangerous disease that, in the absence of correct treatment and prevention, can lead to death. Blood clots sometimes form even for no apparent reason, but most often there are provoking factors - recent surgeries, injuries. To reduce risks, drug therapy is indicated. What medications do doctors prescribe for thrombosis? What is the difference between anticoagulants and antiplatelet agents?
Risk factors for thrombosis
Thrombosis occurs not only in older people, but also in young people. The reason for this is a number of factors that do not themselves lead to the formation of blood clots, but create all the conditions for this. The likelihood of forming blood clots increases in the following cases:
- overweight;
- passive lifestyle;
- forced bed rest for more than three days;
- varicose veins;
- recent myocardial infarction or stroke;
- use of oral contraceptives;
- fractures and injuries of the lower extremities;
- unhealthy diet, unhealthy lifestyle.
How medications help with vein thrombosis
All drugs prescribed for the prevention and treatment of venous thrombosis have a blood-thinning effect, since one of the main causes of the disease is increased blood clotting. They cannot miraculously dissolve existing blood clots, but they do prevent them from enlarging and forming new clots. Medicines to reduce clotting may have different principles of action, but give approximately the same effect. They are taken in courses or on an ongoing basis at the discretion of the attending physician.
Blood thinning medications are selected based on tests, diagnosis, and patient characteristics. Self-medication in this case is unacceptable, as it can lead to serious consequences. One of the main side effects is the risk of bleeding. More often it is minor and manifests itself in the form of bruises and nosebleeds. But an incorrectly selected drug and its dosage can lead to more serious consequences requiring hospitalization.
Signs of pulmonary thromboembolism
- A sharp decrease in blood pressure.
- Severe shortness of breath.
- Interruptions in the functioning of the heart.
- Pain in the chest area.
- Malfunctions
- gastro-
- intestinal tract.
- Blue in the face
- skin.
- Cold,
- sticky sweat.
The first thing to do if you suspect thromboembolism is to urgently call an ambulance, and before the medical team arrives, you need to lay the patient on a hard, flat surface and ensure complete rest. Calling an ambulance is very important - diagnosis
"thromboembolism" can be confirmed using an ECG. Doctors have 2–3 hours to administer drugs that dissolve blood clots (thrombolysis) or perform surgery. In mild cases, you can get by with prescribing anticoagulants.
Blood thinners - differences between anticoagulants and antiplatelet agents
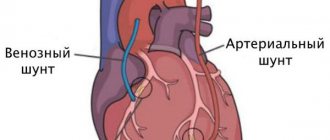
There are two groups of blood thinning drugs - anticoagulants and antiplatelet agents. All of them are intended to prevent thrombosis, but differ in their mechanism of action. Anticoagulants inhibit the activity of proteins involved in blood clotting. Antiplatelet agents prevent platelets from clumping together.
For thrombosis of the veins of the lower extremities, anticoagulants are most often prescribed. Drugs of the second group are indicated more likely for cardiovascular diseases - after valve replacement operations, heart attack or stroke. Their task is to minimize the risk of pulmonary embolism as a result of the formation and separation of a blood clot.
Standing and sitting work, long flights
Those at risk include cooks, salespeople, hairdressers, surgeons, traffic police officers, accountants, programmers, secretaries, as well as those who, as part of their duties, have to fly a lot on airplanes, stand in traffic jams, sit in a car, when people are forced to stay in a car for a long time. static, sitting position.
How to warn. When going on a long journey, sitting or standing idle in the office for hours, make it a rule to change your body position every 30 minutes or just walk. To prevent blood clots, you can also wear compression stockings (support stockings, stockings or tights).
Article on the topic
Thick means dangerous. What you need to know about blood clots
Anticoagulants
Anticoagulants are effective drugs that prevent excessive blood clotting and the formation of dangerous clots. They are divided into two large groups:
- Direct action. Mainly injectable drugs used in hospital settings, such as heparin, rivaroxaban. But there are also medications for oral administration. They act quickly, neutralizing clotting factors in the blood plasma.
- Indirect action. They are vitamin K antagonists and affect coagulation factors, gradually reducing their content in the blood. Many drugs from this group are indicated for continuous use; they begin to act slowly, but the effect lasts a long time. These include Warfarin, Aspirin, Trombital.
