Immature granulocytes are a type of leukocyte - white blood cells that differ in appearance and function in the body. This group includes promyelocytes, myelocytes and metamyelocytes. They got their name because granules are visible when microscopically stained.
Normally, immature granulocytes should be present in the bone marrow and not in the peripheral blood. They can be elevated in an adult, both as a result of physiological reasons and in certain diseases. The analysis is often prescribed for the diagnosis of infectious and tumor processes.
What does a granulocyte test show?
Immature granulocytes are elevated in adults - a marker of a pathological left shift in the leukocyte blood count. Mature cells are the basis of “white blood” or leukocytes, the main function of which is the body’s immune defense. Granulocytes make up up to 80% of the total number of leukocytes.
Immature cells of this type are produced in the bone marrow and appear in the blood in two cases - with a deficiency of mature granulocytes and to replace old forms (normal levels in the blood).
Their circulation in plasma is short - about 6-7 days, and their lifetime in tissues is on average 2 days. Since the biological cycle of cells is very short, their number in the blood should normally be minimal.
A disruption of the circulation mechanism of immature granulocytes indicates a deterioration in the body’s “line of defense”, a decrease in its resistance to infectious and other diseases, since the cells that subsequently form are responsible for the production of antimicrobial, antiparasitic and anti-inflammatory substances.
When the pathological process is activated, granulocytes begin to die faster and there are not enough of them. To replenish the supply, immature forms of cells enter the bloodstream, designed to fill the “gap” in the immune defense.
Immature granulocytes are reduced
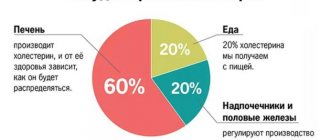
As already mentioned, the norm is when there are no immature granulocytes in the human blood (with the exception of newborns and pregnant women).
How can we talk about their reduced levels in the blood in this case? In this case, we are talking about a decrease in the production of neutrophils, eosinophils and basophils by the bone marrow. When foreign agents (toxins, pathogenic agents) enter the body, mature leukocytes begin to destroy them, dying themselves. However, the bone marrow cannot supply the required number of new cells, including immature ones, to replace the failed white blood cells.
The low content of granular leukocytes, both mature and immature, is caused by many reasons. Moreover, neutrophils have their own reasons, and eosinophils and basophils have their own.
- Neutrophil deficiency is most often observed with:
- neoplasms in the bone marrow (myelofibrosis, leukemia),
- radiation sickness,
- congenital Kostman syndrome,
- autoimmune pathologies (lupus erythematosus, rheumatoid arthritis and others),
- hypersplenism,
- various types of anemia,
- biological depletion of the body due to chronic alcoholism, cachexia,
- taking a number of medications.
- A deficiency of eosinophils is caused by:
- some acute bacterial infections,
- burns,
- taking a number of hormonal drugs,
- anemia,
- numerous injuries,
- physical overload.
- A lack of basophils leads to:
- adrenal dysfunction,
- hyperthyroidism,
- chemotherapy,
- some hormonal medications.
When is the test ordered?
Determining the number of leukocytes and one of their varieties, immature granulocytes, is one of the most common laboratory tests. It is carried out as part of a clinical (“general”) blood test, but on the referral the doctor must indicate that a decoding of the leukocyte formula is required.
The study is prescribed in the following cases:
- during routine medical examinations;
- to analyze the general state of immunity, assess the body’s ability to resist infections of a viral and bacterial nature;
- for allergic pathologies;
- for the diagnosis of leukemia and other diseases;
- to assess the effectiveness of therapeutic measures and the dynamics of the pathological process;
- if it is necessary to hospitalize the patient in a hospital;
- before surgery.
A referral to the laboratory can be given by a doctor of any specialty.
Norms of indicators
Immature granulocytes are increased in adults in analyzes and can be in absolute and relative terms. Normally, they should be completely absent from the blood, but a small amount is still allowed.
The relative content of cells of this type on medical forms is indicated under the designation IMM% and is expressed as a percentage of the total number of granulocytes, and the absolute content is IMM#, the units of measurement of which can be g/l or 109/l in different laboratories.
In men
In healthy men, the number of immature cells should not exceed 5% or 0.07*109/l. In boys during puberty, this figure in relative terms can reach 6%.
