Temporal or giant cell arteritis - what is this disease?
Temporal arteritis is a type of vasculitis and is an autoimmune inflammation that affects large and medium arterial vessels. Mostly with this pathology, the ophthalmic, temporal and vertebral arteries are affected. This disease has several names: Horton's disease, giant cell temporal and temporal arteritis. Pathology was first named after the doctor who first described it in the 30s of the 20th century. The disease is called temporal arteritis because it almost always affects the temporal artery and is characterized by severe pain in the temples.
The pathology is common among Scandinavians and residents of northern Europe. According to statistics, per 100 thousand people there are on average 25 people with Horton's disease. Among Asians, Japanese and the population of Arab countries, arteritis is much less common (no more than 2 cases per 100 thousand people).
The disease mainly affects older people over 50 years of age, with the peak of pathology occurring at 70 years of age. Females suffer from temporal arteritis more often than males.
Prognosis, possible complications
If treatment is carried out at the initial stage of the disease, the prognosis is favorable. Steroid therapy will help block arteritis and get rid of negative symptoms. Laboratory parameters gradually normalize, the condition of the vascular walls improves, and blood flow is restored.
Since the disease is autoimmune in nature, it cannot be completely cured. Without treatment, complications are possible:
- blurred vision, blindness;
- the disease enters the chronic stage;
- arterial thrombosis;
- angina pectoris;
- formation of ischemic areas in the brain;
- formation of necrotic areas;
- neurological and mental disorders.
Important! Properly selected therapy will help eliminate the disease in time, eliminating the risk of heart attack, blindness, and stroke.
Giant cell arteritis - what causes it?
The autoimmune nature of the disease means that inflammation is caused by disruptions in the functioning of the human body's own immune system. The exact causes of the disease have not yet been established, but it is assumed that influenza, herpes, and hepatitis viruses can trigger the disease. Horton's disease often develops after infectious diseases. It is assumed that pathogenic microorganisms can change antigens in the cells of our body, thereby turning them into foreign ones for our immunity. To combat changed cells, the body’s defense system produces antibodies that can attach to the vascular walls and have a destructive effect on them. Thus, foci of inflammation are formed in the arterial vessels, where cellular accumulations occur.
A number of scientists are inclined to believe that the disease may have genetic background: it has been established that many patients are carriers of the same genes.
1.General information
The group of inflammatory processes affecting the walls of blood vessels (vasculitis, angiitis, arteritis) still, unfortunately, remains a blank spot in modern medical knowledge. More precisely, vasculitis is the object of the most thorough and intense research around the world, since it may contain the key (or one of the keys) to autoimmune diseases in general - to an etiopathogenetically unclear, to date, class of diseases in which the body begins to destroy by myself.
Why this particular organ is targeted, and not this one, why people of one gender predominate among the sick, why this or that autoimmune disorder most often begins at a certain age - nature gives all these mysteries extremely reluctantly, as if it is ashamed of cases of such “betrayal” from the outside. so verified and fine-tuned during the evolution of the immune system. The only relative consolation (and even then not for patients) is the rarity of such diseases; However, researchers are receiving increasing evidence that many more diseases are autoimmune in nature than was previously accepted.
Symptoms of temporal arteritis
A diagnosis performed by a doctor can accurately determine that a patient has temporal arteritis. The reason for contacting a specialist can be three categories of symptoms - general, vascular and visual.
- General symptoms.
With arteritis, you may experience fever, fatigue, poor sleep, weight loss, and pain in the muscles and joints. A characteristic symptom is severe headache, mainly in the temporal zone. It can spread to one or both halves of the skull, is accompanied by pulsation, and intensifies at night. The intensity of the headache may increase as the disease progresses. Sometimes there is soreness of the skin in the head area, numbness in the facial area, and pain when chewing.
- Vascular symptoms.
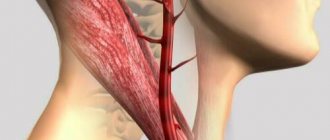
With this pathology, the arteries in the area of the temples and the crown of the head become denser, more painful, and are easily detected by palpation. As the pathology progresses, these arterial vessels stop pulsating. If the internal carotid artery is damaged, the patient may experience an ischemic stroke - blood circulation in the brain area is disrupted, which leads to tissue damage and, as a result, disruption of brain functions. Less commonly, arteritis causes damage to other large arterial vessels with similar symptoms.
