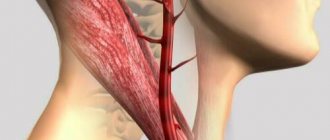
The blood supply to the brain structures is carried out using the vessels of the neck. These are two carotid and two posterior vertebral arteries. The former are responsible for the supply of arterial blood to the anterior lobes of the brain, the latter – to the posterior lobes. With the help of the vertebral arteries passing through the cervical spine, the medulla oblongata, respiratory center, optic nerve, and vestibular apparatus are supplied with blood. Therefore, compression of the vertebral artery can lead to imbalance, a sharp decrease in visual acuity, frequent headaches, shortness of breath, decreased vital volume of the lungs, drowsiness, increased fatigue, attacks of nausea, etc. In severe cases, the patient develops depression and may experience suicidal thoughts.
Compression of the cervical vertebral artery can occur with the development of degenerative dystrophic disease of the intervertebral discs. Osteochondrosis leads to the fact that the position of the blood vessels is disturbed, their course becomes tortuous and uneven.
The posterior vertebral arteries leave the thoracic cavity when the subclavian branches branch at the level of the 6-7 cervical vertebra. Then they follow along the lateral surfaces of the vertebral bodies. Therefore, intervertebral discs protruding beyond the vertebrae and affected by protrusion can provoke severe stenosis of the arteries. This usually occurs when the head is turned suddenly.
In a healthy person, with such a movement, the fullness of the cerebral vessels also changes. But, if the posterior vertebral artery is compressed by a protruding intervertebral disc or a herniated protrusion of the nucleus pulposus, then the blood flow stops. At this moment the person experiences an attack of severe dizziness, nausea and weakness. If blood flow is disrupted for a long time, fainting may occur.
Extravasal compression of the vertebral artery is a condition that poses a potential threat to the life and health of the patient. In the case of total stenosis and cessation of arterial blood supply to the brain structures, an ischemic stroke develops. This is an acute disorder of cerebral circulation, which, with a favorable outcome, will lead to paralysis and disability of the patient. Under unfavorable circumstances, the patient may die from cardiac or respiratory arrest.
Also, compression of the vertebral artery can lead to the development of hemorrhagic stroke. This condition can be triggered by prolonged compression of a blood vessel, and then a sudden release of pressure on it. At this point, too much blood under high pressure will begin to flow to the brain. This can provoke rupture of the vessel and hemorrhage into the cerebral structures. With the hemorrhagic type of stroke, the prognosis in most cases is very unfavorable. Most patients die within a few days.
The proposed material describes the main reasons for the development of compression of the posterior vertebral artery. Information about the first clinical signs and symptoms of the pathology is also provided here. If you experience such manifestations of the disease, seek medical help immediately.
In Moscow, you can make a free appointment with a neurologist or vertebrologist at our manual therapy clinic. Experienced doctors will conduct all necessary manual examinations. Then, after an accurate diagnosis is made, an individual treatment plan will be developed.
What is extravasal compression of the vertebral artery?
To answer the question of what extravasal compression of the vertebral artery is, you should understand this complex term step by step.
“Compression” in medicine means “squeezing something,” in this case the vertebral artery. The vertebral arteries pass through the intervertebral foramina of the cervical vertebrae towards the spinal canal, where they supply the spinal cord. Compression of the vertebral artery is not an independent disease, but rather a consequence of the development of another pathology.
Most often, this pathology is an intervertebral hernia. It is the resulting hernia that can compress the vertebral artery, thereby disrupting the blood supply to the spinal cord. Extravasal compression of the vertebral arteries is usually localized in the area of the 4th-5th vertebrae.
Causes of the disease
As mentioned above, an intervertebral hernia can lead to extravasal compression of the right, left, or simultaneously two vertebral arteries. In turn, a hernia can occur due to developed osteochondrosis or physical overload. Other provoking factors may be:
- benign or malignant tumors in the neck;
- incorrect, abnormal structure of the spine, its curvature (congenital, acquired, traumatic).
