Many people wonder what diseases are possible if the hematocrit is below normal, what does this mean, which doctor should they contact to restore normal values? All this must be taken into account, because correct diagnosis and an appropriate treatment regimen help a person quickly return to a full life.
Main signs of low hematocrit
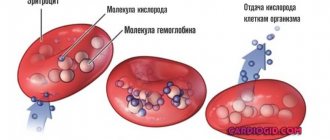
Hematocrit
(the total number of red blood cells contained in the blood) is determined as a percentage and allows the doctor to assess the quality of oxygen supply to tissues.
To determine the hematocrit level, you need to know the standard indicators, while the norm will be different for a child and an adult:
- in newborns - 34-64%
; - up to one year - 34-43%
; - 1-5 years — 33-40%
; - 6-12 years - 34-43%
; - 12-17 years old - 34-45%
; - in women - 30-46%
(indicators decrease during pregnancy due to an increase in total blood volume); - for men - 40-52%
.
Let's list what symptoms indicate decreased performance:
- general malaise and fatigue;
- cardiopalmus;
- deterioration of hair condition;
- frequent migraines;
- paleness of the skin;
- causeless shortness of breath.
All these symptoms may indicate a decrease in hematocrit in the blood: the body ceases to receive the required amount of oxygen. To confirm low levels, you should undergo a complete blood test (indicated in the results by the symbols HCT). Hematocrit is determined using a graduated glass tube, which is filled with blood and centrifuged (as a result, it becomes clear which part of the tube is occupied by blood cells). In addition, special automatic analyzers are increasingly used.
High levels of cholesterol in the blood negatively affect the condition of all human organs, especially the heart and brain. To reduce cholesterol, you can take special medications that reduce this indicator. Read more in the article: “cholesterol pills.”
Indications and preparation for analysis
The hematocrit indicator is always indicated in the results of a general blood test. This means that it can be assessed:
- During any medical examination or mandatory medical examination.
- In preparation for surgery.
- During hospitalization and before discharge.
But besides this, there are certain indications when it is necessary to determine the hematocrit. In this case, a direct measurement is performed: the plasma is separated by centrifuging the material and an accurate indicator is obtained. Indications for this:
- Bleeding.
- Blood clotting problems
- Dehydration of the body.
- Anemia.
- Polycythemia.
In order to get a reliable result, you should refuse food 6-10 hours before taking blood from a vein or from a finger. As a rule, the analysis is taken in the morning. It is also necessary to avoid drinking alcohol 2-3 days and refrain from smoking 2-3 hours before the procedure.
Factors contributing to a decrease in hematocrit
Doctors today identify several reasons why the hematocrit is low:
- poor nutrition;
- kidney pathology;
- diseases that force a person to remain in a lying position for a long time;
- systematic fasting (exhaustive diets, etc.);
- chronic form of inflammatory diseases;
- pregnancy;
- diseases of the cardiovascular system;
- oncological diseases;
- significant loss or increase in blood volume;
- blood thinning;
- disturbances in the formation of red blood cells;
- liver pathology.
A sharp drop in hematocrit levels may indicate anemia, a disease that affects life expectancy.
A low hematocrit indicates serious disorders in the body, therefore, after a blood test, a full examination is required to help find the cause and choose the best treatment.
Lactose intolerance worries a huge number of people. What products contain it, who is most predisposed to the disease, and what symptoms of lactose intolerance occur in adults. Read more in the article: “lactose intolerance.”
Norm
The hematocrit norm differs depending on age and gender. In newborns, the rate is considered high and the norm is 42% - 65%. As one grows older, it decreases; in older people, a minimum level of hematocrit is observed. For adults aged 18-65 years, the norm is:
- For men - 41% - 53%.
- For women - 36% - 46%.
Deviations from the norm can be observed during pregnancy. From about 20 weeks, the indicator decreases due to an increase in the amount of liquid part of the blood for physiological reasons. After childbirth, the hematocrit quickly returns to normal values in the absence of pathologies.
Deviations towards increasing hematocrit are recorded:
- In smokers, due to oxygen starvation of tissues, which leads to an increase in the production of red blood cells.
- When rising to a high altitude, the production of red blood cells increases due to the body's adaptation to the reduced oxygen concentration in the air.
- For stress and traumatic shock, which is characterized by intense pain.
