Temporal (giant cell) arteritis is a chronic inflammatory process that occurs as a result of a malfunction of one’s own immune system, affecting various arteries. Another name for this disease is Horton's disease. It received this name thanks to the doctor who described the pathology in detail.
The exact cause of temporal arteritis is currently unknown. But there is an opinion that its appearance is facilitated by the aging of the body. The fact is that with age, the walls of the temporal and ophthalmic arteries and veins become less elastic, which is why immune inflammation occurs. Since this disease affects the visual system, in rare cases, lack of treatment can cause complete blindness.
Also, according to some experts, Horton's disease has some genetic predisposition. Most often women are susceptible to it.
The disease has two forms - primary and secondary. In primary temporal arteritis, it occurs independently. This form develops due to age-related changes, usually in people over 50-60 years old. The secondary form indicates the occurrence of another disease, which is a catalyst for inflammation. Most often this concerns infectious diseases in a severe stage. The most dangerous among such infections are Staphylococcus aureus and the hepatitis virus.
Temporal or giant cell arteritis - what is this disease?
Temporal arteritis is a type of vasculitis and is an autoimmune inflammation that affects large and medium arterial vessels. Mostly with this pathology, the ophthalmic, temporal and vertebral arteries are affected. This disease has several names: Horton's disease, giant cell temporal and temporal arteritis. Pathology was first named after the doctor who first described it in the 30s of the 20th century. The disease is called temporal arteritis because it almost always affects the temporal artery and is characterized by severe pain in the temples.
The pathology is common among Scandinavians and residents of northern Europe. According to statistics, per 100 thousand people there are on average 25 people with Horton's disease. Among Asians, Japanese and the population of Arab countries, arteritis is much less common (no more than 2 cases per 100 thousand people).
The disease mainly affects older people over 50 years of age, with the peak of pathology occurring at 70 years of age. Females suffer from temporal arteritis more often than males.
Giant cell arteritis - what causes it?
The autoimmune nature of the disease means that inflammation is caused by disruptions in the functioning of the human body's own immune system. The exact causes of the disease have not yet been established, but it is assumed that influenza, herpes, and hepatitis viruses can trigger the disease. Horton's disease often develops after infectious diseases. It is assumed that pathogenic microorganisms can change antigens in the cells of our body, thereby turning them into foreign ones for our immunity. To combat changed cells, the body’s defense system produces antibodies that can attach to the vascular walls and have a destructive effect on them. Thus, foci of inflammation are formed in the arterial vessels, where cellular accumulations occur.
A number of scientists are inclined to believe that the disease may have genetic background: it has been established that many patients are carriers of the same genes.
Symptoms of temporal arteritis
A diagnosis performed by a doctor can accurately determine that a patient has temporal arteritis. The reason for contacting a specialist can be three categories of symptoms - general, vascular and visual.
- General symptoms.
With arteritis, you may experience fever, fatigue, poor sleep, weight loss, and pain in the muscles and joints. A characteristic symptom is severe headache, mainly in the temporal zone. It can spread to one or both halves of the skull, is accompanied by pulsation, and intensifies at night. The intensity of the headache may increase as the disease progresses. Sometimes there is soreness of the skin in the head area, numbness in the facial area, and pain when chewing.
- Vascular symptoms.
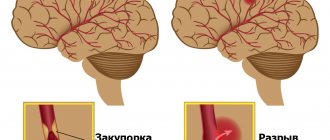
With this pathology, the arteries in the area of the temples and the crown of the head become denser, more painful, and are easily detected by palpation. As the pathology progresses, these arterial vessels stop pulsating. If the internal carotid artery is damaged, the patient may experience an ischemic stroke - blood circulation in the brain area is disrupted, which leads to tissue damage and, as a result, disruption of brain functions. Less commonly, arteritis causes damage to other large arterial vessels with similar symptoms.
- Symptoms from the visual apparatus.
Characteristic signs of the disease are also various eye lesions. In particular, with arteritis, there is a disruption of the blood supply in the arterial vessels, which are located next to the eyeball and are connected to the optic nerve. As a result, a person may notice a sharp deterioration in vision, especially peripheral vision, and loss of visual fields. In 30% of cases, vision deteriorates in both eyes. Other symptoms may also occur: double vision, pain, and blurred images. If you notice such signs, you should consult a doctor as soon as possible.
Experts say that irreversible damage to the optic nerve occurs several months after the onset of the disease. Therefore, if temporal arteritis is diagnosed as early as possible and treatment is started on time, the patient’s vision can be saved.
Causes
Not a single theory of the origin of the disease has been reliably confirmed.
Presumably, the infectious factor plays an important role in its development. There is often a natural connection between the occurrence of arteritis and previous influenza and group B hepatitis. The genetic programming of pathology also has its supporters. Cases of this rather rare disease have been observed in close relatives and identical twins. The leading role in the formation of inflammation of the vascular wall belongs to immunological disorders, and this is recognized by adherents of all etiological concepts. With temporal arteritis, the immune system reacts inadequately to its own tissues - the process proceeds as an autoimmune one.