Signs of extravasal compression of the vertebral artery
Signs of extravasal compression of the right, left, or both vertebral arteries are most often temporary. This pathology manifests itself as pain. Pain appears when turning the head sharply or in the morning after waking up (since during sleep a person can remain in one position for a long time). In addition to neck pain, compression is manifested by headache (aching, throbbing), dizziness, indigestion, difficulty moving, impaired vision or hearing, and lacrimation. Also, compression of the vertebral arteries can lead to the development of neurological diseases.
Extravasal compression of the left vertebral artery
You can understand the signs of compression in more detail by the type of its localization. For example, if this pathology affects the left vertebral artery, then the symptoms may be as follows:
- frequent headache;
- dizziness, tinnitus;
- increased blood pressure;
- nausea.
With pronounced compression of the left vertebral artery, a person may even faint.
Extravasal compression of the right vertebral artery
The same symptoms may occur in patients with compression of the right vertebral artery. During exacerbations of the disease, a person may from time to time lose a sense of balance and fall, but remain conscious.
Bilateral – compression of both vertebral arteries
When both vertebral arteries are compressed, all of the above symptoms persist, but gain double strength. Moreover, all these symptoms are not specific, that is, they can accompany other diseases. This is why compression is so difficult to diagnose and prescribe treatment in a timely manner.
Nature SPA
To a certain extent, SPA is a collective concept and unites a complex of cerebral, vascular and autonomic syndromes that arise as a result of damage to the sympathetic plexus of the vertebral artery, deformation of its wall or changes in the lumen [7, 11]. In ICD-10, it is considered under the code G99.2 and includes the clinic of posterior cervical sympathetic syndrome, repeated episodes of vertebrobasilar insufficiency, episodes of drop attacks, and Unterharnscheidt syndrome. In neurological practice, the diagnosis of SPA is usually made to patients with a certain set of complaints and clinical syndromes that can be associated with degenerative lesions or anomalies of the cervical spine. According to Kalashnikov V.I. (2008), it is more correct to use the term “vertebrogenic vertebral artery syndrome.” Indeed, an analysis of the available literature data allows us to speak specifically about the vertebrogenic nature of dysgemia in the vertebrobasilar region, which underlies SPA [6, 10, 12].
One of the main roles in the development of SPA is played by the state of the perivascular plexuses and the lower cervical sympathetic ganglion, which determines the sympathetic innervation of the vertebral artery [7]. Compression and restriction of blood flow in one or both arteries can occur under normal physiological conditions, but blood circulation in them is usually not impaired due to sufficient compensatory capabilities [13]. The situation changes with hypoplasia (anatomical narrowing) or atherosclerotic stenosis of the arteries. In this case, extravasal factors become decisive factors in circulatory failure in the vertebrobasilar system. Osteophytes formed during osteochondrosis and spondylosis deformans in the area of uncovertebral joints have the greatest compressive effect on the vertebral arteries. Displacement and compression of these arteries can also be observed as a result of subluxation of the articular processes of the vertebrae. In addition, with pathological mobility in individual segments of the cervical spinal column (two vertebrae connected by a disc), the vertebral artery can be injured by the apex of the superior articular process of the underlying vertebra [14–16]. Compression of the vertebral arteries is also possible by the neck muscles (scalenus, longus colli, inferior oblique capitis) in certain head positions [3].
A common cause of the development of SPA is uncovertebral arthrosis. Even small uncovertebral exostoses can have a mechanical effect on the vertebral artery [10, 12]. Initially, osteophytes cause dynamic irritation of its sympathetic plexus only during certain positions or movements in the cervical spine. Then, osteochondral growths can cause compression of the lumen of the vertebral artery canal - compression-irritative syndrome. In addition to mechanical compression, a reflex spasm of the vessel occurs as a result of irritation of the periarterial nerve plexus and angiospastic syndrome develops. The clinic is dominated by diffuse vegetative-vascular disorders, less associated with head turns. The compression-irritative version of PSA is more often associated with pathology of the lower cervical spine, while the reflex version is more often associated with pathology of the upper cervical spine. As a rule, mixed (compression-irritative) variants of SPA are encountered in clinical practice [3]. Kalashnikov V.I. (2008) proposed a clinical classification of PAS, based on a comprehensive assessment of pathogenetic factors and clinical stages of the disease.