Immature granulocytes increase in adults and children when the body is sick
With an increase in the content of immature granulocytes, additional examination and clarification of the anamnesis are required in order to determine the cause of the deviation and make a diagnosis. In doubtful cases, the doctor may prescribe a repeat test.
Among women
There is no difference in normal values for men and women, since the leukocyte formula is practically independent of gender. In children, the ratio of mature and immature cell forms differs from adult values.
How to prepare for research
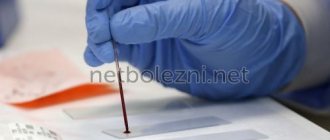
The concentration of immature granulocytes is determined as part of a clinical blood test.
General preparation rules are as follows:
- 12 hours before submitting the biomaterial, you must refuse to eat, you can only drink still water;
- the last meal should be light (early dinner), tea and coffee are excluded;
- During the day before, you should not eat fatty or fried foods;
- 2-3 days (or at least 1 day) before visiting the laboratory you should give up alcoholic beverages;
- per day, it is also necessary to exclude heavy physical activity, visiting a bathhouse, sauna, and try to avoid emotional stress;
- 1 hour before submitting the biomaterial, smoking is prohibited;
- immediately before taking blood, you need to rest for 10-15 minutes; it is also recommended to warm your hands to improve blood circulation.
The analysis is carried out in the morning from 8-00 to 11-00. If other diagnostic or physiotherapeutic procedures are prescribed on the same day, they should be carried out after this.
How the biomaterial is collected
The technique for collecting biomaterial consists of the following sequential steps:
- The patient is seated on a chair at the nurse's table, his left hand is placed on the table.
- The puncture site - the ring finger of the left hand - is wiped with a cotton swab soaked in medical alcohol (or an alcohol wipe). Blood is taken from this finger because it has a synovial vagina that prevents the spread of infections. If this fails, then the fence is made from another finger. In young children, the test can be taken from the heel. In rare cases, blood is taken from the earlobe.
- A puncture is made with a disposable needle in an applicator or with a lancet (sharply sharpened plate). The first method is less painful. The puncture should be made on the side surface of the fingertip, since there are more blood capillaries and fewer nerve endings there.
- The nurse removes the first drop of blood with a dry cloth. It contains many fabric elements, so it is not used. During blood transfusion into the test tube, you should not massage the puncture site so that foreign substances do not get into the biomaterial. To help the blood flow out better, the nurse may apply gentle pressure to the finger in the area above the puncture.
- Blood is drawn into a capillary and transferred to a test tube (or immediately into a test tube with a short capillary, which is subsequently removed from it).
- The puncture site is pressed for 5-10 minutes. alcohol wipe or cotton swab soaked in alcohol.
Decoding analysis responses
Immature granulocytes and interpretation of their blood levels are assessed in conjunction with other clinical data.
Thus, if they are increased by more than 2% in an adult after cardiac surgery, this indicates a high risk of developing infectious and inflammatory complications. When sepsis is detected, an increase in the concentration of immature cells reduces the patient's chances of survival.
On the other hand, there are categories of patients in whom exceeding the 5% threshold may not be a sign of pathology.
These include the following persons:
- women during menstrual bleeding;
- pregnant women;
- newborns;
- patients exposed to chronic stress or constant heavy physical activity.
Reasons for high value
An increased content of immature neutrophils indicates the appearance of pathology. During this period, the body produces an increased number of granulocytes for its own protection.
Sometimes they are elevated for physiological reasons: stress, heavy meals, excessive physical activity.
But the main reasons for increased granulocyte values in adolescents and adults are the following pathologies:
- pyelonephritis, pneumonia, peritonitis, sepsis;
- tuberculosis, typhoid fever, hepatitis;
- skin diseases - dermatitis, psoriasis;
- severe bleeding, major burn;
- intoxication resulting from poisoning, bee stings, poisonous insects, etc.;
- malignant neoplasms.
Taking certain medications (glucocorticosteroids, lithium preparations) can also provoke an increase in indicators.
- Immature granulocytes are reduced - what does this mean?
The greatest influence on the level of leukocytes is exerted by purulent processes and pronounced intoxication of the body.
In a child under 15 years of age, the high content of neutrophils is explained by factors such as:
- ulcerative skin lesions, burns;
- acute infectious pathologies - otitis media, pneumonia, tonsillitis;
- purulent inflammation.
