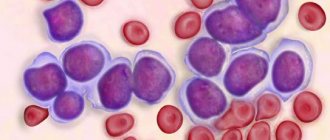
Acute leukemia is a severe pathology of the hematopoietic system, in which a large number of blast (immature) leukocytes appear in the blood. A malignant mutation of a stem cell in the bone marrow leads to the development of a tumor. The modified hematopoietic organ produces blast cells, which over time increasingly displace normal cells. The patient's immunity decreases, resulting in inflammatory processes, infections, bleeding, and the patient's condition quickly deteriorates. Acute blood leukemia never enters the chronic phase. The disease is characterized by a rapid progression and high aggressiveness of malignant cells.
Kinds
According to the generally accepted classification, acute leukemia is divided into lymphoblastic, non-lymphoblastic and undifferentiated, depending on the type of pathologically altered cells.
Lymphoblastic:
- B-cell pre-forms;
- mature B-cell leukemia;
- T-cell pre-forms;
- cortical T cell form;
- mature T-cell leukemia.
These forms most often develop in children and older people. Among childhood cancers, acute leukemia ranks first in frequency.
Non-lymphoblastic acute leukemias:
- myeloblastic;
- myelomonoblastic and monoblastic;
- megakaryoblastic;
- erythroblastic.
Nonlymphoblastic acute leukemias
Non-lymphoblastic acute leukemia - these types of leukemia arise as a result of a mutation in one of the myeloid progenitor cells. They predominate among adult leukemias. In the group of acute myeloid leukemia, the following forms of the disease are distinguished: MO-acute myeloid leukemia, in which blast cells have minimal signs of differentiation; M1-2—acute myeloblastic leukemia with the presence of cells of varying degrees of maturity; MZ—acute promyelocytic leukemia; M4 - acute myelomonoblastic leukemia; M5—acute monoblastic leukemia; M6—acute erythroleukemia; M7 - acute megakaryoblastic leukemia.
Acute myeloblastic (AML) and myelomonoblastic leukemia (AMML) are the most common : among non-lymphoblastic acute leukemias of adults, these forms account for approx. 80%. Age-related peaks of acute myeloblastic and myelomonoblastic leukemia are observed at the age of up to 1-2 years, then at 38 years (AML) and at 50 years (AML). Clinic : characterized by an acute onset of the disease with high fever, necrosis in the throat (with deep primary granulocytopenia); often there are bone pains, anemia, and hemorrhagic phenomena, which are caused not only by thrombocytopenia, but also by disseminated intravascular coagulation syndrome. Bleeding of the mucous membranes (gingival, nasal, uterine, intestinal bleeding), petechial rash on the skin, primarily the legs, is observed; hematuria is observed less often, and even less often, hemorrhage in the brain. Hemorrhagic syndrome is often the earliest manifestation of acute nonlymphoblastic leukemia. The enlargement of the spleen in acute myeloblastic and myelomonoblastic leukemia is moderate. Ulcerative-necrotic lesions of the mucous membranes of the oral cavity (stomatitis, hyperplastic gingivitis with bleeding), pharynx (angina) and intestines are very characteristic - necrotic enteropathy, paraproctitis, etc., which is explained by a decrease in the level of blood granulocytes. Initial symptoms of necrotic enteropathy: splashing and rumbling upon palpation of the ileocecal area, pasty stools, slight bloating, high fever. Prognosis: the average frequency of first remissions in acute myeloblastic and myelomonoblastic leukemia with modern therapy reaches 60%. The duration of the first remission exceeds 2 years. Oncological recovery is observed in 10% of patients of all ages.
Symptoms
In all types of acute leukemia, the symptoms are almost the same and at the initial stage are rather mild. There are no specific signs; the disease can unfold gradually or, on the contrary, suddenly and violently. The most typical manifestations are:
- increased temperature, fever;
- increased sweating, especially at night;
- sudden loss of strength, drowsiness;
- pale skin;
- increased size of lymph nodes, liver, spleen;
- poorly healing wounds and abrasions on the skin and mucous membranes;
- easily formed bruises, hematomas, bleeding;
- extensive bruising on the skin;
- frequent infections and inflammations.
