Chronic occlusions of the coronary arteries
Chronic occlusions make up a significant portion of coronary artery lesions detected in patients during diagnostic coronary angiography. In the case of multivessel disease, the patient may be offered either coronary artery bypass surgery or an endovascular coronary artery stenting procedure.
If multi-vessel lesions of the coronary arteries are detected, it is possible to perform a one-stage endovascular procedure for myocardial revascularization on several coronary vessels or to perform a staged endovascular procedure. Recanalization of chronic occlusions, in turn, requires special training of the radiosurgeon and sufficient experience in performing such operations.
An example of successful treatment of a patient with multivessel disease and chronic coronary occlusions
Patient A., 44 years old, was admitted to the Clinic of Innovative Surgery in September 2015. For a long time, the young man was bothered by chest pain and shortness of breath with little physical activity, and a sharp impairment in his ability to work. After a detailed examination, a diagnosis was made - coronary heart disease, functional class 3. Coronary angiography was recommended and performed.
Coronary angiography revealed multi-vessel multi-level occlusive-stenotic lesion of the coronary bed:
- LKA barrel: normally positioned, not changed,
- RCA: in the proximal segment there is extensive chronic occlusion, the post-occlusion section is satisfactorily filled through intra- and intersystem collaterals.
- 1DV: large branch, in the proximal third from the mouth there is stenosis up to 80%.
- Intermediary artery: large branch, 80% stenosis in the proximal third.
- OA: in the middle segment there is chronic occlusion, the post-occlusion section is satisfactorily filled through intra- and intersystem collaterals.
- RCA: the previously installed stent in the middle segment is passable, without signs of restenosis.
Taking into account the data from the clinical picture, laboratory and instrumental research methods, and coronary angiography, a collective decision was made on the need for surgery to restore the patency of the arteries. Considering all the risks and possible complications, the patient categorically refused coronary bypass surgery and insisted on having coronary stenting. The department's doctors were ready to help him.
Operation stages
After careful medical preparation, the patient underwent recanalization and stenting of the circumflex branch of the left coronary artery, as well as recanalization of the anterior descending branch of the left coronary artery, followed by bifurcation stenting of the LAD and diagonal branch of the LMCA. The complex operation lasted several hours. However. For the patient, it was painless - the intervention was performed under local anesthesia with novocaine at the puncture area in the femoral artery. During the procedure, the anesthesiologist and surgeons were able to communicate with the patient, he was conscious.
The result of the long and painstaking work of the clinic’s team of doctors was the complete restoration of the patency of all arteries of the heart and, as a result, a significant improvement in the patient’s quality of life.
Subclavian artery occlusion
The main causes of occlusion of the subclavian artery are obliterating atherosclerosis, obliterating endarteritis, Takayasu's disease (nonspecific aortoarteritis), post-embolic and post-traumatic obliterations.
Atherosclerosis is the most common cause of occlusive lesions of the aorta and its branches. At the same time, atherosclerotic plaques protruding into the lumen of the vessel are formed in the intima of the arteries. As a result of subsequent sclerosis and calcification of the vascular wall in the area of the affected area, deformation and stenosis of the lumen of the vessel gradually progress, which determine the ischemic stage of atherosclerosis. In some cases, atherosclerotic lesions may be complicated by thrombosis, leading to acute ischemia and necrosis of the blood supplying organ (thrombo-necrotic stage of atherosclerosis). Additional risk factors for atherosclerosis are:
- smoking;
- arterial hypertension;
- hypercholesterolemia;
- diabetes;
- cardiovascular diseases.
Obliterating endarteritis, as the cause of occlusion of the subclavian artery, is characterized by inflammatory changes in the walls of the arteries, pronounced hyperplastic processes leading to thrombosis and obliteration of blood vessels.
Takayasu's disease, named after the Japanese ophthalmologist who first described it, can occur with damage to the branches of the aortic arch, the development of aortic aneurysms, coarctation syndrome, aortic insufficiency, vasorenal hypertension, abdominal ischemia, pulmonary artery damage, and a general inflammatory reaction. Nonspecific aortoarteritis most often leads to occlusion of the distal (second-third) segments of the subclavian arteries.
The development of occlusion of the subclavian artery can be facilitated by extravasal compression factors: scars and tumors of the mediastinum, curvature of the cervicothoracic spine, cervical osteochondrosis, neck injuries, fractures of the clavicle and first rib with the formation of excess callus, and chest injuries. In some cases, occlusion of the subclavian artery is a consequence of congenital anomalies of the aortic arch and its branches.
In the pathogenesis of disorders arising from occlusion of the subclavian artery, the main role is played by ischemia of the tissues supplied by the affected branch. Thus, when the proximal segment of the subclavian artery is occluded, blood enters its distal segment and upper limb through the vertebral artery, which leads to depletion of the blood supply to the brain. This phenomenon, especially manifested during physical activity, is called steel syndrome or “subclavian steal syndrome.”
The rapid development of occlusion of the subclavian artery, associated with associated thrombosis, leads to cerebral ischemia - acute ischemic stroke.
