Probing (or “catheterization”) of the heart is an invasive technique that is practiced in cardiac surgery and is aimed at inserting a catheter into the right or left parts of the organ for diagnostic purposes. In the process, the surgeon creates a puncture in the brachial or femoral artery (to diagnose left cavities) or the ulnar or femoral vein (to diagnose right cavities). A catheter is inserted through it under the control of an X-ray machine and ECG. The procedure allows you to evaluate the condition of the septum and valves of the heart, take blood samples and conduct chamber studies with the introduction of a contrast agent.
The Department of Cardiovascular Surgery CELT invites you to undergo probing of the heart cavities in Moscow. It began its work almost three decades ago and today offers a wide range of services for the diagnosis and treatment of cardiovascular diseases. It welcomes leading domestic specialists, candidates and doctors of sciences with decades of scientific and practical experience. They have modern equipment in their arsenal that allows them to accurately diagnose and carry out treatment in accordance with international standards.
Probing of the heart cavities - 21,000 rubles.
At CELT you can get a consultation with a cardiovascular surgeon.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Probing of the heart cavities: indications and contraindications
Today, catheterization of the cardiac cavities is one of the most frequently performed procedures in cardiac surgery. In European countries alone, it is performed on almost a million patients every year! The use of modern equipment and the high qualifications of our specialists allow us to minimize the risk of complications after surgery. Depending on the situation, it can be not only diagnostic, but also therapeutic.
Indications
- Assessment of left ventricular function and determination of the degree of ischemic disease;
- Diagnosis of congenital and acquired heart defects;
- Determination of narrowing or insufficiency of the aorta before surgery;
- Confirmation/exclusion of the diagnosis of ischemia in patients who suffer from chest pain of unknown etiology;
- Collection of data during the diagnostic process that confirms and complements the results of other studies;
- Diagnosis of pulmonary hypertension, determination of its type and severity;
- Assessing the possibility of heart or lung transplantation.
Contraindications
There are no absolute contraindications to this procedure. All of them are relative and depend on the individual indications of the patient. Whether to carry it out or not is decided by the doctor himself, assessing and comparing the risks. He may refuse it altogether if:
- The patient's blood electrolyte levels are abnormal;
- There is a diagnosis of acute renal failure;
- The patient suffered an acute stroke;
- Gastrointestinal bleeding was detected;
- The patient has an individual intolerance to contrast agents;
- The level of cardiac glycosides in his blood exceeds the norm.
Our expert Burkert Pieske is director of the Clinic for Internal Medicine and Cardiology at the German Heart Center in Berlin. Private practitioners in Berlin most often recommend this clinic to their patients for inpatient treatment using a catheter for cardiac catheterization (a 2015 survey of doctors conducted by the Tagesspiegel newspaper and the non-profit organization City of Health Berlin). Author: MAGDALENA WEBER
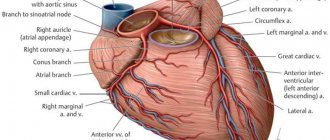
EXPLANATION The cardiac catheter (catheterization) is a very flexible plastic probe up to 1.50 meters long and about three millimeters thick. With this probe, doctors can both recognize and treat heart disease. For example, it is often used for coronary heart disease: If the thin coronary vessels of the heart (coronary arteries) become severely narrowed due to fatty deposits or calcification, they can no longer supply the heart muscle sufficiently with oxygen and nutrients. As a consequence, the function of this vital muscle, the contraction of which makes possible the pumping function of the organ - the heartbeat, so to speak - is increasingly limited. If the vessels are completely clogged, then the muscle tissue for which they are responsible for the blood supply dies and this leads to the development of a heart attack. By using a cardiac catheter, doctors can detect these narrowings and widen them again so that blood can flow freely again. To make sure that the vessels remain patent after the procedure, doctors may additionally implant a stent. In this case, we are talking about a support structure for blood vessels, which, with the help of a catheter, is advanced to the desired area in the heart.
