What is non-straightness of the vertebral arteries?
The vertebral arteries stretch from the prevertebral to the intracranial region, passing through the canal of the transverse processes of the cervical portion of the spinal column. If a person has received any injury, has a curvature of the spine or other diseases, this also affects the vertebral artery - it becomes bent. Blood flow is disrupted, the occipital part of the brain does not receive enough nutrition and oxygen. Irregular tortuosity of the artery is called “non-straightness of the VA”. In most cases, both arteries are affected, but non-straightness of the left vertebral artery or non-straightness of the right vertebral artery may also occur. This happens after a serious injury or the growth of a bone callus.
When a person has a non-linear course of VA on both sides, it is easier to make a diagnosis, and clear symptoms of the disease appear. If this pathology develops only on one side, the body tries to cope with the problem itself by increasing blood flow in the other vertebral artery. In this case, there will be practically no symptoms of the disease, but if the patient was examined for another disease, the doctor may notice this deviation.
Patient's office
Request a call
Symptoms and treatment of vertebral artery syndrome
From this article you will learn: what is vertebral artery syndrome. What diseases lead to the occurrence of pathology. Manifestations of this syndrome and examination methods to establish a diagnosis. Methods for correcting any violations that have arisen.
Content:
Causes of occurrence
Classification Manifestations of the syndrome Diagnostics Treatment
Prognosis
Vertebral artery syndrome (abbreviated as VAS) is a combination of symptoms from the brain, vascular and autonomic systems that arise against the background of damage to the nerve plexus of the artery itself, deformation of its wall or narrowing of the lumen.
In the medical community, such pathology is usually associated with diseases of the cervical spine, but predisposing factors in some patients are the anatomical features of the artery itself or concomitant vascular diseases, leading to changes in the elasticity of their walls and (or) narrowing of the lumen.
Regardless of the cause, the clinical manifestations of the syndrome are associated with two mechanisms that often combine to worsen the course of the disease:
1. Squeezing, or compression, of the artery leads to disruption of blood flow to part of the brain. 2. Irritation, or irritation, of the nerve fibers that surround the vessel leads to the activation of substances that cause narrowing of the arterial wall. This further disrupts the flow of blood to the structures of the central nervous system.
Negative manifestations of SPA include:
1. increased risk of developing an acute disruption of the blood supply to the brain of a temporary or permanent nature (transient ischemic attack, stroke); 2. decreased ability to work due to the need for a number of restrictions on movement and environmental conditions; 3. significant psychological discomfort against the background of clinical manifestations, especially in young patients.
Carrying out the necessary treatment significantly reduces the manifestations of the syndrome, but does not eliminate it completely.
Even after surgical correction methods, there are often residual effects of the disease, and the need for a restrictive regime of work and rest remains. Therapy significantly reduces the risk of acute vascular manifestations in the brain and the risk of fatal disruption of blood flow. Neurologists and neurosurgeons deal with the problem of diagnosis, choice of tactics for management and treatment of patients with SPA.
Factors that increase the risk of developing
| Group | Immediate factors |
| Features of artery anatomy | Deformation Tortuosity Kink Disturbance of the wall structure Incorrect movement |
| Diseases leading to a decrease in the lumen of the vessel | Atherosclerosis Hypertension Arteritis (inflammation of the wall) Thrombosis and embolism |
Vertebral artery syndrome occurs with the following diseases that cause compression of the vessel:
Osteochondrosis
– pathological destructive changes in the disc between two vertebrae, which begin in the central part (core), progressively spreading to the entire motor part of the vertebra.
Spondylosis deformans
– changes are associated with the aging process of the body, when, against the background of decreased blood flow in the capillaries, the nutrition of the intervertebral discs is disrupted, they lose their elasticity and decrease in size. This leads to the formation of bone spurs (osteophytes) on the front and side of the vertebra.
Spondyloarthrosis deformans
– pathology of the intervertebral joints, arising due to occupational hazards or peculiarities of the formation of the musculoskeletal system.
Deforming osteoarthritis of the spine
– one of the elements of systemic destructive damage to the joints of osteoarthritis. Affects two or more motor segments of the vertebrae.