Diagnostic methods
At the first examination, the therapist
,
a neurologist
or other specialist can only suspect the presence of compression of the vertebral artery by asking the patient about all the symptoms, as well as examining him and palpating him. To clarify, confirm (or refute) the diagnosis, the following procedures may be prescribed:
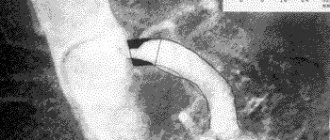
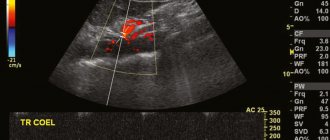
- Ultrasound with Doppler. It is the Doppler study that allows us to evaluate the speed of blood flow in the arteries. On the screen, the doctor can see the lesions and identify the degree of development of the disease.
- MRI
. - CT scan
. - X-ray
.
The last three studies on the list help evaluate the structure of soft and bone tissues, identify fractures, dislocations, foci of inflammation, vascular pathologies, and tumors of various origins.
How to treat?
Treatment of extravasal compression of both vertebral arteries is primarily to eliminate the main factor in its occurrence. That is, treatment of compression occurs in parallel and simultaneously with the treatment of intervertebral disc herniation, tumor, compression fracture, and so on.
Treatment may be medication. Patients are often prescribed painkillers and anti-inflammatory drugs to relieve pain and restore normal well-being. Drugs aimed at restoring blood flow and oxygen supply to the blood may also be prescribed. All medications should be prescribed only by your doctor. The dosage and frequency of use are very important. Self-medication can only harm and worsen the situation.
Treatment of compression can take place in other directions:
- physiotherapy;
- massage and manual therapy;
- physical therapy and special gymnastics.
When all of the above treatment methods do not produce an effect for a long time, the doctor considers the possibility and advisability of surgery. Surgeons, by making small incisions, can remove discs and tumors that are compressing the arteries. Treatment of compression should be carried out by doctors of several specializations: surgeons, therapists, neurologists, oncologists and others. You will find specialists in these and other areas at the Energo clinic. Our team consists of experienced professionals who, in their practice, have encountered various cases of compression of the vertebral artery and have positive experience in eliminating it.
The issues of prevention and treatment of osteochondrosis (OCS) of the spine are gaining special weight due to the progression of the number of patients in all countries of the world, its significant share in the structure of morbidity, disability and disability of the population. One of the leading clinical symptoms of OSC of the cervical spine (CSP) is ) appears to be vertebral artery syndrome (VA), which may have many pathogenetic mechanisms of formation. In ICD-10 there are several diagnoses that define damage to the vertebrobasilar region (VBB): M 47.0 – VA compression syndrome in spondylosis; M 53.0 – posterior cervical sympathetic syndrome; G 45.0 – syndrome of the vertebrobasilar arterial system. In recent years, the topics of diagnosis and treatment of PA syndrome have attracted increasing interest from doctors of many specialties: neurologists, neurosurgeons, vertebrologists, angiosurgeons, therapists, general practitioners, chiropractors, physiotherapists. Anatomy of PA . In order to present the pathogenesis of the formation of PA syndrome, it is necessary to have an understanding of the anatomy of this vessel. The PA supplies blood to a large area: segments of the spinal cord from C1 to Th3, including (superior medullary arterial basin), inner ear, brain stem structures (BS), occipital lobes, mediobasal areas of the temporal lobes, cerebellum, dorsal parts of the hypothalamic region. From the stellate ganglion, formed by the sympathetic centers of the C3–Th1 segments of the spinal cord, the spinal nerve emerges (posterior cervical sympathicus or Frank’s nerve). It penetrates the canal of the transverse processes, wrapping its branches around the PA. Additionally, branches depart from the vertebral nerve that take part in the formation of the Luschka nerve. This nerve innervates the capsular-ligamentous apparatus of the spine, the periosteum of the vertebrae and the posterior part of the intervertebral discs (IVD). A large proportion of the extracranial segment of the VA passes through the mobile bone canal formed by the transverse processes of the vertebrae. Moreover, the