Coronary heart disease is the most common heart disease, and, above all, in industrialized countries the most common disease in general. In Germany, almost five percent of people have such circulatory problems caused by deposits in the coronary arteries. “In the group of people over 60 years of age, this percentage is probably even higher,” says Burkert Pieske, director of the Clinic for Internal Medicine and Cardiology at the German Heart Center in Berlin and at the campus of the Charité University Hospital Virchow-Klinik in the Berlin-Wedding district. However, only a general assessment is possible here, since not every sick person immediately causes symptoms of the disease. However, in general, coronary heart disease is one of the most common causes of death, especially in developed industrial countries.
The catheter (1) is a plastic probe up to 1.50 meters long and with a diameter the thickness of spaghetti. It is injected into the coronary vessels of the heart (2), also called the coronary arteries, through the aorta. Through this access, the doctor can inject a contrast agent, due to which the vessels become visible on an x-ray, including visualization of narrowings (3) in these vessels. Around the catheter is a balloon, above which is a covered stent (white lattice). DRAWING BY FABIEN BARTEL
Around the catheter is a balloon, above which is a covered stent (white lattice). To dilate narrowed blood vessels, the doctor places a catheter with a tiny balloon (4) at the tip to the affected area. There the balloon is inflated and thus the narrowing opens. To prevent the vessel from immediately becoming blocked again, a stent can be used (5). The support structure for the vessel opens together with the balloon, is pressed against the wall of the vessel and secured there. DRAWING BY FABIEN BARTEL
SYMPTOMS A typical symptom of coronary heart disease is the so-called angina pectoris (Angina pectoris). The name Angina pectoris comes from Latin and means “angina pectoris”. Indeed, in addition to pain in the heart area, which often occurs in the form of attacks, for example, during physical activity, in many cases a dull, pressing feeling in the chest also occurs. The pain may radiate to other parts of the body, such as the neck or arms. During such an attack, many patients suffer from lack of air, they feel weak, sweating increases, and pallor appears. Feelings of anxiety may also occur. In addition, angina also manifests itself in the form of intense stomach pain, nausea, poor performance and fatigue, especially in women. Typical chest pain radiating to the left arm is less pronounced in women.
“At first, angina pectoris occurs mainly during physical exertion or in a state of excitement,” says Mr. Pieske. “When the person calms down, the symptoms go away again.” However, if an attack occurs even at rest, this is clearly a warning sign - and an emergency. “In this case, the patient should definitely go to the hospital, as he is at risk of a heart attack.”
CAUSES Coronary heart disease usually develops over a longer period of time. This is why this disease primarily affects older people. Indeed, throughout life, substances such as cholesterol or calcium are deposited on the walls of the arteries - and, consequently, in the coronary vessels. These accumulations of fat and calcium can stick together and form a relatively hard mass that doctors call atherosclerotic plaque. “Atherosclerotic plaques damage the vessel and make it harder, so that it can no longer expand, for example if the heart muscle needs more blood during exercise,” says cardiologist Mr Piske. The more this calcification of the arteries (arteriosclerosis) progresses in the coronary vessels, the narrower the vessels become - and the worse the blood supply to the heart muscle.
For men, age over 45 years is a risk factor that contributes to the disease; for women, it is age over 55 years. This difference is likely hormonally determined. So experts proceed from the fact that the female hormone estrogen performs a kind of protective function in relation to the heart and blood vessels. However, exactly how this process functions remains unclear.
Other risk factors that contribute to the development of coronary heart disease, along with advancing age, are primarily excess weight, elevated blood lipids, high blood pressure and diabetes. “Smoking also has a very negative effect on blood vessels,” says Mr. Pieske. Therefore, smokers often suffer from coronary heart disease at a young age.
DIAGNOSIS To prevent life-threatening consequences such as heart attack, it is very important to recognize coronary heart disease - or an increased risk of developing the disease - as early as possible. Therefore, it is recommended to carry out regular preventive examinations - even in the absence of acute complaints. For example, for patients over 35 years of age, health insurance funds pay for a general preventive medical examination by a family doctor every two years, which also includes important cardiac tests such as measuring blood pressure or determining blood cholesterol levels.