Anticoagulants are indicated for deep vein thrombosis, bleeding disorders, prevention of heart attack, stroke.
The most common blood thinners
Drugs in tablet form are excellent for outpatient treatment. Some of them are taken in long courses or on an ongoing basis if there is a high risk of blood clots. Below is a list of the main drugs.
Aspirin
Aspirin is an acetylsalicylic acid drug that has a wide range of uses. Its effect varies depending on the dosage. This is a time-tested, effective antiplatelet agent, especially often prescribed for cardiovascular diseases. In tablets of 50 mg and 100 mg, it is used for continuous use. In a high dose it is indicated for fever, to relieve moderate pain. Can be prescribed for varicose veins, thrombophlebitis.
The tablets irritate the gastric mucosa, so they are recommended to be taken strictly after meals. Erosive and ulcerative diseases of the gastrointestinal tract in the acute stage are a direct contraindication. The medicine is common and relatively safe compared to other antiplatelet agents, but it is still not recommended to take it on an ongoing basis without a doctor’s prescription.
Clopidogrel
An antiplatelet agent prescribed primarily for diseases of the heart and blood vessels - atherosclerosis, coronary artery disease, heart attack, unstable angina. Suppression of platelet aggregation is noted from the first day of administration.
Clopidogrel does not have too many contraindications, but it can cause side effects such as nosebleeds, abdominal pain, and dyspepsia. In patients over 75 years of age, treatment is carried out with caution, in moderate dosage.
Warfarin
One of the most common, frequently prescribed anticoagulants. Widely used for the treatment and prevention of thrombosis of various etiologies, thrombophlebitis, varicose veins, and secondary prevention of myocardial infarction. An excellent drug with repeatedly proven clinical effectiveness and safety. One of the few coagulants allowed during breastfeeding.
The drug can be taken only as prescribed by a doctor, since even many doctors note the difficulty of selecting a dose at the beginning of treatment for each individual patient. In addition, it is necessary to constantly monitor hemostasis indicators.
Trombital
The list can be supplemented with a modern combination drug consisting of acetylsalicylic acid and magnesium hydroxide. The antiplatelet agent prevents the formation of blood clots and, compared to Aspirin, does not irritate the gastric mucosa. For this reason, Trombital is prescribed to people with gastrointestinal diseases.
But the drug is used mainly for cardiac diseases, for the prevention of myocardial infarction, and for unstable angina. To reduce the risk of thrombosis of the veins of the lower extremities, doctors usually give preference to other drugs.
Blood thinners for injection
Direct anticoagulants are most often available in the form of an injection solution. Some are used only in hospitals, others are intended for self-administration by patients. At the moment, two drugs are most widely used.
Fraxiparine
Direct anticoagulant, low molecular weight heparin. Can be used by patients independently as prescribed by a doctor. It comes in a syringe with a small needle. It has a fast but short-lasting effect.
It is often prescribed by doctors for vein thrombosis; according to their observations, in most cases there is a pronounced positive dynamics and regression of the thrombotic process. The drug is potent and is prescribed with caution to elderly people, patients with low body weight, and severe arterial hypertension.
Heparin
One of the most common, frequently used direct-acting anticoagulants, widely used in hospitals for the treatment of patients with cardiovascular diseases, venous thrombosis, pulmonary embolism, and acute myocardial infarction.
Compared to other anticoagulants, it has a low cost, so it still remains the main drug in this group, despite the emergence of more modern analogues. It is practically not used at home due to the complexity of dosing, the injection form and the increased risk of bleeding.
To reduce the risk of thrombosis, in addition to blood-thinning drugs, agents may be prescribed to strengthen the walls of blood vessels and lower cholesterol levels. Considerable importance is attached to lifestyle - giving up bad habits, healthy eating, physical activity. The daily routine depends entirely on the person, and this is already a big step towards the prevention of thrombosis. But to prescribe the correct drug treatment, you need to consult a doctor.
Still have questions about protection against venous thrombosis?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.