- Symptoms from the visual apparatus.
Characteristic signs of the disease are also various eye lesions. In particular, with arteritis, there is a disruption of the blood supply in the arterial vessels, which are located next to the eyeball and are connected to the optic nerve. As a result, a person may notice a sharp deterioration in vision, especially peripheral vision, and loss of visual fields. In 30% of cases, vision deteriorates in both eyes. Other symptoms may also occur: double vision, pain, and blurred images. If you notice such signs, you should consult a doctor as soon as possible.
Experts say that irreversible damage to the optic nerve occurs several months after the onset of the disease. Therefore, if temporal arteritis is diagnosed as early as possible and treatment is started on time, the patient’s vision can be saved.
Etiology
The causes of giant cell arteritis currently remain unknown. The pathology is based on autoimmune inflammation. Age-related changes that occur in the walls of blood vessels lead to a loss of their elasticity, which further aggravates the situation and contributes to the development of the disease.
There are several theories for the development of arteritis:
- Hereditary predisposition - this disease is often found in members of the same family and almost always in identical twins.
- Infectious theory - the presence of antibodies and antigens in the blood of people who have had influenza, staphylococcal infection, or hepatitis.
- Autoimmune theory, according to which Horton's syndrome is classified as collagenosis. Foreign formations provoke the production of antibodies that attack the vessel’s own tissues. In some patients with arteritis, the same signs of damage to the connective tissue and blood vessels were revealed as in periarteritis nodosa. Arteritis often occurs in patients with systemic lupus erythematosus, dermatomyositis, and scleroderma.
Temporal arteritis primarily affects large blood vessels, affecting capillaries only in rare cases. Inflammation of the vascular wall leads to disruption of tissue structures, narrowing of the lumen of the vessel, organ ischemia, deterioration of local blood flow, and the formation of a blood clot that completely blocks the lumen. Thinned and stretched walls of arteries or veins protrude, an arterial aneurysm develops, which, against the background of a sharp increase in blood pressure, can rupture.
The clinical picture of the disease is determined by the localization of the lesion. Patients develop acute cerebrovascular accident, loss of vision, and stroke. Typically, inflammation occurs in the carotid arteries, aorta and other vascular structures that supply blood to areas of the head and cerebral cortex, the optic nerve, the organ of vision, and some internal organs.
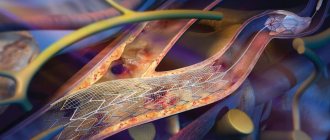
artery changes in giant cell arteritis
Inflammation in arteritis is focal or segmental in nature: the vessels are not affected along their entire length, but in individual areas or segments. The elastic membrane is infiltrated by lymphocytes, the intima thickens, plasma cells, epithelial cells, histiocytes, and multinucleated cells accumulate in it, forming extensive granulomas. Multinucleated giant cells are complexes circulating in the blood that give the disease its name.
In the blood of patients with exacerbation of arteritis, a large number of immune complexes, lymphoblasts, and serum immunoglobulins are found.
Video: temporal arteritis – medical animation
How is the disease diagnosed?
Since Horton's disease causes symptoms from both the visual and vascular systems, many people have a question: which doctor should conduct a diagnostic examination?
Usually, if temporal arteritis is suspected, a comprehensive diagnosis is carried out, which includes an examination by a therapist, an examination by an ophthalmologist and a neurologist, and a series of laboratory, ultrasound and other studies.
Blood tests in patients with arteritis often show an increase in the number of leukocytes, hypochromic anemia, and an increase in ESR. During the examination, the ophthalmologist may detect decreased visual acuity, diplopia, narrowing of the visual fields, and changes in the fundus. During a neurological examination and additional examinations (ultrasound diagnostics of blood vessels, magnetic resonance and computed tomography of the brain, angiography of cerebral vessels), the presence of vascular pathologies can be determined. The results of a biopsy of the temporal artery in the presence of disease may show thickening of the walls of blood vessels, the formation of nodules and giant cells in them, the appearance of blood clots and a narrowed lumen of the artery. But sometimes a biopsy does not give a characteristic picture even in the presence of the disease. This is explained by the fact that the arteries are affected not along their entire length, but in separate segments and, accordingly, the study can be carried out on an undamaged area, which gives a false negative test result.