- When taking corticosteroid drugs and diuretics,
Deviations towards a decrease in hematocrit are recorded:
- With prolonged immobility.
- When taking antiplatelet agents and anticoagulants that thin the blood.
- Against the background of high fluid consumption.
- For chronic alcoholism.
Danger during pregnancy
During pregnancy, NCT levels should be constantly monitored: to avoid the development of anemia, doctors prescribe systematic testing. In this case, there are several reasons for low HCT levels:
Advertising:
- pregnancy a short time after a previous birth;
- early age of the expectant mother;
- pregnancy with multiple fetuses;
- severe toxicosis;
- insufficient consumption of foods containing iron;
- anemia was diagnosed before pregnancy.
If left untreated, the following consequences are possible:
- premature birth;
- postpartum depression;
- underweight baby;
- anemia of the newborn;
- blood loss during childbirth;
- the birth of a baby with behavioral problems;
- delayed physical development of the child.
Reasons for decline in women
{banner_banstat10}
In the fairer sex, the development of a pathological process is possible as a result of exposure to natural factors.
Pregnancy
As practice shows, a decrease in hematocrit is a completely normal phenomenon in the second and third trimesters of gestation.
Natural processes occur, which, in fact, act as a kind of catalyst for a drop in the number of red blood cells.
No action needs to be taken. Provided that the woman does not have the diseases described above.
Menstrual cycle
Approximately in the middle of the cycle, hematocrit values begin to fluctuate downward. This is also normal.
No special treatment is needed. Everything will return to normal after the cycle is completed.
Menopausal process
The reason for a decrease in hematocrit in a woman after 45-50 years is the attenuation of reproductive function with a gradual drop in hormone concentrations.
Occurs in all women and is called menopause. There is no reason to worry, this is also a temporary phenomenon.
Methods for treating low hematocrit
Advertising:
If the hematocrit is below normal, this means that the patient needs to reconsider his diet and replenish the lack of iron in the body. In addition, you need to increase your intake of vitamin C, which helps to better absorb iron.
Useful products are listed in the table.
| Iron-rich foods | Vegetables and fruits containing vitamin C |
| Greenery | Tomatoes |
| Beef liver | Strawberry |
| Fish | Oranges |
| Legumes | Limes |
| Red fish meat | Tangerines |
| Eggs | Bergamot |
| Dried fruits | Lemons |
| Chicken | Grapefruits |
If consumption of such food is impossible due to allergic reactions, then the patient is given special supplements containing iron. An iron course can be recommended in the form of injections or in tablet form. If the main reason for the indicators is below normal is medications, then they are canceled, and the doctor selects others that do not affect the hematocrit. Iron deficiency can also be replenished with vitamin complexes that are specially designed to increase iron levels and contain all the necessary components for better absorption.
One of the most serious causes of a hematocrit below normal is sickle cell disease. Red blood cells are disc-shaped flexible cells. In the case of sickle cell anemia, they become more rigid and sickle-shaped (contain defective hemoglobin). Such red blood cells cannot move freely and can block blood vessels, leading to damage to organs and tissues. In this case, a special treatment regimen is required, as well as consultation with several specialists: a hematologist, cardiologist, therapist and neurologist.
Preparation
Donating blood for a general analysis does not require special preparation, but to identify an adequate clinical picture of the formed elements and hematocrit, it is recommended to adhere to the following rules:
- Blood donation is performed on an empty stomach;
- stopping smoking in the morning on the day of the test (blood is donated in the morning);
- refusal of physical activity the day before and on the day of delivery of the biomaterial;
- prohibition of taking anticoagulants, antiplatelet agents and other drugs that affect the blood coagulation system 3 days before the study;
- abstaining (if possible) from stress and emotional experiences on the eve of the study;
- refusal to carry out diagnostic procedures (x-ray, ultrasound and other studies) the day before donating blood.
Sources:
- A.A. Kishkun, Doctor of Medical Sciences, Prof. Guide to laboratory diagnostic methods, - GEOTAR-Media, 2007.
- Mandy Flannery O'Leary, MD, MPH, FCAP. Hematocrit. — Laboratory Medicine, Medscape, 2014.
- Andrew S Artz, MD, MS. Anemia in Elderly Persons. - Hematology, Medscape, 2015.