At the initial stage, the disease can easily be mistaken for the flu or a cold. If the discomfort does not stop for two or more weeks, you should definitely visit an oncologist.
Clinical symptoms
Acute leukemia can be asymptomatic or have a fairly acute onset. It all starts with intoxication syndrome due to increased breakdown of leukemia cells. Manifested by weight loss, loss of strength, general weakness, drowsiness, decreased appetite, nausea, vomiting, headache, high temperature (neoplastic fever), sweating (especially at night). In general, the picture of the disease has certain syndromes, including:
Immunodeficiency (caused by a sharp violation of cellular and humoral immunity due to the functional inferiority of leukocytes). It can manifest itself as sore throat, pneumonia and the presence of other infections (bacterial, viral, fungal).
Hyperplastic is caused by leukemic tissue infiltration and is represented by enlarged lymph nodes, tonsils, liver and spleen (hepatolienal syndrome).
Hemorrhagic (as a result of a decrease in the number of platelets, increased vascular permeability and impaired coagulation). It can manifest itself as subcutaneous hemorrhages and nasal, gastric, intestinal, renal, and pulmonary bleeding.
Anemic syndrome (caused by a decrease in the number of red hematopoietic cells). Presented with weakness, dizziness, tinnitus, darkening of the eyes, pale skin, tachycardia.
There are also secondary symptoms and syndromes that are not observed in all groups of patients, including:
- Osteoarticular - pain in bones and joints.
- Ulcerative-necrotic - stomatitis, gingivitis, tonsillitis.
- Damage to the genitourinary system - enlargement and hardening of the testicles or ovaries, urination disorders, possible hematuria, uterine bleeding.
- Damage to the digestive organs - dysphagia and obstruction of the esophagus, signs of gastric ulcer, necrotizing enterocolitis.
- Kidney damage - proteinuria, microhematuria, leukocyturia, signs of acute renal failure.
- Lung damage - cough, hemoptysis, shortness of breath, fine wheezing, signs of respiratory failure.
- Heart damage - signs of myocarditis, exudative pericarditis, arrhythmia.
- Skin damage - the appearance of leukemia - dense infiltrates (nodes) of different colors, which are often accompanied by itching.
https://repo.knmu.edu.ua/handle/123456789/3190
Causes and risk factors
The only reason for the development of acute leukemia is a malignant change in the gene of a bone marrow stem cell, which triggers the hematopoietic process. Uncontrolled proliferation of mutated tumor cells leads to disruption of hematopoiesis and gradual displacement of healthy cells by malignant ones. Among the factors that have a negative impact on the bone marrow and hematopoietic system, the most significant are:
- high doses of radioactive radiation;
- some types of chemical compounds;
- T-lymphotropic viruses;
- tobacco smoking, other air pollution;
- inherited predisposition to cancer pathologies;
- immunodeficiency states.
These factors are characterized by insufficient activity of the immune system, which does not have time to recognize and destroy malignant cells immediately after their appearance.
List of sources
- Savchenko V.G., Parovichnikova E.N. Acute leukemia//Clinical oncohematology: a guide for doctors. Ed. Volkova M.A.. 2nd ed., revised. and additional 2007
- Blindar, Valentina Nikolaevna Algorithm for laboratory diagnosis of acute leukemia. Guide for doctors / Blindar Valentina Nikolaevna. — M.: Medical Information Agency (MIA), 2013
- Gavrilov, O.K. Bone marrow and peripheral blood cells / O.K. Gavrilov, G.I. Kozinets, N.B. Chernyak. — M.: Medicine, 2014
- Davidenkova, E.F. Clinic and genetics of leukemia / E.F. Davidenkova, S.I. Sherman, N.N. Kolosova. — M.: Medicine, 2010
Stages
The classification of acute leukemia divides the course of the disease into three stages:
- initial, with mild nonspecific symptoms;
- expanded, consisting of the phases of debut (attack), remission and relapse or recovery;
- terminal, during which healthy cells practically cease to be produced by the hematopoietic system, which leads to a sharp deterioration in the patient’s condition.