medial wall of the VA is adjacent to the uncovertebral joint, and the posterior wall borders the superior articular process. At the C1-C2 level, the VA is covered only by soft tissue, mainly by the inferior oblique muscle of the capitis. Etiology and pathogenesis . Some clinicians explain the clinical picture of PA syndrome in the case of spinal cord syndrome by compression of this vessel by bone growths of the vertebrae. This theory is based on multiple cases of traumatic injury to the VA or their ligation, followed by stroke in the VBB. However, further experimental and clinical studies have shown that compression of the VA alone cannot cause failure in the VSP. Only with congenital or acquired pathology of the VA (aplasia, abnormal narrowness, atherosclerosis, compression by osteophytes, hemodynamically significant stenotic lesions in the area of the VA orifices, occlusion of one of the VAs, vertebral-subclavian steal syndrome, etc.) can clinical failure of the compressed VA appear. The leading mechanism for the formation of VA compression syndrome seems to be extravascular edema due to mechanical compression, which leads to disruption of venous blood flow. Compression of the veins in the bone canal of the transverse processes of the spinal cord occurs earlier than the arterial one, and the venous outflow formed from compression of the veins in the bone canal aggravates the compression of the VA. Long-term irritation of the sympathetic plexus has been well studied in OSCC. Pathological irritation of this plexus during OSCC of the cervical spine causes spasm of the vessels of the VA system, which is clinically manifested by the dysfunction of the parts of the brain they supply with blood. The irritative type of PA syndrome is mainly recorded in young patients who do not have concomitant VBD pathology.
The etiological causes of PA syndrome can be divided into 3 types:
- Occlusive pathology of VA (atherosclerosis, thrombosis, embolism, arteritis).
- PA deformation (pathological tortuosity and deformation).
- Extravasal compression of the VA (compression by bone anomalies, ribs, muscles, IVD hernias, osteophytes and articular processes of the cervical vertebrae, scars, tumors, etc.).
According to various researchers, mechanical effects can cause PA:
1) bone growths of uncovertebral joints in 55.9% of cases;
2) bone growths of the facet joints (DOS) with spondyloarthrosis - 6.0%;
3) anterior-superior angle of the articular process with subluxation during extension (according to Kovach) in the spine - 25.0%;
4) anterior scalene muscle with a combination of scalenus syndrome with lateral origin of the VA orifice - 7.1%;
5) lateral hernia of the IVD, emerging through the uncovertebral fissure - 6.0%;
6) compression in the atlas region (Klippel-Feil anomalies, Kimmerli anomalies, platybasia);
Clinical picture . PA syndrome is clinically reflected by paroxysmal cephalgia (migraine type), dizziness, ataxia, nausea and/or vomiting, visual and auditory disorders, drop-attack episodes, syncope and hypothalamic attacks. Visual disturbances include the following: darkening in the eyes, a feeling of sand, sparks and other expressions of photopsia, slight changes in the tone of the fundus vessels (recorded in every 4-5 patients). Memory loss is more pathognomonic for individuals with pronounced organic changes. In approximately 60.0% of individuals, the syndrome is associated with certain movements or positions of the spinal cord, accompanied by an increase in VA compression. Of great importance in the formation of the clinical picture of PA syndrome is also concomitant pathology, such as atherosclerosis of the brachiocephalic arteries and cerebral arteries, arterial hypertension, coronary heart disease, etc. The diagnosis of PA syndrome is given to individuals who have a certain range of complaints and clinical syndromes that can be associated with OSCC or SHOP anomalies. Clinical variants of PA syndrome:
Barre-Lieu syndrome (posterior cervical sympathetic syndrome) . In most episodes, this syndrome is caused by arthrosis of the uncovertebral joints and subluxations according to Kovacs in the SHOP. Pain syndrome is associated with an earlier development of OSCC and pathological mobility in the cervical spine. It is characterized by cephalgia in the cervical-occipital region with spread to the front of the head (like “removing the helmet”). Cephalgia is combined with autonomic, cochleovestibular and visual disturbances.