Diseases such as leukemia, acidosis, and anemia have a significant impact on the growth of granulocytes.
Reasons for leveling up
An increase in the concentration of immature granulocytes is observed with the development of pathologies such as:
- malignant processes, leukemia;
- infectious diseases of various localizations (typhoid fever, malaria, tuberculosis, rubella, meningitis, pneumonia, pyelonephritis and others);
- systemic inflammatory response syndrome during major surgical interventions;
- liver diseases - cirrhosis and hepatitis;
- autoimmune disorders;
- extensive burns or heavy bleeding;
- severe intoxication;
- allergy;
- acute inflammatory processes (abscesses, peritonitis, appendicitis, phlegmon and others).
Correction
Conservative therapy
There are no direct ways to normalize the number of neutrophil granulocytes. To combat neutrophilia, it is necessary to treat the underlying disease against which it developed. Short-term neutrophilia after eating, stress or physical work does not require any intervention, as it is not a sign of disease or pathological condition. Neutrophilia resulting from surgery also does not need to be treated. In the case of persistent neutrophilia, you should consult a doctor to find out the cause and prescribe differentiated treatment:
- Antimicrobial (antiparasitic) therapy
. For bacterial infections, antibiotics (amoxicillin, cefixime) are used. For generalized infections (sepsis, bacterial endocarditis), it is necessary to use a combination of 2 antibacterial drugs. In case of helminthic infestation in a child, anthelmintic drugs (mebendazole) are prescribed. - Hemorheological therapy
. For heart attacks of any location caused by thrombosis or thromboembolism, antiplatelet drugs (acetylsalicylic acid), anticoagulant drugs (low molecular weight, unfractionated heparin), and sometimes thrombolytic drugs (alteplase) are used. - Antisecretory and antienzyme therapy
. In order to reduce the secretion of hydrochloric acid in peptic ulcers, proton pump inhibitors (omeprazole, pantoprazole), H2-blockers (famotidine, ranitidine) are used. To suppress the destructive action of proteolytic enzymes of the pancreas in acute pancreatitis and pancreatic necrosis, enzyme inhibitors (aprotinin) are effective. - Anti-inflammatory treatment
. To achieve remission of rheumatological diseases, medications are prescribed that stop the inflammatory process. These include glucocorticosteroids (prednisolone), 5-aminosalicylic acid derivatives (sulfasalazine), immunosuppressants (cyclophosphamide, methotrexate). - Chemotherapy.
For the treatment of malignant tumors, chemotherapeutic drugs (cytostatics, antimetabolites, hormone antagonists) are used in combination with radiotherapy. For oncohematological diseases, a combination of several antitumor agents is necessary.
Surgery
Many diseases accompanied by neutrophilia (mainly acute abdominal pathologies) require emergency surgical intervention - laparoscopic appendectomy, laparotomy and suturing of the ulcerative defect, cholecystectomy, opening and drainage of the abscess, etc. For myeloproliferative pathologies, in case of ineffectiveness of conservative therapy, they resort to stem cell transplantation cells.
What could affect the validity of the study?
The following factors may affect the results of the analysis:
- patient failure to comply with preparation rules;
- use of medications (you must notify your doctor about taking them in advance; you may need to stop taking them a few days before donating blood);
- laboratory technician errors - uneven distribution of blood cells on the smear (this depends on the qualifications of the personnel), incorrect counting of immature granulocytes, statistical error.
Blood testing in automatic analyzers is the most preferable, since up to 30,000 cells are studied, while with the microscopic method - only 100.
How much does the study cost, where is it carried out?
A test to determine the level of immature granulocytes in the blood can be carried out in any laboratory specializing in diagnostic procedures.
The average cost of a clinical blood test with a leukocyte formula in commercial medical institutions is about 400 rubles. If blood must be drawn from a vein, you will need to pay an additional 130-250 rubles. Some laboratories provide this service by visiting the patient’s home.