How is the disease diagnosed?
Since Horton's disease causes symptoms from both the visual and vascular systems, many people have a question: which doctor should conduct a diagnostic examination?
Usually, if temporal arteritis is suspected, a comprehensive diagnosis is carried out, which includes an examination by a therapist, an examination by an ophthalmologist and a neurologist, and a series of laboratory, ultrasound and other studies.
Blood tests in patients with arteritis often show an increase in the number of leukocytes, hypochromic anemia, and an increase in ESR. During the examination, the ophthalmologist may detect decreased visual acuity, diplopia, narrowing of the visual fields, and changes in the fundus. During a neurological examination and additional examinations (ultrasound diagnostics of blood vessels, magnetic resonance and computed tomography of the brain, angiography of cerebral vessels), the presence of vascular pathologies can be determined. The results of a biopsy of the temporal artery in the presence of disease may show thickening of the walls of blood vessels, the formation of nodules and giant cells in them, the appearance of blood clots and a narrowed lumen of the artery. But sometimes a biopsy does not give a characteristic picture even in the presence of the disease. This is explained by the fact that the arteries are affected not along their entire length, but in separate segments and, accordingly, the study can be carried out on an undamaged area, which gives a false negative test result.
The American Rheumatological Association has adopted a number of diagnostic criteria for temporal arteritis. This list includes:
- age over 50 years;
- specific nature of the headache;
- pathological disorders of the temporal arterial vessels;
- ESR level in the blood exceeding 50 mm/h;
- Typical results for Horton's disease are the results of a histological examination of material obtained from a biopsy of the temporal artery.
If a patient has at least three of the five listed signs, he will be diagnosed with giant cell arteritis.
Forecast
Temporal arteritis is a serious disease. If not recognized in a timely manner and treated inadequately, the pathology poses a threat to the health and life of the patient. A timely diagnosis and compliance with doctors’ recommendations avoid complications and make the prognosis favorable.
In our department of vascular surgery, a full examination, qualified interpretation of the results obtained and professional implementation of all types of treatment measures are possible.
How is Horton's disease treated?
If a patient is diagnosed with temporal arteritis, treatment should begin immediately. As a rule, it is prescribed and performed by a rheumatologist. The goal of therapy is to stop the incorrect functioning of the immune system, which causes vascular damage. For this purpose, glucocorticosteroid drugs are prescribed. At the initial stage, the patient is prescribed hormones in a dose that is comparable to the level of vascular damage and complications from the visual apparatus. If during the diagnostic process a sharp, acute drop in vision is detected, then so-called pulse therapy can be prescribed - short-term administration of ultra-high doses of corticosteroids to the patient. A month or later from the start of treatment (at the discretion of the doctor), the dose is gradually reduced to maintenance. Typically, the duration of therapy for giant cell arteritis is two years. The doctor may cancel treatment if there are no signs of illness within six months of maintenance therapy.
If treatment with corticosteroid hormones does not bring the expected results or the patient experiences serious side effects, the doctor may alternatively prescribe cytostatic drugs that block or slow down cell growth. Symptoms of the disease are treated with anti-inflammatory, vasodilating medications and anticoagulants.
Temporal arteritis affects mainly older people who suffer, among other things, from other chronic diseases when there are age-related metabolic disorders. To ensure that the therapy does not harm the condition of other organs and systems, during the treatment process the doctor monitors the liver function and the level of the patient’s mineral metabolism in order to notice signs of osteoporosis or liver failure in time. Also, in parallel with treatment, prevention of duodenal and gastric ulcers is carried out, and blood sugar levels are monitored. If the patient develops acute thrombosis in the affected area, the specialist may prescribe surgery.
You need to understand that it is currently impossible to completely cure an autoimmune disease. However, timely initiation and properly selected therapy blocks or significantly slows down the inflammation process, helping to prevent dangerous complications in the form of strokes, heart attacks, and complete loss of vision.
The prognosis for improvement in vascular condition and preservation of visual function is favorable if therapy is started at an early stage. Therefore, you should not put yourself at risk and delay a visit to the doctor if you often have a headache in the temporal region, double vision, or other signs of Horton’s disease.
Treatment
Once Horton's temporal arteritis has been diagnosed, the person should be immediately treated with the drug cortisone . For the first four weeks, a dosage of one milligram of prednisolone per kilogram of body weight is recommended. If symptoms have resolved due to therapy and blood levels of inflammation have returned to normal, the dose should be continuously reduced. If symptoms recur, more prednisolone should be taken again. The attending physician will work with the patient on a precise treatment schedule. If blindness is inevitable, prednisolone therapy should be given in large doses through a vein over three to five days.
Because cortisone therapy can cause many unwanted side effects, it is necessary to take additional medications. Calcium and vitamin D reduce the risk of osteoporosis (brittle bones). In case of possible vascular occlusions, aminosalicylate (for example, aspirin) should be taken. Proton pump inhibitors protect the gastric mucosa. In addition, your blood sugar levels should be checked regularly and adjusted if necessary.