Basilar migraine. It is characterized by visual disturbances on both sides, combined with dizziness, ataxia, dysarthria, and tinnitus. At the height of paroxysm, intense pain develops in the occipital region, combined with vomiting and, in some cases, loss of consciousness.
Vestibulo-atactic syndrome. Dizziness, a feeling of unsteadiness of the body, darkening of the eyes, imbalance with nausea and vomiting prevail. Symptoms progress when moving to the shopping center.
Cochleovestibular syndrome. It appears as noise in the ears or the back of the head, paresthesia, hearing loss, decreased perception of whispers, changes in the audiogram. These disorders are mainly combined with periodic non-systemic dizziness (a feeling of unsteadiness and staggering) or systemic dizziness.
Ophthalmic syndrome. Visual disorders are characterized by paroxysmal photopsia, atrial scotoma, fatigue and decreased vision when reading and other visual stress. Signs of conjunctivitis may be recorded: pain and a feeling of a foreign body in the eyes, redness of the conjunctiva, lacrimation. Cases of paroxysmal loss of visual fields are also recorded, often associated with the position in the SHOP.
Syndrome of autonomic disorders. The following vegetative symptoms are most often recorded: feeling of heat, chills, cold extremities, hyperhidrosis, changes in dermographism. Laryngopharyngeal disorders, as well as recurrent sleep and wakefulness disturbances, may occur.
Dropp-attack attacks . An episode of an unexpected fall is associated with ischemia of the caudal parts of the brainstem and cerebellum and appears in the form of tetraplegia with sudden extension in the spinal cord with rapid restoration of motor function.
Transient ischemic attacks.
Unterharnscheidt syndrome (syncopeal vertebrogenic syndrome) . It represents stroke in the reticular formation of the brainstem trunk, characterized by a short-term switching off of consciousness during rapid movement in the cervical spine or a prolonged forced position.
Diagnostics. To identify vertebrogenic PA syndrome, the presence of 3 clinical diagnostic criteria is necessary:
1. Clinical picture (presence of one of the nine clinical options described above or their combination).
2. The presence of changes diagnosed during MRI or CT in combination with functional spondylography of the spine (spondylosis in the area of uncovertebral joints, arthrosis of the joint joint, subluxation of the articular processes, instability and hypermobility in the spine, lateral hernias of the IVD, anomalies of the bone bed of the VA, craniovertebral junction, etc. .).
3. The presence of changes diagnosed when performing duplex scanning of the VA and/or when performing Dopplerography using functional tests with rotation, flexion and extension in the cervical spine (compression of the VA, asymmetry of the linear velocity of blood flow in the VA, vasospastic reactions in the VA and basilar arteries, hyperreactivity for functional tests, change in PA diameter).
Treatment. Conservative treatment includes: manual therapy, massage, acupuncture, physiotherapy, and spa treatment. According to modern understanding, neuroprotection is a complex of drug therapy aimed at compensating for the developing energy deficit of neurons, protecting them from the influence of damaging factors, activating neuroregeneration processes, and correcting blood flow in the brain. In PA syndrome, neuroprotection seems to be one of the most effective methods for preventing chronic cerebral ischemia, expressed as insufficiency in the VBB. The administration of neuroprotectors helps prevent the formation of metabolic disorders of the brain in individuals with an increased risk of ischemia, especially with a decrease in cerebrovascular reserve. Neuroprotection has the leading value in people with symptomatic stages of PA syndrome - stroke, transient ischemic attacks, syncopal vertebrogenic syndrome, dropp-attack attacks.
Rules for drug treatment of PA syndrome:
1. Drugs acting on venous outflow: semisynthetic diosmin (detralex, phlebodia), troxerutin, ginkgo biloba.
2. Nonsteroidal anti-inflammatory drugs: nimesulide, lornoxicam, celecoxib, Celebrex.
3. Drugs that normalize blood flow in the PA: pentoxifylline, vincamine, vinpocetine, cinnarizine, nimodipine, nicergoline, sermion, instenon.