The American Rheumatological Association has adopted a number of diagnostic criteria for temporal arteritis. This list includes:
- age over 50 years;
- specific nature of the headache;
- pathological disorders of the temporal arterial vessels;
- ESR level in the blood exceeding 50 mm/h;
- Typical results for Horton's disease are the results of a histological examination of material obtained from a biopsy of the temporal artery.
If a patient has at least three of the five listed signs, he will be diagnosed with giant cell arteritis.
Giant cell arteritis (GCA) is one of the most common forms of primary systemic vasculitis - immune-mediated diseases of unknown etiology that cause inflammatory, including productive (granulomatous), as well as necrotic damage to the vascular wall [1-5]. GCA is a granulomatous vasculitis of large and medium-sized vessels, predominantly craniofacial, including precerebral and cerebral arteries. Like other forms of systemic vasculitis, GCA is characterized by a progressive course, leading to early or late death if untreated.
The main clinical manifestations of GCA are caused by isolated or combined damage to the arteries of three vascular systems: 1) branches of the external carotid artery, in most cases its thin terminal branch - the superficial temporal artery; 2) branches of the internal carotid artery, often the ophthalmic artery; 3) the aorta and/or its large branches, also brachiocephalic arteries, often the vertebral artery.
Damage to precerebral and cerebral arteries caused by GCA can lead to the development of ischemic cerebral disorders - one-sided blindness and stroke (in many cases associated with delayed diagnosis of GCA). The incidence of late diagnosis of GCA (due to an erroneous diagnosis of another disease) is quite high. In this regard, the greatest importance in the practice of a neurologist is to identify the initial neurological manifestations of GCA, justifying the immediate prescription of glucocorticoids.
Epidemiology
It is believed that GCA is a disease that does not occur in people under 50 years of age and develops exclusively in middle-aged (over 50 years of age), elderly and senile people (most patients are aged 70-85 years); incidence rates reach 15-25 cases per 100,000 persons over 50 years of age; women get sick more often than men (ratio from 2:1 to 3:1) [2, 5, 6]. The increasing likelihood of developing GCA with age is associated with a decrease in the activity of the immune system and remodeling of the blood vessel wall [5, 7].
Pathomorphology
GCA is classified as a granulomatous inflammatory process that occurs, in addition to GCA, in a number of other forms of vascular and visceral pathology [8]. Focal and segmental inflammatory damage to the arteries caused by GCA is most often transmural - in the form of panarteritis, which largely affects the medial layer of the arterial wall.
The morphological substrate “giant cell arteritis” that determines the name of the disease implies the presence of giant multinucleated cells in the inflammatory infiltrate of the affected vessel wall. However, in approximately ½ of cases, only mononuclear cells are detected in biopsies of the superficial temporal artery in patients with clinical manifestations of GCA. Multinucleated giant cells are also found in other forms of systemic vasculitis, so their presence cannot be considered a pathognomonic morphological sign of GCA [9].
In GCA, polymorphic cellular infiltration of the thickened vascular wall is observed - lymphoid cells, histiocytes (tissue macrophages), sometimes plasma cells and eosinophilic leukocytes. In some cases, the infiltrate contains giant multinucleated cells involved in the formation of granulomas. In areas where giant cells are localized, fragmentation and destruction of collagen and elastic fibers may be observed. However, the destruction of the vascular wall observed in necrotizing forms of systemic vasculitis is not typical for GCA.
Arteritis-induced concentric thickening of the vessel wall due to hyperplasia and fibrosis of the inner choroid leads to narrowing, deformation or closure of the vessel lumen [2, 5, 9]. Ischemic disorders arising under these conditions are, as a rule, not associated with mural thrombosis. The morphological manifestations of HCA in the form of pan- and post-starteritis are schematically presented in the figure.
Pathomorphological manifestations of GCA.