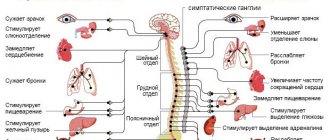
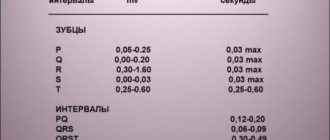
When diagnosing coronary heart disease, we first of all talk about a conversation with the patient (history taking), during which the doctor asks questions about the presence of possible risk factors and complaints. This is usually followed by a physical examination and blood tests, blood pressure measurements, and an electrocardiogram (ECG), which can visualize the heart's electrical currents. To substantiate the initial suspicion, other methods are used, such as an exercise ECG (ergometry) or ultrasound examination of the heart (echocardiography).
To determine whether there is insufficient blood supply to the heart during exercise, doctors may also take magnetic resonance imaging (MRI) images or do what is called a myocardial perfusion (blood supply) scintigraphy. In this process, the blood supply to the heart is visualized using a slightly radioactive substance that is injected into the bloodstream. Under certain circumstances, a computed tomography (CT) scan may be performed.
And finally, another informative diagnostic method is a study using a catheter to probe the heart, the so-called angiography. In this study, doctors use a thin needle to access an artery in the groin or shoulder joint under local anesthesia. “From there, a thin catheter probe is advanced to the heart,” says Mr. Pieske. The entire procedure is carried out under x-ray control - in addition, x-rays also allow you to see possible risk areas. For this purpose, a contrast agent is injected into the blood, making the blood vessels visible on the X-ray screen. If doctors find areas of narrowing in the coronary vessels of the heart, they can immediately treat them on the spot with a catheter.
TREATMENT Incipient coronary heart disease can usually be treated with medications. In addition, patients should minimize risk factors such as smoking and excess weight. However, if the coronary arteries are already narrowed to such an extent that these measures are no longer enough or there is even a threat of a heart attack, then in this case a catheter is used to probe the heart: with its help, doctors can dilate the affected vessel again. “To do this, the empty balloon is advanced with the help of a catheter to the site of narrowing,” says Dr. Pieske. There it is “inflated” under high pressure and thereby pushes the walls of the vessel apart - the artery again becomes passable. To ensure that the vessel continues to remain patent, doctors can use a catheter to install a support structure for the vessel - a stent. Often, dilation of the artery and implantation of the stent are performed in one surgical procedure.
There are several types of vascular support structures: Stainless steel drug-eluting stents are designed to provide long-term prevention of the re-formation of atherosclerotic plaques. Another form is the so-called absorbable stents. They consist of a sugary substance and dissolve on their own over time. This way, the foreign body does not remain in the heart for a long time, however, according to Mr. Piske, this method is not suitable for all patients: “If the coronary arteries are already heavily calcified and hardened, they can crumble the self-resorbable stent.” Therefore, stents made of steel are usually used. To prevent rejection reactions or re-narrowing of the vessel, stents are coated with drugs that are slowly released into the blood. To avoid complications such as thrombosis in the stent and in the long term, after implantation, patients must take medications to inhibit blood platelets (platelets), which are important for the blood clotting process.
Currently, cardiac catheterization and stent implantation have already become standard procedures for cardiologists. “However, there are, of course, certain risks,” says expert Pieske. For example, at the puncture site in the groin or elbow area, minor damage may occur, resulting in bruising. More serious - but also very rare - are possible catheter injuries to large vessels on the way to the heart or to the coronary vessels themselves, which in extreme cases can lead to a stroke or heart attack. In addition, another intervention may be required, either because deposits will reappear in the operated area and re-narrow the vessel (re-stenosis), or because a narrowing will occur in another area in one of the three coronary vessels hearts.
Source - https://www.tagesspiegel.de/themen/arztbriefe/arztbrief-herzkatheter/13465636.html
Types of catheterization of cardiac chambers
There are two of them: catheterization of the right and left parts of the heart.
| Catheterization of the left chambers of the heart | Catheterization of the right chambers of the heart |
Allows you to determine the anatomical features of the structure of the coronary artery and identify coronary artery disease. Thanks to it, you can determine and evaluate the following parameters:
| Allows you to evaluate the following parameters:
The procedure is used for heart transplantation or mechanical support. Thanks to it, you can estimate the pressure in:
|
What does an ultrasound of the heart show?