Ligamentosis ossificans (Forestier disease)
– systemic damage to the ligamentous apparatus of the human skeleton, characterized by the deposition of calcium in the ligaments, which progressively reduces their extensibility and mobility.
Kimmerly Anomaly
– pathological structure of the first cervical vertebra.
Basilar impression
– violation of the location of the occipital bone, it is pressed into the cavity of the skull, compressing the spine.
Cervical spine injuries
associated with sudden hyperextension.
Compression of the artery by the neck muscles in certain head positions. Destructive changes in cervical localization of osteochondrosis lead to the development of RAS in 42.5–50% of patients.
Classification
Vertebral artery syndrome is classified according to the main causative mechanism, but in most cases the disease is of a mixed nature.
| Mechanism of occurrence | Its features |
| Compression | Compression of the lumen of the vessel from the outside |
| Irritative | Irritation of the nerve fibers of the perivascular plexus |
| Angiospastic | Reflex narrowing of the artery lumen in response to mechanical activation of receptors in the wall |
| Mixed | Any combination of the above options |
Manifestations of the syndrome
Patients with SPA experience constant difficulties in performing any tasks. Every wrong movement can cause clinical manifestations, forcing the patient to limit himself in work and everyday activities. The symptoms themselves are quite painful and disturb the psychological peace of the sick, forcing them to consult doctors to correct it.
In the clinical course of the syndrome, two phases of development are distinguished:
| Phase | Her characteristics |
| 1. Functional or dystonic | Symptoms are not persistent Good response to treatment Low risk of stroke |
| 2. Organic, or ischemic | The appearance of a focus of persistent disturbance of blood flow High risk of developing acute posterior cerebral stroke The effect of treatment is reduced, residual effects on the brain are possible |
In vertebral artery syndrome, symptoms are highly variable and affect many functions:
| Clinical variant of the symptom | Its manifestations |
| Posterior cervical sympathetic syndrome (Barré-Lieu) | Pain in the neck and back of the head with reflection (irradiation) to the forehead Constant, pulsating pain Intensifies in the morning after sleep, with movement and shaking, sudden turns of the head Noise in the ears Decreased hearing Flashes before the eyes |
| Basilar migraine | The attack begins with changes in vision (sparks, loss of part of the image) Severe dizziness and gait disturbance Incoherent speech Tinnitus Pain in the back of the head |
| Vestibulo-atactic syndrome | Impaired gait and balance Nausea and vomiting Dizziness Darkness in the eyes Rapid pulse Increased blood pressure |
| Cochleovestibular syndrome | Hearing loss Tinnitus that changes when you turn your head Unsteadiness when walking Swaying |
| Visual or ophthalmic syndrome | Flashes, flickering before the eyes Deterioration of vision Tearing Rapid eye fatigue Redness of the eyes Feeling like “sand has been poured into the eyes” Periodically loss of part of the visible image |
| Autonomic dysfunction syndrome | Feeling hot or cold Increased sweating Cold feet and hands Difficulty swallowing Voice problems Insomnia or drowsiness |
| Vertebral syncope (Unterharnscheidt) syndrome | A short attack of loss of consciousness during certain movements of the neck or prolonged stay in an uncomfortable position |
| Transient ischemic attack | Impaired active movement of the limbs Changes in skin sensitivity Loss of vision Loss of balance when walking Dizziness with nausea and vomiting Double vision Inability to speak and swallow |
| Drop attack attacks | Sudden paralysis of the whole body with a fall after throwing back the head. The duration of the attack is from several seconds to a minute |
| Mental changes | Unpleasant sensations of foreign material in the upper half of the body Refusal to eat Decreased all types of activity Thoughts about a fatal disease and the inability to recover from it |
The disease can manifest itself in only one of the listed options or a combination of them.
Diagnostics
Vertebral artery syndrome is a multifaceted disease that often imitates various pathologies of the organs of vision, hearing, neck, and brain.