General clinical manifestations
Various variants of the manifestation and course of GCA are known. There are so-called classic, partial and erased variants of clinical manifestations. Moreover, as the disease progresses, a significant modification of the initial version of its course is possible. In the literature [10–12], one can also find indications of typical and atypical clinical manifestations of GCA. Among the atypical ones, of course, is focal granulomatous hepatitis [13]. However, the manifestations of GCA, especially those caused by damage to different vascular systems, should be characterized as heterogeneous or variable. Based on this, the detection of any “typical” and “atypical” manifestations of GCA can be considered just a “typical” feature of this disease.
The main symptom complexes of GCA are presented below (see figure).
The development of symptoms of damage to a specific vascular system usually occurs against the background of previously or simultaneously occurring general - constitutional symptoms. Relatively short-term or long-lasting constitutional symptoms mainly include increased body temperature, night sweats, general weakness, decreased appetite, and weight loss.
Clinical manifestations of arteritis of the branches of the external carotid artery, primarily the superficial temporal artery:
1. Headache, craniofacial (including temporomandibular) pain. 2. Palpable changes in the superficial temporal artery: wall thickening, pain, weakening or disappearance of pulsation. 3. Ischemic “intermittent claudication of the lower jaw” - pain in chewing movements that increases during chewing. 4. Intraoral ischemic disorders - orofacial pain, dysphagia, in rare cases, ulceration and partial necrosis of the tongue [11, 14].
Let's look at some of these manifestations in more detail.
Headache.
The first manifestation of GCA is usually pain in the temporal (frontotemporal, temporofacial), and less often in the occipital regions. Compared with ordinary cephalalgia, temporal and occipital pain in GCA is a local symptom corresponding to the localization of the affected vessel - the superficial temporal artery, in some cases - the occipital artery (another branch of the external carotid artery, not so often affected by GCA). Such pain in the temporal and occipital localization is distinguished by the following features: patients feel it as a new pain that has never occurred before; is limited, initially with one-sided localization; constancy and increasing intensity, which does not decrease with the use of conventional analgesics; characterized by the presence of areas of hyperalgesia, exposure to which (headgear, pillow) leads to increased or renewed pain; combined with generalized musculoskeletal pain (polymyalgia rheumatica), as well as constitutional symptoms.
Local palpation changes.
The development of headache in most cases is accompanied by areas of palpation pain in the temporal region and hardening of the branches of the superficial temporal artery accessible to palpation, as well as strengthening of their subcutaneous contours. One of the cardinal local signs of GCA is the weakening/disappearance of pulsation of the branches of the superficial temporal artery (when compared with palpable vessels on the intact side).
In the area of the affected superficial vessel, skin hyperemia may be observed, and in some cases, local trophic disorders and focal necrosis [15]. On the skin of the scalp along the branches of the superficial temporal artery, a kind of nodules can be detected - local painful compactions [2].
Ischemic "intermittent claudication of the lower jaw."
This manifestation is considered an important subjective one, somewhat specific to GCA. Essentially, this is an “intermittent claudication” of the masticatory muscles. This disorder is described by patients as transient difficulty or weakening of the movements of the lower jaw during prolonged chewing, especially of solid foods.
The presence of “intermittent claudication of the lower jaw” is a sign of insufficient blood supply to the masticatory muscles (supplied by the middle and deep temporal arteries, other branches of the external carotid artery). The development of “masticatory intermittent claudication” is thought to increase the likelihood of visual disturbances.
Polymyalgia rheumatica.
Almost 50% of patients with GCA are diagnosed with polymyalgia rheumatica syndrome - acute, bilateral aching pain and stiffness, covering proximal muscle groups - the neck, shoulder and pelvic girdle [2, 6, 16-18]. Compared with myofascial pain, polymyalgia rheumatica is accompanied by general signs of rheumatic disease and joint manifestations, including morning stiffness (magnetic resonance imaging and ultrasound examination of joints may also reveal periarticular and intra-articular changes [6]). In addition, polymyalgia rheumatica usually resolves under the influence of glucocorticoids.
The general clinical manifestations of GCA described above, obviously not associated with the development of critical ischemic disorders, belong to the first period of the classical variant of the disease. With the progression of GCA, the next stage is a period of stenotic/occlusive damage to the arteries of various vascular systems. For example, damage to the aorta is possible (with the development of dissection, aneurysm and rupture of the vascular wall [2, 19]), as well as its branches supplying blood to the upper and lower extremities.
Particular ophthalmic and neurological manifestations.