The resulting parameters allow you to determine:
- hypertrophy of the LV walls;
- regurgitation of blood through the valves;
- tumors, blood clots, scars, aneurysms;
- blood flow condition;
- valve condition;
- degree of myocardial contractility;
- size of the heart cavities;
- state of the LV pumping function in a dynamic state.
It is considered normal if:
- there is no fluid in the pericardium;
- the size of the final section of the pulmonary artery is within 1.8-2.4 cm; trunk - up to 3 cm;
- ejection fraction is 55 – 60%;
- the volume of the pancreas at the final stage of relaxation of the heart (diastole) ranges from 0.9 to 2.5 cm;
- thickness of the interventricular septum in the final stage of diastole from 0.5 to 1.12 cm
- the final section of the aorta in diameter is 2 – 3.7 cm
- the thickness of the posterior wall of the LV at the final stage of relaxation of the heart (diastole) varies from 0.6 to 1.12 cm
- the change in the movement of the posterior wall of the LV towards contraction (systole) is 0.91 – 1.41 cm
- the size of the LV cavity in the final stage of relaxation (diastole) ranges from 3.51 to 5.7
- cardiac output (MCV) must be no less than 3.5 and no more than 7.5 l/min
- cardiac index ranges from 2 to 4.1 l/m2
- the diameter of the terminal part of the pulmonary artery is from 1.8 to 2.4 cm, its trunk is up to 3 cm
- the blood flow speed through the carotid artery is 22 cm/s with an error of +-5 cm/s
- there are no manifestations of regurgitation and dysfunction of the papillary muscles, growth on all valves.
The degree of discrepancy with normal values is determined by a sonologist, but the final diagnosis is made by a cardiologist taking into account the information received and based on other symptoms. The disease cannot be diagnosed by ultrasound alone.
Preparation for probing the cavities of the heart
It is necessary to ensure that this procedure does not lead to any complications. Within its framework, CELT specialists prescribe the patient to undergo a number of diagnostic tests:
- General and biochemical blood tests;
- Chest X-ray;
- Electro- and echocardiography;
- Magnetic resonance imaging of the heart.
The above allows you to determine the levels of platelets and hemoglobin in the blood, as well as the correct functioning of the kidneys, liver, heart, lungs, and aorta. The patient must inform the attending physician about his individual intolerance to seafood, contrast agents, iodine-containing and any other pharmacological drugs. In addition, he should be informed if he is taking medications for erectile dysfunction or if he is pregnant.
Additional preparation for cardiac probing is required for those under one year of age or over seventy years of age, as well as for patients who suffer from:
- Type 1 diabetes mellitus;
- Diseases of the blood vessels of the brain;
- Severe pulmonary or renal failure.
In what situations should you undergo a cardiac ultrasound?
- Changes in ECG indicators.
- Heart murmurs.
- A slight increase in body temperature in the absence of inflammatory processes in the throat, nose, ear or kidneys.
- Arrhythmia.
- An x-ray of the heart showed a change in its shape and size, as well as in the vessels extending from it.
- Hypertension.
- Predisposition to hereditary heart diseases.
- Possible changes in cardiac structures.
- Fainting, swelling, shortness of breath, dizziness.
- Pain in the left half of the chest and behind the sternum.
- Risk of heart tumors.
- After myocardial infarction.
- Effusion pericarditis.
- Angina pectoris.
- Diagnosis of cardiomyopathy and its type.
- To detect true or false cardiac aneurysm.
It is extremely important to carry out this procedure after a myocardial infarction to determine how many muscle cells have died.
ECG and ultrasound of the heart should be performed by people in stressful situations, experiencing severe emotional and physical stress.
EchoCG has no age restrictions. It is prescribed to children if a congenital heart defect or a change in its structure is suspected, which often occurs during the period of active growth of the child.
EchoCG is prescribed for pregnant women, because allows you to identify heart defects in the fetus in the womb. The procedure is painless and does not cause harm.
Heart ultrasound is a mandatory procedure during pregnancy if:
- There was a history of spontaneous abortions.
- Diabetes.
- Hereditary predisposition to heart disease.
- In the 1st and 2nd trimester, the woman was forced to take antiepileptic drugs and antibiotics.