4. Cholinergic drugs: citicoline, ceraxone, recognan, gliatilin.
5. Complex neuroprotective drugs: cytoflavin, actovegin, cerebrolysin, piracetam, mexidol
6.Metabolic therapy: cytoflavin, mildronate, thiotriazoline, trimetazidine
7. Symptomatic therapy - muscle relaxants: tolperisone, antispasmodics: drotaverine, histamine-like: betahistine, antimigraine: sumatriptan.
Complex conservative treatment includes orthopedic interventions on the source of pathology (cervical spine traction, cervical spine immobilization, manual therapy, etc.); novocaine blockade of spastically contracted and painful muscles of the spinal cord; physiotherapeutic and balneological methods.
Therefore, in the treatment of patients with PA syndrome, along with traditional conservative therapy, puncture methods of influence should be used: blockade of the PA, stellate ganglion, inferior oblique muscle of the head, dereception of the IVD and DOS.
Novocaine blockade of the sympathetic plexus of the PA is both diagnostic and therapeutic. The course includes 4-5 blockades at intervals every other day. The blockade technique is as follows: the patient was placed on his back with a bolster under his shoulders. Using the index finger of the left hand, push the carotid artery laterally, penetrating between it and the middle organs of the neck. The carotid tubercle of the transverse process of C6 is identified. After piercing the skin with a needle, they rest against the indicated tubercle, then, sliding off it, the needle falls through the intertransverse muscle, i.e., into the PA canal. An aspiration test ensures that there is no damage to the vessel. Then 3-5 ml of a 2% novocaine solution is injected. After performing the manipulation, the patient should lie on his back for 20 minutes so that the anesthetic does not spread through the perineural spaces to the stellate ganglion.
At the same time, with pathological impulses from the affected DOS, a persistent or intermittent spasm of the VA occurs. The main advantage of chemical denervation of the DOS over more local influences (laser vaporization, cold plasma coblation, high-frequency destruction) is that the alcohol-vocaine solution turns off a larger number of nociceptive vegetative structures around the DOS, including branches of the Luschka nerve, which play a major role in the formation of reflex syndromes facet syndrome SHOP.
The first minimally invasive methods were chemonucleolysis, IVD dereception and percutaneous nucleotomy. Chemonnucleolysis and dereception of the IVD lead to the development of fibrosis of the nucleus pulposus of the IVD with the creation of conditions for ankylosis of the spinal motor segment at various stages of its dystrophic lesion. The development of fibrosis of the IVD limits the range of movements in the operated segment, while the minimum range of movements that does not lead to local overload of adjacent spinal motion segments is not excluded. The process of IVD restructuring after chemonucleolysis is long and takes 1.5-2 years, which can lead to the development of relapse of the disease.
For vertebrogenic PA syndrome, the following operations are performed:
- decompressive and stabilizing - uncusectomy with ventral interbody fusion;
- decompressive-plastic - transdiscal decompression of the VA;
- decompressive - extradiscal uncusectomy and arteriolysis, resection of abnormal rings of the C1 vertebra, resection of the cervical rib and arteriolysis, etc.;
- stabilizing operations for dynamic compression of the VA;
- laser vaporization of IVD for reflex syndrome of PA and IVD protrusion.
A distinctive feature of surgical treatment of persons with VA syndrome is determined by the frequent combinations of vertebrogenic lesions of the VA with their atherosclerotic or congenital pathology (32.0% of patients), as well as with occlusive and stenotic lesions of the carotid arteries (26.7-28.0%). This indicates the need for precise preoperative examination of these individuals and comprehensive treatment. In patients with combined lesions of the VA and carotid arteries, the first stage is reconstruction of the carotid system.