Question to the doctor: how to avoid thrombosis
What can you do to reduce your risk of blood clots? What role does heredity play in the occurrence of thrombosis? What examination do you need to undergo to check the condition of your blood vessels? What research methods are used today? Does everyone at a certain age need anticoagulants? These and other questions from patients are answered by a cardiovascular surgeon at the National Medical Research Center for Surgery named after. A.V. Vishnevsky, candidate of medical sciences, associate professor Zaurbek Akhsarbekovich Adyrkhaev.
– What role does heredity play in the occurrence of thrombosis?
– From the point of view of heredity, there are several factors that may predetermine an increased risk of thrombosis. The first of them is genetic mutations, of which there are at least 12. In arterial thrombosis, this is also congenital hypercholesterolemia and hyperhomocysteinemia. These and other hereditary factors that can, at the level of blood rheology, predetermine an increased susceptibility to thrombosis - both venous and arterial - can be identified using laboratory diagnostics.
– Are arterial thrombosis and atherosclerotic plaques the same phenomenon?
– Plaques can increase the risk of arterial thrombosis - narrow the lumen of the vessel and thereby contribute to a change in the spectrum of blood flow in this area. Or they fragment - and then their pieces can come off, closing the lumen of the vessel or locally impeding the flow of blood in it, which leads to a decrease in the speed of blood flow and the formation of blood clots in this area.
– What are the differences between a blood clot and a plaque? Do they have different structures?
– A plaque is a denser formation, while a thrombus is a blood clot. A fresh blood clot is purplish-red in color, soft, and somewhat reminiscent of a slug in structure.
– Why does it form in some people and not in others? What is the mechanism of this blood thickening?
– All vascular doctors know the rules of Virchow’s triad (Rudolf Virchow is a German pathologist, a pioneer in the pathophysiology of thrombosis). In order for the process of thrombus formation to be started, three factors must occur: a slowdown in blood flow, damage to the endothelium (the internal lining of the vessel) and coagulopathy (increased blood clotting). Only in the presence of these three factors is the formation of a blood clot possible. One factor is not enough, but if it is present, as a rule, others join it and sooner or later begin to manifest themselves. Simply put, if a patient has a hereditary coagulopathy, he is already at risk. He may go on a long 8-hour flight, fall asleep on the plane and not wake up because his coagulopathy will be accompanied by a factor such as a decrease in blood flow.
– In what cases does it decrease?
– Under prolonged static loads - if a person stands for a long time, or sits, or rides in a car, flies on an airplane... In a word, being stationary contributes to the formation of venous thrombosis. At risk are also patients who have some kind of concomitant pathology - cancer, gynecological diseases that require taking hormonal medications. By the way, oral contraceptives also increase these risks.
Arterial thrombosis very rarely occurs without the presence of systemic atherosclerosis. Another risk factor for their occurrence is, of course, heart rhythm disturbances. If a patient, even with mild atherosclerosis, has atrial fibrillation, then against its background blood clots form in the heart, which can migrate and close the vessels, including the main ones - up to the aorta and iliac arteries, causing acute ischemia of the vessels of the legs.
– In what parts of the body do blood clots usually form?
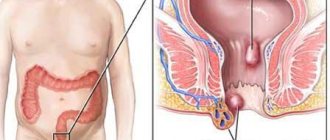
– With venous thrombosis, the most common location is the deep veins of the legs. The danger is that the blood clot quickly rises from the lower extremities into the femoral iliac veins. This carries enormous risks of pulmonary embolism - what is often popularly called a “blot clot.” This is the most dangerous complication of venous thrombosis, and, of course, if it is not diagnosed in time, it poses a real threat to the patient’s life.
With arterial thrombosis, the most common complication is embolism in the aortic bifurcation, when the iliac arteries close, as well as embolism in the arteries of the legs. The arteries most commonly affected are the crural arteries and the superficial femoral arteries, although others may also be affected. Here we are already talking about saving the limb, because, as a rule, such patients experience acute ischemia, which requires emergency surgical intervention to restore blood flow in the leg. And if this is not done in the coming hours, the patient may lose his leg.
– And if there is thrombosis, but it is asymptomatic, what should prompt a person to go to the doctor?