Classification
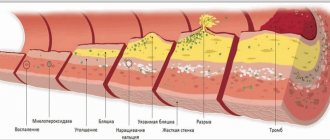
Neutrophil leukocytes themselves come in two main types: segmented (mature) and band (young). Band neutrophils normally make up from 1 to 5% of the total number of leukocytes, segmented neutrophils - from 35 to 65%. Based on the ratio of young and mature cells, neutrophilia are distinguished with and without nuclear shift. A nuclear shift to the left implies an increase in the number of young forms of neutrophils and is divided into the following types:
- Hyporegenerative
. A slight increase in band neutrophil leukocytes. The cause is infectious, inflammatory diseases with a mild course. - Regenerative
. It is characterized by the appearance of metamyelocytes in the blood (intermediate forms between myeloblastic cells and granulocytes). Occurs during infections with moderate severity (typhoid fever, pneumonia). - Hyperregenerative
. Severe hyperactivation of the bone marrow granulocyte lineage with impaired granulocyte maturation. In the blood, the number of band neutrophils, metamyelocytes, promyelocytes is sharply increased, and myeloblasts are sometimes present. Possible aneosinophilia (complete absence of eosinophils). This form of neutrophilia is observed at the very beginning of purulent-inflammatory processes (sepsis, abscesses, phlegmon). - Degenerative
. Along with the increased number of band leukocytes, a large number of destructively altered segmented neutrophils (toxic granularity, pyknosis of nuclei) appear in the blood. Indicates inhibition of the functional activity of the bone marrow. Characteristic of the height of severe infections.
With neutrophilia, which has a nuclear shift to the right, the hemogram shows the absence of young forms of granulocytes and the appearance of hypersegmented (containing more than 5 segments) neutrophils. Neutrophilia without nuclear shift is accompanied by an increase in only segmented neutrophils. In relation to other types of leukocytes, the following are distinguished:
- Relative neutrophilia
. An increase in the percentage of neutrophils (in adults more than 75%, in children under 5 years of age - more than 55%) in the leukocyte formula, the total number of leukocytes is normal. - Absolute neutrophilia
. An increase in the number of neutrophils while simultaneously increasing the level of leukocytes.
Normalization of indicators
Abnormality in itself for immature granulocytes is not diagnostically valuable. A pathological violation of indicators must be accompanied by other symptoms. To identify the cause of a high level of immature cells, additional instrumental and laboratory diagnostics are necessary.
In this regard, independent treatment is not recommended, since diseases in which changes in granulocytes occur are diverse in nature and require a completely different therapeutic approach, both conservative and surgical. Below are the most common causes and remedies for this condition.
For preventive purposes, it is necessary to systematically undergo medical examinations for early detection of pathologies, adhere to a healthy lifestyle, avoid infectious diseases, and strictly follow doctor's instructions in the presence of diseases.
Medicines
The table below shows the main methods of treating diseases in which the level of immature granulocytes increases:
| Group of diseases | Disease | Essential drugs |
| Infectious pathologies | Typhoid fever | Antibacterial agents: fluoroquinolones (Ciprofloxacin, Pefloxacin, Ofloxacin, Gatifloxacin), cephalosporins (Ceftazidime, Ceftriaxone, Cefotaxime, Cefixime), macrolides (Azithromycin) Gastrointestinal motility stimulants (Domperidone, Metoclopramide) Enterosorbents (Polymethylsiloxane polyhydrate, Rekitsen-RD, Pektovit) Antidote Dimercaprol |
| Malaria | Antimalarial drugs (Chloroquine, Hydroxychloroquine, Primaquine and others) | |
| Tuberculosis | Anti-tuberculosis drugs (Isoniazid, Rifampicin, Rifabutin, Pyrazinamide and others) | |
| Rubella | There is no specific treatment; Paracetamol is used to eliminate symptoms | |
| Meningitis | Antibacterial agents (Penicillin, Ampicillin, cephalosporins, carbapenems) | |
| Pneumonia | Broad-spectrum antibiotics (cephalosporins, macrolides, carbapenems, fluoroquinolones) | |
| Pyelonephritis | Antibacterial agents (Penicillin, aminoglycosides, fluoroquinolones, cephalosporins) Painkillers, antipyretics and other drugs for symptomatic treatment | |
| Liver diseases | Cirrhosis | Hepatoprotectors (Essentiale Forte, Phosphogliv, Antraliv, Essliver, Phosphonziale, Rezalut Pro, Gepatrin) |
| Hepatitis | Hepatoprotectors (Methionine, ursodeoxycholic acid, essential phospholipids) Means for normalizing the gastrointestinal tract (lactulose, lacto- and bifidobacteria) | |
| Burns | — | Infusion therapy Local antibacterial drugs (hydrogen peroxide, potassium permanganate, nitrofurans, Levomycetin, Erythromycin, Sulfonamides) Painkillers |
| Intoxication | — | Enterosorbents (activated carbon, Filtrum and others) Antidotes |
| Allergy | — | Antihistamines (Suprastin, Tavegil, Diphenhydramine, Diazolin, Claritin, Fenistil and others) |
Folk remedies
Immature granulocytes are elevated in an adult for various reasons. To eliminate them, appropriate traditional medicine recipes are selected.