- The analysis revealed high titers of antibodies to rubella, or the woman had it during pregnancy.
Fetal echocardiography is prescribed at 18-22 weeks. Children undergo it when the above symptoms appear.
Technique for probing the cavities of the heart
The patient assumes a supine position, the medical staff fixes electrocardiography electrodes on him, installs an intravenous infusion system and starts the administration of a five percent glucose solution or sodium chloride solution. Next steps:
- After anesthetizing the area where the catheter is inserted, the surgeon makes a small incision in the skin and inserts it into the blood vessel, carefully moving it towards the heart and checking his actions through an X-ray machine;
- Once the catheter has reached the desired location, he injects a contrast agent, which allows for good visualization of the cardiac structures and arteries;
- During the procedure, basic physiological indicators (heart rate and contractions, blood pressure and respiratory rate) are monitored every fifteen minutes;
- Upon completion of the diagnosis, the doctor removes the catheter and applies a tight bandage for half an hour.
If the patient begins to feel nauseous during the procedure, they are asked to cough to reduce the effect. Sometimes, after the administration of contrast, arrhythmia may develop, which can be eliminated by deep breathing. It also makes it possible to easily install a catheter into the pulmonary artery and makes visualization of the heart clearer.
Technique
How is catheterization performed?
The left heart catheterization procedure is performed through a percutaneous approach from the femoral, radial, brachial, or axillary artery. Right heart catheterization is usually performed through a percutaneous approach from the femoral, internal jugular, or subclavian vein.
Before cardiac catheterization, a puncture of the cubital vein in the arm is performed with the installation of an intravenous infusion system. Through it, the patient receives a sedative, which helps to relax or fall asleep during the procedure, or a drug for general anesthesia.
If general anesthesia is not used, the doctor will administer local anesthesia at the site where the catheter will be inserted. This location may be in the upper thigh, arm, neck, or under the collarbone. The doctor inserts a needle into a blood vessel at the access site. The guide wire is then inserted into the needle and the needle is removed. The doctor then places a small tube (sheath) in the blood vessel around the guide. The guide is removed and the catheter is inserted through the sheath. Under continuous video fluoroscopic control, the doctor advances the catheter to the heart and then into the ventricle or coronary artery.
Once the catheter has been guided to the desired area, the doctor can use it for tests or treatment.
Additional vascular access approaches
Rarely, severe atherosclerotic disease may affect both the upper and lower extremities and obstruct vascular access in normal locations. In such cases, access to the descending aorta can be achieved using a translumbar approach, and coronary angiography can be performed using standard catheter shapes.
Catheterization of the left atrium and left ventricle can be performed through a transseptal approach. Transseptal catheterization is useful if the patient has a mechanical aortic valve or if true left atrial pressure needs to be obtained. The intracardiac septum is pierced with a needle, and the catheter is advanced into the left atrium and ventricle. The operator must have a clear understanding of the radiographic anatomy of the heart to avoid puncture of adjacent structures (eg, right atrium free wall, coronary sinus, or aortic root).
Transradial catheterization in clinics in Belgium
Since its first introduction in 1989, the transradial approach (radial artery or vein puncture) to coronary angiography has become increasingly popular compared with the transfemoral (femoral artery or vein puncture) approach in clinics in Europe and the United States.
In cardiac centers in Belgium, this approach is also considered preferable and most procedures are performed using it.
Several randomized controlled trials and meta-analyses have demonstrated with the transradial approach:
- reduction in mortality;
- reduction of bleeding;
- reducing the number and severity of complications at the access site;
- reducing the length of hospital stay.
The results were replicated in routine diagnostic and percutaneous interventional procedures, as well as in the emergency setting of ST-segment elevation myocardial infarction.
Radial access procedures also improve patient comfort, reduce post-procedural bed rest and, ultimately, length of hospital stay.
How long does the procedure take?
The cardiac catheterization procedure usually takes about 30 minutes (1-2 hours if a therapeutic procedure is performed). But the preparation and recovery time takes several hours. The patient spends the entire day in the hospital.
