Stenosing atherosclerosis is a chronic vascular disease in which the lumen of the vessel narrows due to the formation and increase in size of atherosclerotic plaques. The disease is accompanied by pathological changes in the structure of the walls of the affected vessel, as well as impaired nutrition and oxygen supply to the surrounding soft tissues. The main reason for the development of atherosclerosis is a high level of cholesterol in the blood, which is gradually deposited on the walls of blood arteries in the form of fatty plaques, narrowing their lumen and disrupting normal blood circulation. The disease is diagnosed mainly in patients aged 50–55 years. Timely detection of such vascular pathology makes the prognosis for successful treatment as favorable as possible.
Difference between stenosing and non-stenosing atherosclerosis
Atherosclerosis is a chronic vascular disease that develops with age, and all people are susceptible to it. At the initial stage, the plaques in the vessels are small, but if they do not block the vessel by more than half, this condition is called non-stenotic atherosclerosis. In this case, there are simply no signs of atherosclerosis, and the person feels great. As the cholesterol plaque grows, the vascular lumen becomes blocked—arterial stenosis occurs. In this case, organs deprived of the usual amount of oxygen and nutrients suffer from ischemia. This explains why the diagnosis of “stenotic atherosclerosis” occurs mainly in older and elderly people.
How does atherosclerosis of the arteries of the lower extremities manifest?
The article was prepared by cardiologist Ksenia Nshanovna Borel
Are you worried about pain in your legs? Surely the majority will answer in the affirmative. Did you know that atherosclerosis of the arteries of the lower extremities can also be accompanied by pain in the legs? Let's discuss this in more detail so as not to miss the symptoms of a rather formidable disease.
Atherosclerosis is a chronic and progressive systemic disease that affects arteries of any location. If, after reading this text, you suspect that you have similar symptoms, consult a doctor and conduct a comprehensive comprehensive examination so as not to miss damage to the arteries and other locations (heart, carotid arteries, arteries of the upper extremities).
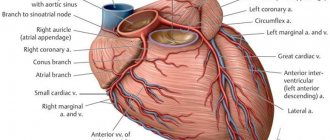
The substrate of atherosclerosis is an atherosclerotic plaque, which is plus tissue that narrows the lumen of any artery. This means that the diameter of the artery determines the speed at which symptoms appear, i.e. It is quite natural that the smaller the diameter of the artery, the more pronounced the manifestation of atherosclerosis.
Damage to the arteries of the lower extremities is indicated when any artery extending below the origin of the renal arteries from the aorta is involved in the pathological process.
The arteries supplying blood to the lower extremities are quite large vessels in size and diameter, because their job is to deliver an adequate volume of arterial blood to supply a large array of muscle tissue of the legs (gluteal muscles, thigh muscles and lower legs). Any arteries of the human body in the direction from the center to the periphery decrease in diameter, i.e. The lower leg and foot are supplied with blood by smaller vessels than the thigh muscles.
That is, with atherosclerotic lesions of the arteries of the lower extremities, the symptoms are ascending in nature - from the periphery to the center: the first signs of the disease are manifested by pain in the muscles of the feet and legs.
Risk group
Atherosclerotic damage to the arteries of the lower extremities occurs more rapidly at older ages, in patients with diabetes mellitus, high cholesterol levels, arterial hypertension, and more often in men who smoke.
The worst prognostic factors for the risk of atherosclerosis of the arteries of the lower extremities are male gender, smoking, especially heavy smoking, and lipid metabolism disorders.
It has been scientifically proven that addressing modifiable risk factors can improve the situation: in particular, quitting smoking improves the prognosis of patients. The duration and severity of diabetes mellitus also worsens the condition of the blood vessels of the lower extremities.
Symptoms and signs of atherosclerosis
What symptoms should alert you? Patients may complain of fatigue, cramps, chilliness of the legs (frequent feeling that the legs are cold, despite the ambient temperature), pallor of the skin of the legs, thinning of the hair on the legs, deterioration of the nails.
Dear men, remember that erectile dysfunction is the first and very early symptom of atherosclerosis. Because the artery supplying blood to the penis is the narrowest artery in the male body.
The main and specific symptomatology of atherosclerosis of the lower extremities is intermittent claudication, or Leriche syndrome. The name of the symptom very eloquently describes the essence of the complaint: when walking at a certain pace or a certain distance, the patient experiences pain in the leg muscles, which alternates with normal exercise tolerance. For comparison: with venous diseases, pain appears at rest, towards the end of the day, and often disappears after a little physical activity.
The severity of intermittent claudication varies, but the main feature is that pain occurs while walking - at different distances and at different paces, and the pain stops when you stop. The cause of these symptoms is a discrepancy between the needs of blood volume and its supply: any physical activity means an increased consumption of oxygen and blood in order to provide working muscles with nutrients.
Stages of arterial insufficiency
Depending on the tolerated physical activity, several stages of arterial insufficiency are distinguished with intermittent claudication.
Test yourself:
- Do muscle pain appear when walking 1000 meters or more? Stage 1
- Do muscle pain appear when walking more than 200 meters? 2a stage
- Do muscle pain appear when walking up to 200 meters? 2b stage
- Do muscle pain appear at rest and/or in a horizontal position? Stage 3
- limb gangrene? Stage 4
Diagnosis of atherosclerosis of the arteries of the lower extremities
Careful questioning and examination of the patient allows one to diagnose with great accuracy damage to the arteries of the lower extremities: it is very important to palpate the pulse in the arteries of the feet, assessing the strength of the pulse wave and its symmetry.
In addition, auscultation is performed in the projection of the femoral arteries (on the anterior surface of the thigh, under the inguinal ligament): if there is noise here, the patient not only with a high degree of probability can indicate the presence of atherosclerosis of the arteries of the lower extremities, but also announce 2 times more high myocardial infarction and cardiovascular mortality.