Therefore, the main method of establishing the correct diagnosis is a thorough interview of the patient to identify the prevailing syndrome of the disease. To clarify the cause of the pathology, a number of additional procedures are required:
| Study | Target |
| X-ray of the cervical spine and skull bones with functional loads | Primary assessment of bone elements Identification of gross skeletal pathology |
| Ultrasound scanning of the vessels of the neck and head | Inspection of the artery itself for anatomical changes, pathology of the wall and lumen, identification of compression and kinks of the vessel |
| Multislice computed tomography | Assessment of all bone structures, identification of pathology associated with the destruction of elements of the spinal column |
| Magnetic tomography of the cervical spine and blood vessels of the head and neck | Assessment of “soft” skeletal elements (discs, ligaments), identification of pathology from the artery itself and its branches |
| Angiography | A clarifying method in complex diagnostic situations. Indicated for suspected blockage of an artery by a blood clot to select subsequent treatment. |
Treatment
Treatment of vertebral artery syndrome includes both medicinal effects on the vessels and surrounding tissues, and surgical methods for correcting compression by the bone structures of the vertebrae. There is no complete cure for the disease, since pathological processes in the elements of the spinal column are irreversible .
But a complex effect on all elements of the mechanism of occurrence makes it possible to slow down and (or) stop changes, as well as reduce the clinical manifestations of the syndrome.
Medicinal methods of correction
1. Drugs to relieve swelling and inflammation
When the lumen of the bone canal decreases, the venous vessels are the first to be compressed, and against the background of impaired blood outflow from the brain, increased compression of the vertebral artery occurs. Any prolonged compression leads to a local inflammatory reaction. Therefore, spa treatment begins with these medications:
— Troxerutin; — Diosmin; — Nimesulide; — Celecoxib; - Lornoxicam.2. Medicines that normalize blood flow in the arteries Against the background of disruption of the normal blood supply to brain structures, the risk of stroke and transient attacks increases. To prevent complications use: - Pentoxifylline; — Vinpocetine; — Cinnarizine; — Nicergoline; - Instenon. 3. Drugs to protect nerve cells Under conditions of lack of blood flow, neurons are exposed to free radicals and suffer from a lack of oxygen. Medicines from this group are indicated in the phase of organic disorders in SPA in order to prevent the development of persistent impairment of brain function. — Citicoline; — Gliatilin; — Actovegin; - Cerebrolysin; — Piracetam; — Mexidol; - Mildronate; - Sumatriptan; — B vitamins; - Antispasmodics. 4. Non-medicinal treatment is aimed at relieving spasm of the muscles surrounding the spine and improving blood flow in this area - massage; - acupuncture; - PRP therapy; - physiotherapy (UHF, shock wave, HILL laser, magnet, amplipulse); — therapeutic exercises and physical education; - sanatorium treatment.
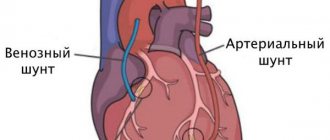
Surgical correction
To relieve pressure on the artery, a number of techniques are used to normalize the supporting function of the spinal column:
1. Percutaneous spinal fusion
– fixation of two adjacent vertebrae relative to each other
2. Fenestration of discs between vertebrae
– creation of artificial defects in them for the growth of connective tissue
3. Autodermoplasty of discs
– replacement of the intervertebral disc with one’s own tissues
4. Replacement of the disc
with a titanium-nickel explant
Prognosis
Vertebral artery syndrome cannot be completely cured cure.
This is due to causal pathological factors - changes in the osteoarticular component of the spinal column do not undergo reverse development. Any surgical techniques provide a temporary or incomplete therapeutic effect. Drug correction is aimed at reducing the clinical manifestations of the disease, but has virtually no effect on the primary cause of the pathological process. Despite this, all treatment methods significantly alleviate the course of the disease and stop its progression.
More details
Causes of pathology
Why might a person develop this disease? Non-straightness of the course of the vertebral arteries between the transverse processes and in other areas (there are several sections of the VA: prevertebral, cervical, cervico-occipital, intracranial) appears due to a number of diseases:
- cervical osteochondrosis;
- congenital anomalies;
- injuries in which the cervical spine was damaged;
- hypothermia, which causes muscle spasm, which affects the location of the artery;
- tumor;
- Bekhterev's disease;
- scarring of tissue after surgery.