With GCA - vasculitis of large and medium-sized arteries of the craniofacial region, adjacent large and medium-sized precerebral and cerebral arteries of the carotid and vertebrobasilar systems may be involved.
Indeed, various forms of cerebrovascular disorders, including visual ones, are characteristic clinical manifestations of GCA. In contrast, vasculitic polyneuropathy caused by damage to the vasa nervorum
is not characteristic of GCA, nor is it characteristic of another large vessel vasculitis, Takayasu arteritis [20]. With GCA, local sensory neuropathic disorders may develop, usually in the area of focal skin necrosis; Such manifestations of sensory mononeuropathy should be considered as a consequence of arteritis of any superficial vessel supplying the skin and its innervation apparatus.
Clinical manifestations of vascular arteritis of the internal carotid and vertebral arteries.
These are visual and cerebrovascular disorders (actually visual and oculomotor) and stroke.
Visual impairment
in patients with GCA they can be visual [21–24] and oculomotor [25, 26]. In this case, oculomotor disorders may be limited to isolated pupillary symptoms in the form of persistent unilateral mydriasis with an absent reaction to light.
All forms of short-term and persistent visual disturbances arising from GCA are vascular intracranial, caused by focal ischemia/infarction in the blood supply area of the internal carotid and, in some cases, vertebral arteries. Primary vascular disorders that cause the development of visual disorders are most often represented by stenosis of the ophthalmic artery (a branch of the internal carotid artery) or the ciliary and other branches of the ophthalmic artery. The most characteristic of GCA is damage to the posterior ciliary branches of the ophthalmic artery, which supply blood to the distal part of the optic nerve [24].
The development of actual visual and oculomotor disturbances in GCA may be a harbinger or sign of vascular damage to the eyeball or brain. At the first stage, short-term visual disturbances usually occur in the form of decreased visual acuity and diplopia, which are essentially one of the forms of transient partial disturbance of intracranial circulation. Later (after several hours, days or weeks), persistent visual disturbances may develop, often combined with focal cerebral symptoms.
Topically, visual disturbances in GCA can be defined as extracerebral (damage to the oculomotor nerves, muscles and other structures of the eyeball) or cerebral (damage to the optic nerve - “brain appendage”, stem - oculomotor and cortical - visual structures). Our own version of the taxonomy of visual disorders in GCA is presented in Table. 1.
Table 1. Taxonomy of the main forms of visual disorders occurring in GCA
Information about recently occurring visual disturbances, including short-term ones (decreased visual acuity, double vision), in combination with acute/subacute headache are important diagnostic indications for GCA. In such cases, immediate administration of glucocorticoids in high doses helps prevent the development of persistent visual impairment. If persistent vision loss has already occurred, it is possible to obtain a therapeutic effect only in some cases with immediate initiation of treatment (no later than the first few hours after the development of symptoms). However, the use of glucocorticoids can probably prevent the development of visual impairment in a previously intact eye.
An irreversible decrease in visual acuity in patients with GCA is usually associated with the development of anterior ischemic optic neuropathy [24]. Moreover, anterior ischemic optic neuropathy largely confirms the diagnosis of GCA, and ischemic retinopathy confirms the presence of cerebrovascular pathology.
Stroke
- an infrequent and in many cases delayed neurological manifestation of GCA. Its frequency can be 3–7% of cases [12, 16, 27], while strokes in the vertebrobasilar system predominate, reaching 50–75% of cases [10]. Current data indicate the relative rarity of stroke caused by GCA. A significantly higher prevalence of cerebrovascular disorders in GCA is evidenced by transient ischemic cerebral and visual disorders, the frequency of which, according to our data, is many times higher in patients with GCA.
According to angiography and the results of morphological studies, the development of stroke in patients with GCA occurs against the background of multiple, including bilateral local narrowing of the arteries of the carotid and vertebrobasilar systems, including their extracranial sections. A significant frequency of stenotic lesions of the extracranial part of the vertebral artery (greater than those caused by atherosclerosis) may be associated with the structural features of the vertebral artery. A number of researchers in this matter share the concept of I. Wilkinson and R. Russel (1972), according to which the elastic fibers of the middle and outer choroid, the targets of the inflammatory process in GCA, are mainly represented in the vertebral artery before it enters the cranial cavity [10]. The selectivity of damage to the elastic fibers of the middle and outer choroid in GCA may also apply to other large arteries of the muscular elastic type [2, 28].