– Here we will also have to separate venous and arterial thrombosis. In the first case, this is usually a feeling of tension in the lower limb, sometimes visually assessed swelling, pain and redness along the veins that are visible on the leg. These moments should, of course, alert you, especially if this happens after those episodes that we talked about - taking hormonal drugs, pregnancy in women in the 3rd trimester, long journeys, sedentary work... If a person feels tension, swelling and pain in the limb, as well as redness and hyperemia along the vein, of course, he should consult a doctor.
If thrombosis is localized only in the veins of the leg, often the patient may even go unnoticed, and we will find out about it later - when he is examined for some other reason. By doing an ultrasound, we see that the veins are changed, and even if there are no blood clots, there are signs that the patient has suffered thrombosis.
As for arterial thrombosis, it is difficult to miss. If blood flow in any segment of a limb suddenly stops, the patient will somehow feel it. Of course, this is acute pain, coldness of the limb. The longer the ischemia lasts, the more neurological complications appear - in the form of numbness of the leg, limitation of movement in the ankle and knee joint. In later stages, of course, swelling appears.
The most difficult stage is the formation of so-called contracture in the knee and ankle joints, when the patient can no longer move the leg independently due to severe pain as a result of muscle spasms. The color of the leg changes, it first becomes pale, then a marble color appears. Severe episodes of acute ischemia are accompanied by dangerous complications such as phlegmon of the foot, etc.
If this process develops quickly, it can lead to wet gangrene, when the patient can no longer be helped. Therefore, it is so important not to miss the first symptoms - sharp pain that becomes permanent, coldness of the leg, change in skin color. And, of course, you should not try to treat yourself with home remedies; you should urgently consult a doctor.
– How does Dopplerography of leg vessels differ from ultrasound, and in what cases is this study performed?
– Doppler examination mainly shows the speed characteristics of blood flow; it is not aimed at determining the condition of the internal lining of the vessel, visualizing plaques or blood clots that nest there. Today this is no longer informative, and in our routine practice we are switching to color duplex scanning. It allows you to obtain complete data on both the speed characteristics of blood flow and the condition of the vessel as a whole: the thickness of its wall, the degree of inflammation, if any, the presence or absence of atherosclerotic plaques, how much they narrow the lumen of the vessel, whether there are blood clots in it or not, how much they spread, how many centimeters of the vessel they occupy, how tightly they are fixed to the wall (which is also very important).
– We are talking about the legs, but there are blood clots in the vessels of the head. Or is this a different story?
– Such thrombosis leads to a serious complication – stroke. Today in Moscow, and throughout Russia, a huge number of vascular centers have been opened, which are designed to combat acute coronary syndromes and acute strokes. Thrombosis results in a so-called stroke in progress, that is, the patient has the entire clinical picture of a stroke (a part of the body, an arm or a leg goes numb, speech is impaired, etc.). If an ambulance arrives on time for such a patient, it will take him to one of the vascular centers, where an attempt will be made to either systemic or local thrombolysis (dissolution of blood clots), or mechanical thromboextraction, when this thrombus is removed from the artery using special devices. Now there are all the possibilities for this, and these conditions are being dealt with quite successfully. The main thing is to do everything on time, to get into the so-called therapeutic window (from 6 to 12 hours).
– There is an opinion that after a certain age everyone needs to take blood-thinning drugs, and everything will be fine.
– Let’s start with what a person can do himself to protect himself as much as possible. The first and main thing is an active lifestyle. Aerobic exercise is needed. I tell my patients: you should walk 30-60 minutes a day, and not at a walking pace, but accelerating up to 3-4 km per hour. Do Nordic walking, swim, do whatever you like best, but be sure to move! And you should spend at least half an hour a day in the air, and spend it actively. Of course, you need to stop smoking - this is a proven fact of the risk of atherosclerosis and any complications of atherothrombosis.
The third thing is, of course, nutrition. Now the most popular diet, which is heard in all recommendations, is the Mediterranean diet. It is accessible and easy and enjoyable to stick to. The principles are very simple: limiting the consumption of animal fats and red meat (up to 1-2 times a week), the predominance of vegetable fats and fish, the basis of the diet is plant foods and plant proteins.