Treatment methods for femoral artery occlusion
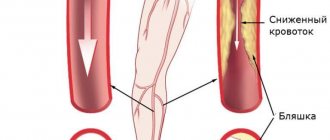
With limited occlusion, the body can compensate for the blood circulation of the limb using blood flow through the lateral branches of the arterial system (collateral circulation). In this case, conservative treatment is possible.
With increasing severity of ischemic symptoms, intermittent claudication occurring after less than 100 meters of walking, pain at rest, it is necessary to resort to surgical treatment. Such symptoms mean that circulatory compensation is insufficient, and this threatens the development of ulcerative-necrotic changes, gangrene and loss of limb.
Surgery
In the surgical treatment of occlusion, depending on the area of artery damage, the following are used:
- endarterectomy (removal of atherosclerotic deposits from the lumen of the artery);
- femoropopliteal bypass surgery;
- femoral-tibial bypass (if there is concomitant occlusion of the popliteal artery).
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Surgical interventions for vasoconstriction. Coronary angioplasty
Today, there are several non-invasive techniques that are effectively used to narrow blood vessels.
The most popular methods in modern endovascular (vascular) surgery include angioplasty and stenting.
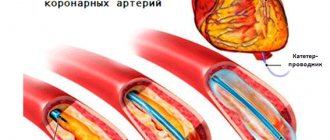
Minimally invasive vascular surgery is performed through a small puncture or incision in the patient's skin. The surgeon first inserts a needle with a special core - a stylet - into the hole made, and then a catheter - a thin hollow tube. The progress of the procedure is monitored using an X-ray monitor. Moving the catheter up the bed of the vessel, it is brought to the site of narrowing of the artery, localized in advance by angiography. Depending on the specific procedure, a stent or balloon is attached to the end of the catheter.
The lumen of a healthy artery is uniformly wide and the walls are smooth. Age and atherosclerosis provoke the appearance of deposits on the walls of blood vessels, consisting of fibrous tissue, calcium and cholesterol. These are so-called atherosclerotic plaques. The more such plaques on the walls of the arteries, the more the lumen of the vessel narrows and the blood flow worsens. Eventually the narrowing reaches a critical degree and normal blood flow becomes impossible. Ischemia (insufficient blood supply) develops and, as a result, pain and even necrosis (death) of tissue.
Angioplasty (balloon) is most often used to treat diseases of peripheral vessels, and sometimes to restore the functional patency of veins. In addition, it is the only medical alternative to coronary artery bypass surgery, in particular because it does not require an incision for manipulation, is performed under local anesthesia, and the recovery period after surgery is quite short.
Stenting is used when it is necessary not only to expand the lumen of a vessel, but also to reinforce it by placing a stent - a miniature wire frame.
Indications for surgery
Traditionally, vascular surgery is indicated for all patients with moderate to severe vasoconstriction.
A significant blockage of the vessel (the tip of the catheter does not pass through the narrowing site) may be a contraindication.
Complications that occur after stenting
The possibility of complications after stenting cannot be excluded:
- bleeding at the catheter insertion point;
- formation of a channel between a vein and an artery;
- high risk of blood clots forming around the stent (in the first months after surgery);
- the occurrence of restenosis;
- blockage of the lumen of the artery below the site of narrowing;
- blood clot formation in an artery;
- renal failure;
- weakening or rupture of the vessel wall;
- allergy to contrast;
- arterial wall dissection
Coronary angioplasty surgery
Preoperative preparation for coronary angioplasty (transluminal reconstruction) consists of a complete examination of the patient, during which the following must be carried out:
- X-ray examination of the chest;
- electrocardiogram;
- laboratory tests of urine and blood;
- X-ray contrast tolerance test (if an angiographic examination of the heart vessels is prescribed before surgery)
Before surgery, it is recommended to abstain from eating. Regarding taking medications (especially antidiabetic drugs), you should consult a cardiologist.
Specifics of the procedure
A catheter is inserted through the patient's femoral artery and passed to the narrowed section of the artery for intraoperative coronary angiography, during which the location and stage of narrowing of the arterial lumen is identified.
Based on the data obtained, the cardiac surgeon selects a balloon of the appropriate size and a suitable guide catheter. In order to prevent blood clots and further thin the blood, the patient is prescribed heparin.
A guide catheter is a thin wire with a radiopaque tip that is inserted into the patient's diseased coronary artery. Having received a complete picture, the cardiac surgeon directs the guidewire to the right place.
The tip is brought out beyond the narrowing of the artery lumen.
After this, a balloon catheter is inserted through the guidewire, which delivers the balloon to the site of narrowing. Once inflated, the balloon expands the lumen of the artery, flattening the plaque. If the purpose of the operation is to place a stent, then when the balloon is inflated, it is pressed into the wall of the vessel, reinforcing the affected area and preventing it from narrowing.
Effect and rehabilitation
As a rule, as a result of a successful coronary angioplasty operation, blood flow in the coronary vessels is significantly improved and the likelihood of coronary artery bypass grafting is significantly reduced.
To minimize the manifestations of the underlying disease, you should adhere to the diet prescribed by your doctor, refrain from smoking and eliminate stressful moments.
Within six hours after a successful operation, the patient is allowed to get up and walk, but he spends the first two days in the inpatient department of the cardiac center.
The rehabilitation period lasts on average a week.