These are the main reasons, but there may be others.
Medical Scientific and Practical Center for Vertebrology and Neuroorthopedics, Professor M.L. Kurganov
The names for this suffering are varied, just as its manifestations are varied. This syndrome was described in 1925 by doctors Barre and Lieu for cervical spondyloarthrosis. Now synonyms are often used: “posterior cervical sympathetic syndrome” , “cervical migraine” . Such diagnoses are often used in medical documentation and doctor's notes. Therefore, there is a need to explain to my patients what we are talking about. In a broad clinical sense, vertebral artery syndrome is a disturbance of blood flow to the brain in the basin of one or both vertebral arteries. A little about the blood supply to the head.
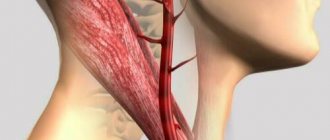
The brain is supplied with blood from 2 pools. The first - carotid - includes the carotid arteries. They (or rather, their main branches - the internal carotid arteries) provide up to 70-85% of blood flow and are responsible for all major circulatory disorders, primarily strokes. They are traditionally given special attention during examination; their atherosclerotic lesions and its complications are the object of special attention of cardiologists, neurologists, and vascular surgeons.
The vertebral arteries (right and left) belong to the vertebrobasilar region, supply blood to the posterior parts of the brain and, according to various sources, provide about 15-30% of blood flow. Their defeat does not lead to such serious complications as a stroke, but they can ruin the patient’s life for a long time and make him disabled.
Arterial damage manifests itself as
- severe dizziness,
- headache,
- loss of consciousness,
- coordination disorders,
- hearing and vision impairments.
The causes of damage to the vertebral arteries can be divided into 2 groups:
• The first group is non-vertebrogenic (not associated with the spine) lesions. They are caused either by atherosclerosis (it occurs much less frequently than in the carotid arteries), or by congenital anomalies in the size and course of the arteries. These anomalies usually have no independent significance, but when combined with other causes of arterial compression, they provide an unfavorable background.
• The second group is vertebrogenic (associated with spinal pathology) lesions. These are disorders caused by diseases of the spine. They can appear as early as adolescence with dysplastic and post-traumatic instability of the cervical spine. But the most pronounced changes develop in adults with the development of osteochondrosis.
The fact is that the artery passes part of its path to the skull in a bone canal formed by the transverse processes of the cervical vertebrae (starting from the 6th to the 1st vertebra). With osteochondrosis, deformation of the lateral (hook-shaped) processes of the vertebral bodies develops, the so-called uncovertebral arthrosis, and vertebral instability caused by the destruction of the intervertebral discs. All these reasons lead first to irritation of the sympathetic plexuses of the vertebral arteries, their subsequent spasm, and then to compression of the arteries throughout the entire bone canal or at the entrance and exit of the artery with the development of short-term circulatory disorders that occur when turning and tilting the head, changing position torso.
Clinical picture
The main characteristic symptom is headache . Characterized by a constant, sometimes intensifying, painful headache of a burning, sometimes pulsating nature in the occipital region. During an attack, pain can spread to other areas of the head, often radiating to the orbit and bridge of the nose (“cervical migraine”), to the parietal-temporal region, to the forehead, and ear. Most often localized on one side, it can be paroxysmal or permanent. The pain clearly intensifies with neck movements. Pain in the scalp often occurs even with a light touch or combing of the hair. When turning or tilting the head, a “crunch” is often heard, and sometimes a burning sensation is felt. In some patients, the syndrome manifests itself as dizziness with nausea or vomiting, a sensation of noise, ringing in the ears (often synchronous with the pulse). Dizziness develops when the head is raised upward (the artery goes into the narrow part of the hole), and with atherosclerosis of the cerebral vessels, dizziness develops when the head is tilted forward.