The occurrence of stroke in patients with GCA may be preceded by transient ischemic attacks, often in the form of short-term visual impairment. The development of focal neurological symptoms in GCA (as in other systemic rheumatic diseases, in particular systemic lupus erythematosus and antiphospholipid syndrome) may be associated with multifocal cerebral damage. However, in systemic lupus erythematosus and antiphospholipid syndrome, brain damage, even in cases of recurrent stroke, is often reversible [3, 4]. In GCA, single or multiple focal brain lesions can lead to the development of severe neurological disorders [10, 12, 27, 28]. Clinical features of stroke in GCA are summarized in Table. 2.
Table 2. Clinical characteristics of cerebrovascular manifestations of GCA
Diagnosis of GCA
When making a diagnosis of GCA, it is recommended to use the “classification criteria of the American College of Rheumatology” (1990) [29]. Five such criteria include 1) age at onset ≥50 years; 2) recent (“new”) headache; 3) changes in the superficial temporal arteries (pain on palpation or decreased pulsation not associated with atherosclerosis); 4) increase in ESR ≥50 mm/h; 5) biopsy data of the superficial temporal artery: vasculitis with a predominance of mononuclear cell infiltration or granulomatous inflammation with the presence of multinuclear giant cells.
The diagnosis of GCA is considered reliable if at least three of any signs are present. Despite the undoubted clinical significance of the five specified classification criteria, their practical application cannot be considered as a “key” to establishing the diagnosis of GCA [30], since criteria 1, 2 and 4 can be positive in many other individual or combined diseases.
In neurological practice, the formulation of the diagnosis of “stroke due to GCA” is carried out according to the rules for writing the final clinical diagnosis: GCA is indicated as the “main disease”, and the resulting stroke is a “complication of the main disease”.
Diagnostic actions of a neurologist for suspected GCA
1. Conducting local diagnostics: visual and palpation examination of the temporal areas; palpation and auscultation examination of brachiocephalic vessels.
2. Carrying out a routine diagnostic procedure - measuring blood pressure in both arms.
3. Purpose of a laboratory blood test: determination of ESR and C-reactive protein.
4. Purpose of ultrasound examination of the brachiocephalic arteries in order to identify occlusion/stenosis of the subclavian, common, internal and external carotid and vertebral arteries.
5. Purpose of computed tomography or magnetic resonance imaging of the brain: to exclude subarachnoid hemorrhage in the presence of intense, acute headache, especially combined with dizziness, nausea and photophobia, or meningeal symptoms; exclusion of stroke when focal neurological symptoms are detected.
6. Schedule an immediate consultation with a rheumatologist.
7. Appointment of a biopsy of the superficial temporal artery.
Carrying out local diagnostics for suspected GCA.
Concern for possible GCA should arise when examining any patient over 50 years of age experiencing subjectively “new,” acute/subacute craniofacial pain, predominant in the temporal region. The validity of the assumption of a diagnosis of GCA may be indicated by the results of local diagnostics aimed at identifying local signs of possible vasculitis (Tables 3 and 4).
Table 3. Local diagnosis for suspected GCA
Table 4. Anatomical landmarks for studying the superficial temporal and brachiocephalic arteries
Biopsy of the superficial temporal artery.
Biopsy of the superficial temporal artery is a method of intravital verification of the diagnosis of GCA. It is believed that its implementation should be carried out before the end of the first week of glucocorticoid use. However, morphological signs confirming the diagnosis of GCA can be detected within 2-6 weeks after the start of treatment [31].
This diagnostic procedure is a low-traumatic surgical intervention performed in a dressing room or operating room. Delay or refusal to perform a biopsy can only be associated with the lack of informed consent of the patient. When collecting material, it is necessary to excise at least 1-1.5 cm of the superficial temporal artery - directly at the site of its palpation and visual changes [10, 31, 32].
It is known that the results of a biopsy of the superficial temporal artery sometimes turn out to be negative, without revealing the morphological signs of GCA. This may be due to the intactness of the examined area (due to the focal and segmental nature of the vessel lesion) or the entire vessel (due to the selective nature of the vascular lesion). However, the absence of morphological confirmation of GCA does not entail the need to discontinue glucocorticoids in the presence of appropriate symptoms, as well as positive dynamics in response to their use.