Oncological pathologies are treated using plant poisons:
- Decoction of celandine. 1 tbsp. l. herbs of this plant, the same amount of plantain, 2 tbsp. l. lemon balm, nettle leaves, horsetail, 1 tbsp. l. dandelion roots are mixed. 2 tbsp. l. collection pour 3 tbsp. water and boil. Drink 1/3 tbsp of the decoction. 3 times a day before meals.
- Hemlock tincture. The inflorescences and leaves of the plant are placed in a glass jar and filled with alcohol (ratio 1:3). Keep for a month, then filter. Take the product on an empty stomach in the morning, starting with 1 drop diluted in 100 g of water. Gradually this amount is increased to 30-40 drops.
For infectious diseases, the following recipes are used:
- Pyelonephritis - decoctions of bearberry (2 tbsp. per 0.5 l of boiling water, drink 2 tbsp. 3-4 times a day), lingonberry (2 tbsp. per 1.5 tbsp. boiling water, drink as follows) same scheme), juice or fruit drink from cranberries (2 tbsp. per day).
- Pneumonia:
- 2 tbsp. Chop the peeled garlic, squeeze out the juice and pour it into a jar with 1 liter of Cahors. Leave for 1 week. Drink 1 tbsp. l. 3 times a day.
- Chop 2 large onions, pour 1 tbsp. hot milk, boil for 5 minutes. Strain, take 1 tbsp. l. every hour (in acute illness).
The following effective methods are used for liver pathologies:
- Cut off the top of a medium-sized ripe pumpkin, clean out the seeds from the inside and fill it with flower honey. Close the resulting “barrel” and keep it in a dark, dry place for 2 weeks. Take this remedy for a month.
- Squeeze beetroot and carrot juices, mix them in a ratio of 1:5. Drink 1 tbsp. before meals 3 times a day.
- Chop young branches of weeping willow, put in a saucepan and pour 3 liters of boiling water. Leave for 1 night, strain. Drink throughout the day instead of tea. Keep refrigerated.
Diet therapy
General nutritional rules for the above diseases are as follows:
- food intake should be regular, in small portions;
- Steamed and boiled dishes are preferable;
- the diet should be nutritious and varied;
- It is necessary to exclude fried, canned, spicy, fatty foods, coarse fiber, as they irritate the gastrointestinal tract.
Dietary recommendations for this symptom depend on the characteristics of the disease. So, with pyelonephritis, it is necessary to follow a dairy-vegetable diet; salt intake is limited to 5 g per day. In case of liver cirrhosis, the protein content should be at least 1 g per 1 kg of body weight daily. There are other nutritional features that your doctor should be familiar with.
Causes of neutrophilia
Physiological reasons
There is a so-called physiological neutrophilia, or pseudoneutrophilosis. Its occurrence is not associated with increased neutrophil production, but with their redistribution, i.e. a change in the ratio of the parietal and circulating pools of neutrophils towards the latter. Pseudoneutrophilia is observed under stress, intense physical activity, exposure to heat or cold, and after eating. Also, neutrophils are often increased during pregnancy and in a newborn child.
Infections in children
Due to a physiological decrease in the level of neutrophils due to leukocyte crossover, a child of preschool age (up to 5-6 years) has an increased susceptibility to bacterial infections. In children, neutrophils increase mainly with scarlet fever and streptococcal sore throat. A dangerous infection such as diphtheria is quite common in the pediatric population. Parasitic infestations (ascariasis, enterobiasis, toxocariasis) are also common among preschoolers. In these diseases, in addition to neutrophilia, high eosinophilia is observed in the blood.