Sometimes there is decreased hearing and visual disturbances: decreased visual acuity, “spots”, blurred vision, fog before the eyes, double vision. Occasionally, swallowing problems and a sensation of a foreign body in the throat occur - the so-called pharyngeal migraine. When the vertebral artery is compressed, there are paroxysmal conditions that are clearly associated with turning the head:
- after turning the head, the patient falls “as if knocked down,” but does not lose consciousness, and soon gets up on his own;
- after a sudden movement of the head, the patient suddenly falls and loses consciousness. After 5 - 20 minutes he comes to his senses, gets up, but for a long time he feels weak.
There are also autonomic disorders: short-term feeling of hunger, thirst, feeling of heat or chills.
With a leading lesion of the sympathetic plexus of the vertebral artery, Bernard–Horner syndrome is noted. Pain and paresthesia in this case are often one-sided and can affect the face, hard palate, teeth, tongue, pharynx (tingling, burning, foreign body sensation). Vestibular disorders are usually observed in the form of spin, a feeling of staggering and sinking, accompanied by nausea, ringing and noise in the ear. During a headache, blurred vision, flashing before the eyes, increased fatigue, decreased performance, sweating, and chills may occur. In all cases there is a neurotic background. Changing the position of the head leads to increased headaches, but the patient can find a certain position in which the pain disappears or decreases.
Diagnostics and additional methods
Currently, the main method for diagnosing circulatory disorders in the vessels supplying the brain is generally accepted to be Doppler ultrasound (USD).
The study of the arteries of the carotid and vertebrobasilar basins is called USDG of the branches of the aortic arch or USDG of estracranial vessels. However, when performing a standard ultrasound examination, the main attention is traditionally paid to the carotid arteries, and the examination of the vertebral arteries is performed only partially. This is also due to the lack of uniform standards and differences between different schools of specialists. Often the artery is not examined along its entire length, but only in the initial and final segments, functional tests are not performed, the conclusion about the pathology of the vertebral arteries is made based on indirect data, the specific causes and level of compression are not indicated.
Treatment of vertebral artery syndrome: When treating this condition, the main goal is adequate blood circulation in the vertebral arteries , as well as eliminating or minimizing the causes of irritation or vascular spasm. The treatment uses methods of manual therapy, reflexology, vacuum therapy, pharmacopuncture, magnetic therapy, exogenous bioresonance therapy with fixed frequencies. Vascular therapy is necessarily involved in the complex of therapeutic measures. If necessary, anti-inflammatory drugs and mild antidepressants are prescribed.
Symptoms
When a person has a non-linear course of the vertebral arteries, symptoms can only indicate that blood circulation in the brain is impaired. Only a complete examination will help make the correct diagnosis.
Stage of functional impairment (dystonic)
The main symptoms that show that the patient has a non-straightforward course of the vertebral arteries:
- the back of the head hurts, the pain is bursting and aching;
- there is a feeling of pressure in the back of the head;
- neck pain regularly;
- dizzy when getting out of bed;
- blood pressure rises, it is not possible to lower it with medications;
- there is no strength to do everyday work, you constantly want to sleep, it’s hard to wake up in the morning;
- nausea bothers me, nosebleeds appear, although there are no problems with the gastrointestinal tract;
- weakness in the arms and legs, even if the person has not played sports;
- Vision and hearing deteriorate, tinnitus appears, and “spots” flash before the eyes.
Ischemic stage
It is advisable to consult a doctor as soon as the above symptoms occur. He will refer you for examination and prescribe a course of treatment. If symptoms are ignored, irreversible changes may occur. With severe deformities, a spinal stroke develops. Its main symptoms:
- gait becomes unsteady;
- facial expressions change;
- the tongue deviates to one side;
- there may be paralysis of the legs or arms on the left or right side;
- the patient cannot speak.
In this case, we are talking about life and death, the patient must be urgently taken to a neurological or special vascular hospital.