Treatment of GCA
Establishing a diagnosis of GCA is an indication for the immediate administration of glucocorticoids (Table 5). Additionally, antiplatelet agents should be prescribed (in particular, acetylsalicylic acid in a low dose), possibly reducing the likelihood of stroke and blindness [6, 10, 16, 31].
Table 5. Features of the use of glucocorticoids in establishing the diagnosis of GCA
The effectiveness of the treatment is usually indicated by normalization of body temperature, a decrease in ESR and C-reactive protein, as well as regression of head, craniofacial, musculoskeletal pain and ischemic “intermittent claudication of the masticatory muscles.” However, previously occurring vision loss, as well as stenotic changes in the precerebral and cerebral vessels, persist in most cases.
At the same time, without excluding GCA as a possible, but rather rare cause of headache, there are not always enough reasons for the immediate prescription of glucocorticoids. For example, during the initial neurological examination of an elderly patient with recent onset of pain in the frontotemporal region, the absence of meningeal and acute focal neurological symptoms, an acceptable blood pressure level and unknown laboratory parameters.
In such cases, the neurologist’s recommendations may be limited to indicating the diagnostic measures listed above, as well as prescribing antiplatelet agents and vasoactive agents. During the mandatory re-examination, the need or otherwise for the use of glucocorticoids will likely become more apparent.
Forecast
With timely treatment, the course of GCA may be limited to a single period of exacerbation. However, the question of “cure” of the disease (as with other forms of systemic vasculitis) remains open in each case.
As a result of treatment based on the use of glucocorticoids, partial or complete regression of clinical and laboratory signs of the disease can be achieved. At the same time, even with continued use of glucocorticoids in maintenance doses, the possibility of developing another exacerbation of GCA cannot be excluded. Along with this, previously unobserved manifestations of the disease may occur, in particular acute ischemic cerebral disorders caused by stenosis of individual precerebral and cerebral arteries - the morphological outcome of GCA.
The author expresses gratitude to N.V. Bunchuk, L.P. Ananyeva and V.M. Tyurnikov for assistance in conducting this study.
How is Horton's disease treated?
If a patient is diagnosed with temporal arteritis, treatment should begin immediately. As a rule, it is prescribed and performed by a rheumatologist. The goal of therapy is to stop the incorrect functioning of the immune system, which causes vascular damage. For this purpose, glucocorticosteroid drugs are prescribed. At the initial stage, the patient is prescribed hormones in a dose that is comparable to the level of vascular damage and complications from the visual apparatus. If during the diagnostic process a sharp, acute drop in vision is detected, then so-called pulse therapy can be prescribed - short-term administration of ultra-high doses of corticosteroids to the patient. A month or later from the start of treatment (at the discretion of the doctor), the dose is gradually reduced to maintenance. Typically, the duration of therapy for giant cell arteritis is two years. The doctor may cancel treatment if there are no signs of illness within six months of maintenance therapy.
If treatment with corticosteroid hormones does not bring the expected results or the patient experiences serious side effects, the doctor may alternatively prescribe cytostatic drugs that block or slow down cell growth. Symptoms of the disease are treated with anti-inflammatory, vasodilating medications and anticoagulants.
Temporal arteritis affects mainly older people who suffer, among other things, from other chronic diseases when there are age-related metabolic disorders. To ensure that the therapy does not harm the condition of other organs and systems, during the treatment process the doctor monitors the liver function and the level of the patient’s mineral metabolism in order to notice signs of osteoporosis or liver failure in time. Also, in parallel with treatment, prevention of duodenal and gastric ulcers is carried out, and blood sugar levels are monitored. If the patient develops acute thrombosis in the affected area, the specialist may prescribe surgery.
You need to understand that it is currently impossible to completely cure an autoimmune disease. However, timely initiation and properly selected therapy blocks or significantly slows down the inflammation process, helping to prevent dangerous complications in the form of strokes, heart attacks, and complete loss of vision.