Infections in adults
Most often, neutrophils are increased during bacterial infections. The main function of neutrophils is anti-infective protection of the macroorganism, namely, the destruction of bacteria. They also take part in the fight against viruses and parasites. Migrating through the vascular wall, neutrophils are directed to the site of localization of the pathogenic microorganism. By releasing cytokines and inflammatory mediators, neutrophils activate other components of the immune system (complement, T-B lymphocytes).
Neutrophil leukocytes first phagocytize (absorb) the infectious agent, then secrete degradation enzymes (lysozyme, lactoferrin, phosphatases) and reactive oxygen species (superoxide anion, hydroxyl radical, hydrogen peroxide), which contributes to the death of microorganisms. Neutrophilia increases rapidly, reaches a maximum parallel to the height of the disease, and gradually decreases after antibacterial therapy.
The most common cause of neutrophilia in adults is acute localized bacterial (pneumonia, sinusitis, pyelonephritis) or specific infections (typhoid fever). Moderate neutrophilia is typical for them. Less commonly, the cause is severe generalized infections (bacterial endocarditis, sepsis, meningococcal meningitis), characterized by high neutrophilia with a hyperregenerative or degenerative shift.
Acute surgical pathologies
Quite often, neutrophils are increased in acute abdominal pathology (cholecystitis, pancreatitis, perforation of a stomach or duodenal ulcer), purulent processes (phlegmon, abscess). Neurophilia in a child often occurs with appendicitis. An increase in the number of neutrophil leukocytes in these diseases acts as a reaction to the inflammatory process. A correlating relationship between the severity of inflammation and the degree of increase in neutrophils has been precisely established. Usually there is high neutrophilia with a degenerative shift of the leukocyte formula to the left, which quickly regresses after emergency surgery. However, neutrophils may remain within normal limits.
Tissue damage or breakdown
Such conditions include infarctions of various organs (myocardium, lungs, intestines), abdominal operations, gangrene, pancreatic necrosis. The cause of neutrophilia is stimulation by decay products of granulocytopoiesis in the bone marrow. An additional role is played by reactive neutrophilia, which occurs due to the release of large amounts of stress hormones (catecholamines, glucocorticosteroids) into the blood.
Also, the occurrence of neutrophilia in these conditions is facilitated by the addition of a secondary infection (for example, pneumonia due to pulmonary infarction). The degree of neutrophilia correlates with the volume of damaged, necrotic tissue, often reaches very high values (especially in a child), can persist for a long time, and decreases with recovery.
Rheumatological diseases
Neutrophilia can be observed in some chronic inflammatory pathologies of a rheumatic nature. There is an assumption that mediators, cytokines, and autoantibodies that are formed during rheumatic inflammation stimulate the bone marrow production of neutrophilic granulocytes. Typically, the appearance of neutrophilia along with other laboratory markers, such as an increased erythrocyte sedimentation rate and C-reactive protein, indicates an exacerbation of the disease.
After anti-inflammatory treatment, the concentration of neutrophils gradually returns to normal. In adults, especially high neutrophilia is characteristic of acute gouty attack, necrotizing vasculitis (polyarteritis nodosa, granulomatosis with polyangiitis). In a child, neutrophils are enlarged most often due to dermatomyositis.
- Joint diseases
: rheumatoid arthritis, ankylosing spondylitis (ankylosing spondylitis). - Diffuse connective tissue diseases (collagenoses)
: systemic lupus erythematosus, systemic scleroderma, Sjogren's disease. - Inflammatory bowel diseases
: Crohn's disease, ulcerative colitis. - Systemic vasculitis:
Takayasu's nonspecific aortoarteritis, Horton's giant cell arteritis.
Oncological diseases
Neutrophilia can sometimes indicate a malignant tumor. Its occurrence is promoted by two mechanisms - the breakdown of tumor tissue and the ability of some tumor cells to secrete granulocyte colony-stimulating growth factors (paraneoplastic syndrome). Neutrophilia most often occurs in patients with breast, lung, colon, and ovarian cancer. Neutrophilia increases slowly as the tumor grows, reaches moderate numbers, gradually regresses after chemotherapy, or quickly returns to normal after surgical removal of the neoplasia.
Hematological diseases
High neutrophilia is observed in oncohematological diseases. It can reach very high numbers (up to 100 thousand) in myeloproliferative diseases (acute, chronic myeloid leukemia). In lymphoproliferative pathologies (non-Hodgkin's lymphomas, lymphosarcoma), neutrophilia is slightly less pronounced and is almost always accompanied by absolute lymphocytosis. In a child, the most common cause is lymphogranulomatosis (Hodgkin's lymphoma).