Treatment of crises and complications
The main goal of treatment is to prevent crises and reduce the risk of complications, such as kidney and liver pathologies, stroke, heart attack, visual impairment and prolonged depression. Doctors, as a rule, recommend the drug Hydroxycarbamide for any type of disease: it reduces the risk of developing anemia and speeds up recovery.
Advertising:
The patient’s well-being is also positively affected by:
- minimizing stress and overexertion;
- moderate exercise;
- proper consumption of drinking water.
Quite often, cases of false hematocrit are observed, for example, due to incorrect general analysis, long clamping of the vein with a tourniquet, taking the analysis in an inappropriate position, etc.
Critical hematocrit values require immediate blood transfusion to save the patient’s life.
Reasons for increasing hematocrit
Dehydration (dehydration). Loss of fluid due to repeated vomiting and/or diarrhea, sunstroke, burn disease, pathology of the digestive tract, intestinal obstruction, hyperhidrosis (excessive sweating), peritonitis leads to blood thickening due to an unchanged number of red blood cells.
Hypoxia. People suffering from diabetes, smokers, people located high in the mountains or in unventilated areas experience a lack of oxygen, which leads to the release of red blood cells into the bloodstream.
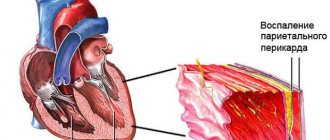
Cardiovascular pathology. Heart defects, coronary disease, and cardiovascular failure are accompanied by a lack of oxygen in the blood.
Bronchopulmonary pathology. Chronic hypoxia leads to: bronchial asthma, emphysema, obstructive bronchitis and other pulmonary diseases.
Neoplasms in the kidneys. Any kidney tumor provokes increased production of erythropoietin, which increases the formation of red blood cells.
Erythrocytosis. The pathology is characterized by increased production of red cells (true erythrocytosis) or redistribution of formed blood elements in some diseases (redistribution).
Erythremia. Refers to true erythrocytosis, synonymous with Vaquez-Osler disease. It is one of the variants of chronic leukemia.
Leukemia. Accompanied by an increase in white blood cells and a decrease in its liquid part.
Thrombocytopenia
HIV
Hepatitis
Iron deficiency
14803 12 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Thrombocytopenia: causes of occurrence, in what diseases it occurs, diagnosis and treatment methods.
Definition
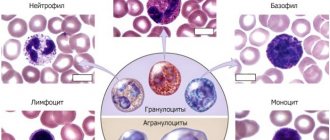
Platelets are plate-shaped blood cells that participate in blood clotting processes. Their main function is to close a wound when bleeding by forming a thrombus, or blood clot. Thrombosis is a natural process of protection against massive blood loss in any injury. A deficiency of platelets in the blood is called thrombocytopenia. This condition is often asymptomatic, but can be life-threatening if the number of blood platelets decreases significantly.
In addition to stopping bleeding (hemostasis), platelets perform a number of important functions in the human body: releasing substances that constrict blood vessels during bleeding; stimulation of tissue repair in case of any injury; regulation of local inflammation and immunity processes.
These functions are activated when there is any damage to the endothelium (the inner layer covering the walls of blood vessels). A lack of platelets leads to a disruption of the blood coagulation system and, as a result, increased bleeding, hematomas (bruises) and a dark red rash on the skin and mucous membranes (this rash does not disappear with pressure).
Prolonged bleeding of the gums, large amounts of bleeding from small wounds and during menstruation are an alarming signal indicating a possible problem with the blood coagulation system.
Types of thrombocytopenia
Thrombocytopenia is understood as a decrease in the number of platelets in the peripheral blood below 150 thousand/μl. Among all thrombocytopenias, the following conditions are distinguished:
- Dilution thrombocytopenia - occurs with massive bleeding and replenishment of the circulating blood volume with solutions.
- Thrombocytopenia of distribution - often occurs with excessive pathological utilization of platelets in an enlarged spleen.
- Productive thrombocytopenia occurs when bone marrow function is impaired as a result of various diseases or radiation therapy.
- Thrombocytopenia of consumption - occurs with DIC syndrome (disseminated intravascular coagulation - a pathological condition when blood clots form in the bloodstream of many organs) or with constant autoimmune damage to the vascular endothelium. There is a pathological activation of platelets and their rapid consumption (consumption) by the body.
- Pseudothrombocytopenia occurs when the analysis technique is violated with the development of platelet aggregation.