And another important point. In order to reduce the risk of blood clots, you need to maintain an adequate hydration regimen. A person must consume the required amount of liquid per day, and this is no less than a liter and a half (with soup, jelly, water, tea - it is not necessary to drink only clean water). By consuming liquid, you achieve blood thinning physiologically. If a person regularly does not get fluid and there is not enough fluid in his bloodstream, naturally, the blood will thicken, and the concentration of red blood cells per 1 ml of blood will increase. In this situation, he can, for example, go to the bathhouse and return from there with venous or arterial thrombosis. By sweating, a person loses up to several liters of fluid, which means that the same amount must be replenished.
Now about the drugs. I believe that no one should take anything without a doctor's recommendation. Outpatient therapists are now very educated in the field of prevention and possible complications of cardiovascular diseases, so every person should be observed in a clinic, undergo medical examination, which is being revived in our country, and if there are problems, register with a cardiologist or therapist, who, in accordance with will prescribe therapy based on indications. But you can’t take a drug that you’ve heard of or that your neighbor has been prescribed.
Previously, to reduce the risk of heart attacks and strokes, everyone was prescribed aspirin - but now studies have begun to appear that indicate the dubious benefits of uncontrolled and universal prescription of aspirin. 40 percent of people are generally tolerant to this drug, that is, when taking aspirin, they do not get the effect for which they take it. And no one who prescribes this aspirin monitors the expected effect. But everyone has a negative effect on the stomach and has long been proven.
– But new generations of antiplatelet agents have appeared.
“They are also not recommended for everyone, since they thin the blood so much that they carry the risk of bleeding. Yes, some people need them, especially after 50 years, but they should be prescribed by doctors according to indications. Everyone must do their job. The doctor is to treat, and the patient, being responsible for his health, tries to lead a healthy lifestyle as much as possible and consults doctors in a timely and periodic manner.
– You talked about a healthy lifestyle. And if, say, a blood clot already exists or is forming, can’t fitness provoke its movement?
– If at the age of 50 you decide to take up fitness for the first time in your life, of course, you should first be examined. Before starting classes, you must pass a basic fitness test. This is not at all the same as when they tell you how and what kind of exercise machine works; you should be consulted by a doctor who will determine your tolerance to physical activity and do tests under the control of an ECG and other devices.
– Let’s simulate such a situation. The person knows that there have been strokes and cases of blood clots in his family. And he wants to protect himself as much as possible. What examinations should he do to check the condition of the blood vessels?
– Firstly, a general and biochemical blood test, for a lipid profile - to find out the atherogenic index (the ratio of high and low density lipoproteins).
You need to take a coagulogram - look at blood clotting indicators, do an ECG, measure the ankle-brachial index, which reflects the state of blood circulation in the lower extremities. If this index is reduced, we can talk about systemic atherosclerosis. It is necessary to determine the level of homocysteine in the blood (an elevated level can also indicate atherosclerotic complications), and also perform an ultrasound of the carotid arteries.
I would also not overlook an abdominal ultrasound, which can look for an aortic aneurysm, which is often the first disease to manifest in a patient with atherosclerosis. And, of course, if a more in-depth examination is carried out, an echocardiogram will be required to see whether the heart muscle is functioning normally.
The brain, heart and lower extremities are the risk points for atherosclerosis and blood clots for a person who knows his hereditary predisposition to these diseases. And the listed studies are the minimum that will allow him to draw up a primary picture.
– And after this live in peace?
- Not certainly in that way. The person who has done all these studies should then go to the doctor. Even if the indicators are within the normal range, this may be the upper limit of the norm, which already indicates some changes. Only a doctor can determine the risks. And if changes in the vessels are detected, the examination must be repeated once a year.
Moreover, I recommend everyone to monitor their blood sugar, because diabetes is also one of the risk factors and worsens the prognosis in patients with atherosclerosis. As for venous thrombosis, you should pay attention to whether your legs swell at the end of the working day, whether you feel discomfort after long journeys and flights, whether it is difficult to put on boots or shoes. In this case, you need to do an ultrasound of the veins and again consult a doctor.
The main thing is not to self-medicate, it will never be effective. Take care of your blood vessels and overall health!
The full version of the interview was published in No. 5/20 of the Be Healthy magazine.