Clinical types of the syndrome
Posterior cervical sympathetic syndrome (Barre–Lieu)
Posterior cervical syndrome is characterized by headaches localized in the cervical-occipital region with radiation to the front of the head. The headache is usually constant, often in the morning, especially after sleeping on an uncomfortable pillow. Headache may occur when walking, driving a car, or when moving the neck. The headache can also be pulsating, piercing, localized in the cervical-occipital region and radiating to the parietal frontal and temporal zones. Headache may intensify when turning the head and is accompanied by vestibular, visual and autonomic disorders.
Migraine basilar
Basilar migraine does not result from compression of the vertebral artery, but from stenosis of the vertebral artery, but clinically has much in common with other forms of vertebral artery syndrome. As a rule, a migraine attack begins with a sharp headache in the back of the head, vomiting, and sometimes loss of consciousness. Visual disturbances, dizziness, dysarthria, and ataxia are also possible.
Vestibulo-cochlear syndrome
Disturbances from the hearing system manifest themselves in the form of noise in the head, decreased perception of whispered speech and are recorded by changes in data during audiometry. Tinnitus is persistent and long-lasting and tends to change when the head moves. Cochlear disorders are associated with dizziness (both systemic and non-systemic).
Ophthalmic syndrome
With ophthalmic syndrome in the foreground, visual disturbances such as scintillating scotoma, decreased vision, photopsia may also be symptoms of conjunctivitis (lacrimation, conjunctival hyperemia). Loss of visual fields can be episodic and is mainly associated with changes in head position.
Autonomic change syndrome
As a rule, autonomic disorders do not appear in isolation, but are combined with one of the syndromes. Autonomic symptoms are usually the following: a feeling of heat, a feeling of cold extremities, sweating, changes in skin dermographism, sleep disturbances.
Transient ischemic attacks
Ischemic attacks can occur during the ischemic stage of vertebral artery syndrome. The most common symptoms of such attacks are: transient motor and sensory disturbances, visual disturbances, hemianopsia, ataxia, attacks of dizziness, nausea, vomiting, speech impairment, swallowing, double vision.
Syncopal vertebral syndrome (Unterharnscheit syndrome)
An episode of syncopal vertebral syndrome is an acute circulatory disorder in the area of the reticular formation of the brain. This episode is characterized by a short-term loss of consciousness when turning the head suddenly.
Drop attack episodes
An episode of a drop attack (fall) is caused by impaired blood circulation in the caudal parts of the brainstem and cerebellum and will clinically manifest itself as tetraplegia when the head is thrown back. Restoration of motor functions is quite rapid.
Diagnosis of vertebral artery syndrome
If unpleasant symptoms appear, go to the doctor: the sooner the better. a therapist first
, he will give a referral to
a neurologist
. Even an experienced doctor will not be able to diagnose you without an examination, because... he needs to study the pictures to make sure that the blood flow is disrupted. Each doctor himself makes a list of examinations, but most often it includes the following components:
- Doppler ultrasound
, which shows the speed and direction of blood flow, arterial patency; - compression-functional tests;
- duplex scanning showing the condition of the vessel walls;
- MRI
; - radiography.
Based on the results of the examination, the doctor will determine whether the course of the vertebral arteries is really disrupted or whether it is another syndrome, another disease.
How to treat?
If you have non-straightness of the vertebral arteries, treatment depends on the severity of the symptoms. In the early stages, conservative treatment can also help. It is necessary to figure out what caused the pathology and first cure the underlying disease. If the cause of this pathology is a spasm of the cervical muscles, it needs to be removed. Physical therapy or massage may help. Conservative treatment did not help? Then the doctor prescribes surgery.
Drug treatment
The doctor also decides which medications to prescribe, but most often drugs that improve venous outflow, painkillers, pills that lower blood pressure, etc. are prescribed. Such treatment cannot solve the problem itself, i.e. correct changes in the vessel, but it improves the patient’s well-being.
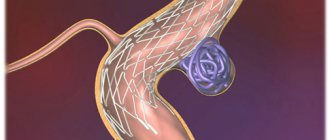
Surgical
The operation is prescribed if the doctor fears that the patient will have an ischemic stroke. The surgeon decides what exactly needs to be done. Sometimes he shortens and straightens the artery, sometimes he performs prosthetics or stenting.