Possible causes of thrombocytopenia
One of the common causes of thrombocytopenia is excessive platelet consumption
in the body, for example, with DIC syndrome.
Immune form of thrombocytopenia
is considered the most common immune blood pathology. It develops quickly, with a rise in body temperature and the appearance of a profuse rash on the skin of the lower extremities, buttocks, around large joints, sometimes reaching the face. The rash consists of small hemorrhages in the skin, often accompanied by joint pain, swelling, and loss of movement in the affected joints. Sometimes it manifests itself as cramping abdominal pain, nausea, vomiting and loose stools. Cases of blood appearing in the urine have been described.
Autoimmune thrombocytopenia
(idiopathic thrombocytopenic purpura, Werlhof's disease) is caused by a decrease in platelet lifespan due to the effects of antiplatelet autoantibodies. Such thrombocytopenia can occur in waves, with alternating periods of exacerbation and remission. Often the disease makes itself felt against the background of infectious diseases: influenza, human immunodeficiency virus (HIV), Epstein-Barr virus (EBV), parvovirus B19, cytomegalovirus infection (CMV), viral hepatitis B and C.
Among productive thrombocytopenias
Aplastic anemia, tumor processes in the bone marrow, and radiation injuries occupy a special place.
All of these conditions are characterized by a sharp decrease in the hematopoietic (hematopoietic) function of the bone marrow due to certain structural changes.
Aplastic anemia
is characterized by a decrease in the production of all three hematopoietic lineages: red blood cells, leukocytes and platelets. Each germ is responsible for specific functions in the body, and a decrease in the cells produced leads to the appearance of corresponding symptoms. A decrease in platelets leads to increased bleeding, a decrease in the number of red blood cells indicates signs of anemia (pallor, fatigue, brittle hair, chest pain), and a decrease in leukocytes leads to infectious complications in the form of recurrent sore throats, pneumonia, etc. In some cases, the bone marrow is replaced by fatty tissue tissue, which also disrupts the formation of blood cells.
For B12 and folate deficiency anemia
the maturation of future platelets is disrupted; they die even before the maturation stage. The disease is manifested by pale skin, rapid heartbeat, and shortness of breath. With a severe deficiency of vitamin B12, sensory disturbances, paresis and paralysis are possible.
Different types of leukemia
lead to the appearance of tumor cells, which divide at tremendous speed and soon replace the bone marrow. In this case, the function of all three hematopoietic germs is disrupted. Immature cells appear in the bone marrow and blood, unable to perform their function.
Drug-induced thrombocytopenia
may develop as a result of taking certain medications, for example, cytostatics, which inhibit platelet formation in the bone marrow.
Diseases accompanied by an increase in the size of the spleen
(splenomegaly) can lead to increased destruction of platelets, or hypersplenism (increased platelet utilization by the spleen). In addition to platelets, red blood cells are also destroyed, which leads to the development of not only a thrombocytopenic state, but also to hemolytic anemia.
Such diseases include liver cirrhosis, including alcohol etiology, chronic heart failure, and lymphoproliferative diseases.
Which doctors should you contact if you have thrombocytopenia
? The diagnosis of thrombocytopenia is established using laboratory tests. Most often, patients who subsequently develop thrombocytopenia come to us with complaints of increased bleeding, rash, malaise, and fatigue. If a decrease in platelet count is detected, the therapist will prescribe a consultation with a hematologist. In some cases, consultation with a hepatologist or rheumatologist is required.
Diagnosis and examinations for thrombocytopenia
If signs of thrombocytopenia are detected, the doctor will prescribe a set of laboratory and instrumental research methods:
- clinical blood test: general analysis with platelet count, leukoformula, ESR (with blood smear microscopy in the presence of pathological changes);
Blood test for hematocrit
The manipulation is performed in the morning, blood is taken from a vein or from a finger. At the Medart clinic, the most modern equipment is used for analysis, so the sampling is most often done from a vein.
To obtain the material, special vacuum containers (vacutainers) are used. This is a modern syringe replacement that provides a number of benefits for the patient:
- Virtually painless procedure.
- Minimum time to obtain the required amount of blood.
- Accurate calculation of the amount of reagent and blood.
- Minimum time for conducting the study and issuing results to the patient.
Modern technologies allow the procedure to be carried out as quickly as possible, without consequences for health.