Our doctors
Drozdov Sergey Alexandrovich
Cardiovascular surgeon, phlebologist, Doctor of Medical Sciences
47 years of experience
Make an appointment
Malakhov Yuri Stanislavovich
Doctor - cardiovascular surgeon, phlebologist, Honored Doctor of the Russian Federation, Doctor of Medical Sciences, doctor of the highest category
Experience 36 years
Make an appointment
Babunashvili Avtandil Mikhailovich
Cardiovascular surgeon, head of the department of cardiovascular surgery, Doctor of Medical Sciences, Professor, Honored Doctor of the Russian Federation
34 years of experience
Make an appointment
Kartashov Dmitry Sergeevich
Doctor - radiologist, angiosurgeon, head of the office of X-ray surgical methods of diagnosis and treatment
31 years of experience
Make an appointment
Emelyanenko Mikhail Vladimirovich
Cardiovascular surgeon, arrhythmologist, doctor of the highest category
Make an appointment
Tishchenko Ivan Sergeevich
Cardiovascular surgeon, candidate of medical sciences, doctor of the highest category
16 years of experience
Make an appointment
Bylov Konstantin Viktorovich
Cardiovascular surgeon
23 years of experience
Make an appointment
Search for the cause of the disturbance in the functioning of the cardiovascular system
- Vascular examination If the cause of heart muscle suffering is atherosclerosis, we will offer you to conduct an ultrasound examination (ultrasound) of the vessels of the brain and neck, ultrasound examination of the vessels of the arms and legs because with atherosclerotic damage to the vessels of the heart, there is a high probability that some other vessels are involved in the process.
- Biochemical blood test (lipid profile study, i.e. the ratio of harmful and good cholesterol);
- Immunological and microbiological studies (bacteriological cultures, PCR, determination of antibodies to infections). These studies may be useful for selecting targeted treatments for carditis.
- An immunogram can be useful to find the reason why the causative agent of carditis was able to enter the body. Typically, the immune system prevents any foreign agent (bacteria, virus, etc.) from entering the body. Our task is to find the dysfunctional link in the immune system and prevent the development of carditis in the future.
When there is an imbalance in various forms of cholesterol, atherosclerosis develops.
Atherosclerotic cholesterol plaques block the lumen of blood vessels, impair blood circulation, and can cause myocardial infarction and heart pain. We recommend regular heart examinations, namely bicycle ergometry, Echo-CG (ultrasound of the heart), ABPM and others. This will help identify problems with the cardiovascular system before obvious symptoms appear. Bicycle ergometry is an indispensable study to check how the myocardium (heart muscle reacts) to physical activity or stress; ultrasound of the heart shows the contractility of the myocardium. Daily blood pressure monitoring (ABPM) will help identify trends in blood pressure changes and help in identifying factors that contribute to a rise in blood pressure.
Reviews of doctors providing the service - cardiac probing
I had surgery on 2 legs with Yuri Stanislavovich Malakhov.
I want to express my deep gratitude to him for a new breath of life, lightness on my feet, one might say, a completely different standard of living. Yuri Stanislavovich, you have golden hands and you are a doctor from God! I recommend it to everyone, women and men - don’t be afraid and... Read full review Irina Nikolaevna G
11.06.2021
I would like to sincerely thank the surgeon-phlebologist Yuri Stanislavovich Malakhov for the high-quality treatment of varicose veins using a modern method: no incision, no hospitalization, high cosmetic effect. The very next day I went to work. Yuri Stanislavovich is a professional... Read full review
Natalia Viktorovna F
18.04.2021
After the procedure
After the procedure, the doctor removes the catheters, sheath and guidewire. A pressure bandage is applied to the site where the catheter was inserted to stop bleeding. Pressure can be maintained manually, using a sandbag or other device. The patient is transferred to the recovery room, where he will need to lie down for 2-3 hours. Heart rate and blood pressure will be monitored by bedside monitors.
Depending on your initial health status and what additional procedures were done during the cardiac catheterization, the patient may have to spend the night in the hospital. It is important to strictly follow your doctor's instructions about what medications to take and when to resume activity.
Most people can return to their normal activities the day after the procedure, depending on whether any additional interventions were performed during cardiac surgery.
There may be a slight bruise at the puncture site - this is normal.