This once again indicates the systemic nature of the lesion: in any patient with angina pectoris or a history of myocardial infarction, the arteries of the lower extremities should be examined and vice versa.
If, based on any objective signs, the doctor suspects that you have peripheral artery disease, then these assumptions will need to be confirmed objectively:
- To determine the amount of physical activity tolerated, it is recommended to perform a treadmill test: walking on a treadmill that changes speed and incline.
- Ultrasound of the arteries of the lower extremities is considered a routine screening diagnostic method, inexpensive, accessible and does not require expensive equipment.
- The gold standard for diagnostics is computed angiography.
- MRI of the arteries of the lower extremities
Treatment of arterial atherosclerosis
Drug and non-drug correction should be aimed at quitting smoking, normalizing blood pressure and blood sugar levels (if the patient suffers from diabetes). Sometimes medications are prescribed to help dilate the arteries and prevent additional “gluing” of red blood cells and platelets.
The patient must be prescribed statins: according to studies, these drugs improve not only the long-term prognosis, but also help increase the maximum distance traveled by 50-100 meters.
Treatment strategies are determined in each case individually. However, the only radical method of correction is surgical restoration of blood flow in the affected limb. As a rule, these are minimally invasive procedures (endovascular interventions, or stenting) or more traumatic (bypass surgery or prosthetics).
The last stage of treatment is amputation of the affected lower limb. This method is used only in situations of acute ischemia of a limb or in a situation where it is not possible to save the affected limb or the situation is life-threatening (for example, in the presence of gangrene).
This is a rather ominous sign for determining a further favorable prognosis for patients. Thus, studies were conducted with patients who had undergone amputation, who were followed for 2 years after the procedure. The results were very disappointing: after amputation of the lower leg within 2 years, 30% died, 15% suffered amputation of the hip, 15% had amputation of the other limb.
When it comes to the problem of atherosclerosis of the arteries of the lower extremities, the expression “better to prevent than to treat” is more justified than ever. The most eloquent confirmation of this is the statistics of long-term prognosis after amputation.
SIGN UP FOR AN ULTRASOUND
Consequences
Among the causes that provoke various diseases of the blood vessels of the legs, heart, and brain, stenosing atherosclerosis occupies a leading position.
- If the coronary vessels are affected, symptoms of cardiac ischemia occur. Coronary heart disease makes itself felt by chest pain and shortness of breath during exercise. This diagnosis ends with myocardial infarction. Every year, thousands of people are admitted to cardiology hospitals in Moscow due to atherosclerosis of the heart vessels.
- When stenosing atherosclerosis affects the arteries of the vascular system of the legs, obliterating atherosclerosis of the lower extremities occurs - a disease that threatens disability and amputation of the limb.
- Atherosclerotic plaques in the vessels supplying the kidneys lead to the development of renovascular hypertension and renal dysfunction.
- If the neck vessels narrow and the arteries supplying blood to the brain (BCA - brachiocephalic arteries) are blocked, stenosis in the damaged area leads to cerebral ischemia and stroke. Read more about stenosing atherosclerosis of the brachiocephalic arteries and its consequences in the following publication.
Diagnostics
A neurologist deals with cerebral atherosclerosis. His task is to collect anamnesis, as well as conduct a series of tests. Doctor:
- will ask you to look up (a sick person will not be able to fulfill the request);
- will check the reflexes (they will be either excessively high or low, and asymmetrically);
- will ask you to stretch your arms forward and look to see if there is any tremors in the fingers, or if the patient is losing balance;
- will ask you to touch your nose with the tip of your finger with your eyes closed (the patient will not be able to cope with this task).
This is only a small component for assessing the patient’s health. Therefore, more detailed examinations are required next:
- consultation with an ENT doctor, ophthalmologist and other specialists depending on the identified disorders;
- biochemical blood test for triglycerides and cholesterol (lipid spectrum);
- According to indications, instrumental examinations are carried out.
To assess the condition of cerebral vessels, the following is carried out:
- Ultrasound of the brain and neck using two-dimensional and transcranial duplex scanning technology;
- angiography of cerebral vessels;
- Doppler ultrasound;
- MRI of the brain in vascular mode;
- REG (radioencephalogram);
- CT computed tomography of the brain and blood vessels;
- EEG – electroencephalogram.
The diagnostic capabilities of our multifunctional center of the FMBA of Russia allow us to carry out not only these, but also any other examinations necessary for the patient using the most modern and accurate equipment. You will be able to get advice from related specialists on any clinical case, including suspected cerebral atherosclerosis.
Risk factors
In addition to the age-related changes in the condition of blood vessels that we have already mentioned, atherosclerosis is caused by factors associated with a person’s habits and lifestyle. Smoking, alcohol abuse or fatty foods increase the risk of developing atherosclerosis. Nicotine causes vascular spasms, and alcohol and junk food increase cholesterol levels, which contributes to the formation of atherosclerotic plaques. People who lead a sedentary lifestyle are at risk. Among the causes of coronary heart disease and other vascular diseases, hereditary predisposition is also noted.
Treatment
In the early stages of the disease, drug treatment aimed at preventing the development of atherosclerotic plaques and improving the rheological properties of blood is acceptable. For this purpose, statins and antiplatelet agents (aspirin) are used.
If the lumen of the vessel is so closed that the blood supply to the limb is disrupted, surgical treatment is necessary:
- balloon dilatation and stenting of the vessel (expansion of the narrowed part and installation of a stent to prevent re-narrowing of the lumen),
- endarterectomy (removal of plaque with the inner layer of the vessel),
- shunting (creating bypass paths for blood flow around an irreversibly damaged area of the vessel).