The prognosis for improvement in vascular condition and preservation of visual function is favorable if therapy is started at an early stage. Therefore, you should not put yourself at risk and delay a visit to the doctor if you often have a headache in the temporal region, double vision, or other signs of Horton’s disease.
Causes
The main cause of the development of temporal angiitis is considered to be an autoimmune reaction, in which specific complexes are produced that destroy healthy cells. Antibodies to immunoglobulins M and A are found in the blood of most patients. Immune complexes are deposited in the elastic layer of the arterial wall, causing persistent inflammatory processes. Other causes of the disease include:
- viral infections (hepatitis, herpes, influenza);
- genetic predisposition;
- chronic autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis);
- taking certain medications (vascular damage can be promoted by treatment with antibiotics, chemotherapy drugs, immunostimulants);
- age-related changes in the body;
- penetration of toxic chemicals into the blood;
- exposure to ionizing radiation.
Prevention
Due to the fact that the causes of the disease are not fully understood, doctors cannot give practical, effective measures for prevention. Despite this, there is a clear connection with the transmission of infectious diseases, so a person should carefully monitor the state of his immune system.
- Normalize your daily routine, go to bed on time, take breaks during heavy and active exercise.
- Watch your diet, do not eat junk food, drink enough water per day.
- Take vitamins, eat fruits and foods that are healthy for the body.
- If you have the slightest signs or suspicion of temporal arteritis, consult a doctor immediately.
- Complete abandonment of bad habits that affect the functioning and tone of blood vessels.
- Practice moderate physical activity in the form of gymnastics or other simple exercises.
- It's great if you toughen up in the morning. A morning contrast shower has a positive effect not only on your health, but also on your mood.
- Ventilate the room before going to bed.
Treatment
Unlike some other autoimmune diseases, Horton's disease responds well to therapy.
Rheumatologists treat the pathology. Therapy involves the use of conservative and surgical techniques.
Therapeutic treatment
Drug therapy is carried out in the absence of dangerous complications. The treatment regimen includes the following drugs:
- Glucocorticoids (Prednisolone). In the early stages of treatment, large doses of drugs are used. After stabilizing the patient's condition, the amount of administered medication is reduced to the minimum effective. The use of high doses of Prednisolone takes at least a year. Maintenance treatment is carried out for 12-24 months. Hormone therapy is accompanied by regular blood tests. The effectiveness of treatment is indicated by normalization of ESR and hemoglobin levels.
- Immunosuppressants (Azathioprine, Methotrexate). The drugs are used for severe vasculitis or glucocorticoid intolerance. They suppress the production of antibodies, reducing the intensity of autoimmune damage.
- Pulse therapy with Prednisolone. If there is a threat of vision loss, the drug is administered intravenously for 3 days. In the following weeks the patient takes tablets.
- Vasodilators (Papaverine). The drugs eliminate the spasm caused by inflammation, restoring blood flow.
- Anticoagulants. Heparin injections are used to prevent blood clots. Normalization of the rheological properties of blood plays an important role in recovery.
Important information: How is blood erythremia and symptoms of Vaquez disease treated?
Surgical method
Surgical interventions are performed when complications develop in the form of blockage of a vessel or the formation of an aneurysm.
In case of acute obstruction of the temporal artery, the affected area is replaced with a prosthesis. If angioprosthetics is not possible, workarounds are created to help restore blood flow.
Folk remedies
Folk remedies cannot be used as an independent means of treatment. Refusal to use medications leads to rapid deterioration of the condition. Acute manifestations are treated in a hospital; during the recovery period the following remedies can be used:
- Calendula infusion. The plant contains substances that have anti-inflammatory and healing properties. To prepare the infusion 2 tbsp. l. flowers are poured with 0.5 liters of boiling water and left for 3 hours. The strained liquid is taken 100 ml 3 times a day.
- Licorice root infusion. 2 tsp. crushed raw materials are brewed in a glass of boiling water. After 2 hours, filter the infusion. This remedy is drunk throughout the day, divided into 3-4 doses.
- Chamomile tea. 1 tbsp. l. flowers are poured with 200 ml of hot water and kept for 30 minutes. Drink 200 ml of tea 3-4 times a day.
- Echinacea infusion. 1 tbsp. l. herbs are poured into 500 ml of boiling water and left in a thermos for 3 hours. Drink a glass of infusion in the morning and evening.