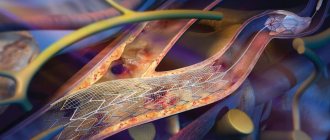
Reconstruction of V1 VA is advisable to apply with intact distal segments (V2-4). When identifying atherosclerotic lesions of the VA in the V1 segment, the following reconstructive operations are performed:
- transposition of the VA into the internal carotid artery;
- transposition of the VA into the common carotid artery;
- transposition of the VA into the subclavian artery;
- transposition of the VA into the thyrocervical trunk;
- modified transposition (replantation) of the VA mouth;
- endarterectomy and angioplasty of VA;
- arteriolysis and desympathization of PA.
Indications for VA reconstruction in the V3 segment:
1) stenosis or occlusion of the V1 and V2 segments of the VA with an open circle of Willis;
2) extravasal compression of the V2 segment of the VA with an open circle of Willis;
3) upcoming reconstruction on the V1 segment of the VA or carotid-subclavian anastomosis;
4) stent fracture or severe restenosis (if repeated stenting is not possible) after stenting of the V1 segment of the VA.
Access to the V3 segment of the VA (between the transverse processes of C1-2) has several advantages: the location of the VA in this area is the most superficial, the ability to perform dissection of the VA without bone resection at a prolonged distance, and the venous plexus in this area is less pronounced than in others.
In case of atherosclerotic lesions of the VA in the V3 segment, the following reconstructive operations are performed:
- transposition of the VA into the internal carotid artery;
- general-distal spinal bypass surgery;
- external carotid-distal spinal shunting;
- intracarotid-distal spinal shunting;
- external carotid-distal spinal anastomosis;
- occipito-distal spinal anastomosis;
- subclavian-distal vertebral bypass surgery.
Conclusion. The clinical picture of PA syndrome does not always have a classic picture, and the most stable signs are cephalalgia, dizziness and tinnitus. The effectiveness of treatment of PA syndrome is inextricably linked with the timely diagnosis of this disease. A comprehensive impact on the possible pathogenetic mechanisms of the formation of PA syndrome is necessary. Conservative treatment of people with PA syndrome can reduce the severity and frequency of clinical symptoms. Minimally invasive methods of treating PA syndrome should take their rightful place in the arsenal of a vertebrologist, neurosurgeon and neurologist. Reconstructive operations on VA for atherosclerotic lesions in specialized departments (vascular surgery and neurosurgery) should also be more widely used. There is also a need for greater awareness among primary care physicians about this disease and how to diagnose and treat it.
Disease prevention
Extravasal compression of the vertebral artery is such a serious disorder that it is easier and better to prevent it than to treat it later. Treatment usually takes a long time, while prevention consists of simple things:
- active lifestyle and giving up bad habits;
- regular exercise (you don’t have to go to the gym for this, you can just do morning jogging or light exercise);
- massage aimed at improving blood flow, strengthening muscles, restoring their tone.
All of the listed preventive measures, observed in combination, will certainly give a positive result and will help to avoid not only compression of the vertebral arteries, but also other problems with the musculoskeletal system, nervous system, heart and vascular system, and so on.
Treatment measures
The most important task in treatment is to replenish the blood supply with further elimination of causative factors. Typically, therapy involves taking medications in combination with physical therapy measures.
Patients are often prescribed nonsteroidal anti-inflammatory drugs, which are accompanied by analgesic and anti-inflammatory effects. In addition, drugs are used to relieve swelling and replenish blood supply.
In the process of selecting pharmaceuticals, the patient must have a clear understanding of the state of his health. Treatment and signs of extravasal compression of both vertebral arteries are very important. The slightest mistakes in choosing medications can lead to irreparable consequences.
- Hypoplasia of the left vertebral artery: what is it, causes and treatment features
As for physiotherapeutic techniques, the following procedures are effective:
- massage,
- physiotherapy,
- acupuncture,
- visiting a physiotherapy room.
If your health suddenly worsens, then you must inform your leading doctor about this so that he can adjust subsequent therapy.
If all of the above methods do not have the desired effect, and the condition does not change in any way, then you may be offered surgery.
At the end of the treatment course, patients are advised to visit a medical and preventive sanatorium to undergo a course of rehabilitation treatment. This will help to quickly recover and improve the patient’s general well-being.