In addition to neutrophilia itself, in patients with acute leukemia, a basophilic-eosinophilic association, a large number of blast cells and the absence of intermediate forms (leukemic failure) are found in the blood. The mechanism of neutrophilic leukocytosis lies in the malignant transformation of a hematopoietic stem cell. Granulocyte counts return to normal only after several courses of chemotherapy or bone marrow transplant.
Rare causes
- Endocrine disorders
: Cushing's disease or syndrome, thyrotoxic crisis. - Blood diseases
: hemolytic anemia, polycythemia vera, Addison-Birmer pernicious anemia. - Endogenous intoxication
: chronic renal failure, liver failure, diabetic ketoacidosis. - The phenomenon of bone marrow hyperactivation
: after agranulocytosis, treatment of megaloblastic anemia. - Use of medications
: adrenaline, cardiac glycosides, glucocorticosteroids, lithium. - Intoxication with mercury, lead
. - Exposure to ionizing radiation
.
Prognosis and complications
If a slight increase in the level of immature granulocytes within normal limits is not accompanied by other pathological symptoms, then this condition does not pose a danger to human health.
With advanced pathologies, serious metabolic disorders, decreased immunity and other complications accompanying the disease are possible (up to death in hepatitis, cirrhosis, malignant and infectious processes).
The prognosis of the disease depends on its type, timely diagnosis and treatment. Therefore, if a leukocyte shift is detected in the blood, it is necessary to undergo a full examination in accordance with the doctor’s prescriptions.
Immature granulocytes in themselves are not a sign of a specific disease. If they are elevated in an adult, then additional examination is required. The results of the analysis are taken into account in conjunction with other information. One of the most common reasons for an increase in their number is infectious and inflammatory pathologies.
Article design: Vladimir the Great
Reasons for deviation from the norm
An increase in the level of immature granulocytes clearly indicates the onset of inflammation in the body. The immune system turns on and begins to actively form neutrophils to remove pathogens. There are reasons for the different origins of immature granulocytes that characterize deviations from the norm.
An increase in indicators is observed when:
- poisoning, intoxication;
- severe bleeding;
- thermal, chemical and other types of burns;
- pulmonary, myocardial infarction;
- malignant formations;
- abscesses, peritonitis;
- blood diseases;
- An increase is also possible after taking certain medications and as a reaction to a given vaccination.
Intoxication of the body
However, neutrophils can also increase in cases of ordinary physical processes:
- second trimester of pregnancy, childbirth;
- increased physical activity;
- period;
- stress;
- after a heavy meal.
Immature neutrophils are elevated in newborns, this is due to the fact that, being in a favorable intrauterine environment, the child experiences unprecedented stress after birth.
The small organism is just beginning its work in new conditions, therefore it responds to the shock situation by increasing the production of granulocytes.
In all other episodes, an increase in indicators should be a guide for medical workers and parents to action, namely a comprehensive examination.
- Granulocytes - what are they? Granulocytes in the blood: increased, decreased, normal
The number of young neutrophils in a general blood test in children tends to increase when:
- acute otitis media;
- pneumonia;
- appendicitis;
- burns;
- purulent inflammations and the like.
A slight increase in granulocytes indicates the initial stage of the disease. But a rapid, sharp increase indicates blood poisoning.
A decrease in the level of granulocytes can be observed with the following ailments:
- hepatitis;
- diabetes mellitus;
- infectious diseases - sore throats, meningitis, acute respiratory infections, influenza;
- tuberculosis;
- skin diseases;
- blood leukemia in the acute stage;
- low hemoglobin indicates anemia of various origins, etc.
A low number of immature granulocytes signals lead poisoning, radiation sickness, and other autoimmune diseases (lupus erythematosus, rheumatoid arthritis, etc.).
Experts do not recommend vaccinating children if cases of decreased granulocytes are detected during a blood test.
A suspicious change in the number of immature granulocytes towards an increase or decrease indicates the presence of serious diseases, so you must definitely visit a hematologist, undergo a comprehensive examination and begin adequate treatment. You should not self-medicate.
Mandatory consultation with a doctor