The disease is detected during the debut of the advanced stage of acute leukemia, when the bone marrow begins to actively produce blast cells. The active efforts of oncologists and hematologists lead to a reduction in their amount in the patient’s blood to 5% or lower. If this condition persists for five years, then the remission is considered complete and the patient is cured. With incomplete remission, the number of blast cells in the blood after some time again increases to more than 5%.
Circulatory and lymphatic systems
To understand the different types of leukemia, it is helpful to have basic information about the circulatory and lymphatic systems.
Bone marrow is the soft, spongy, inner part of bones. All blood cells are produced in the bone marrow. In infants, bone marrow is found in almost all the bones of the body. By adolescence, bone marrow is stored mainly in the flat bones of the skull, shoulder blades, ribs, and pelvis.
Bone marrow contains blood-forming cells, fat cells, and tissues that help blood cells grow. Early (primitive) blood cells are called stem cells. These stem cells grow (mature) in a specific order and produce red blood cells (erythrocytes), white blood cells (white blood cells) and platelets.
Red blood cells carry oxygen from the lungs to other tissues of the body. They also remove carbon dioxide, a waste product of cellular activity. A decrease in the number of red blood cells (anemia, anemia) causes weakness, shortness of breath and increased fatigue.
White blood cells help protect the body from germs, bacteria and viruses. There are three main types of leukocytes: granulocytes, monocytes and lymphocytes. Each type plays a special role in protecting the body against infection.
Platelets prevent bleeding from cuts and bruises.
The lymphatic system consists of lymphatic vessels, lymph nodes and lymph.
Lymphatic vessels resemble veins, but they do not carry blood, but a clear liquid - lymph. Lymph consists of excess tissue fluid, waste products and immune system cells
Lymph nodes (sometimes called lymph glands) are bean-shaped organs located along the lymphatic vessels. Lymph nodes contain cells of the immune system. They can increase in size more often during inflammation, especially in children, but sometimes their increase can be a sign of leukemia, when the tumor process has spread beyond the bone marrow.
Top
Diagnostics
Laboratory tests are required to make a diagnosis and determine the type of disease.
- General blood test with leukocyte count for the primary diagnosis of pathology.
- Biochemical blood test to detect deterioration in liver and kidney function.
- A bone marrow biopsy for later examination (usually taken from the ilium).
- Histological examination of the biopsy specimen. Necessary for identifying malignant cells.
- Cytochemical analysis of biopsy specimen. Specific enzymes characteristic of certain blasts are determined.
- Immunophenotypic analysis. Determination of surface antigens makes it possible to accurately determine the type of acute leukemia.
- Cytogenetic analysis. Detects chromosome damage, which allows you to accurately determine the type of disease.
- Molecular genetic analysis. It is carried out in cases where other methods do not give a clear result.
- Ultrasound of the peritoneal organs. Confirmation of an increase in the size of the liver and spleen, identification of metastases in the lymph nodes and other internal organs.
- Chest X-ray. Detection of enlarged lymph nodes and inflammation in the lungs.
In the future, other diagnostic studies may be needed to clarify the diagnosis and to monitor changes in the patient’s condition.
Attention!
You can receive free medical care at JSC “Medicine” (clinic of Academician Roitberg) under the program of State guarantees of compulsory medical insurance (Compulsory health insurance) and high-tech medical care.
To find out more, please call +7, or you can read more details here...
Treatment
Currently, there are many ways to treat acute leukemia.
- Chemotherapy is the main method, which involves the use of specific medications that destroy malignant cells. As a rule, oncologists-chemotherapists use multicomponent regimens, selecting drugs depending on the type of leukemia cells and the individual characteristics of the body. The treatment regimen consists of four main stages: induction - the main impact, consolidation - consolidation of the result, reinduction - repeated induction to destroy “dormant” leukemic foci, and as the final stage - maintenance therapy with low doses of cytostatics.
- Transfusion therapy is used as an auxiliary therapy to improve the tolerability of chemotherapy drugs. To correct anemic syndrome, the patient is administered red blood cells or platelets, various isotonic solutions, etc.
- Antibiotic therapy is given when infections occur.
- Radiation therapy is usually given before a bone marrow transplant to maximize the destruction of leukemia cells.
- Bone marrow transplantation is carried out after high-dose polychemotherapy, which is often combined with irradiation of the hematopoietic centers. Autotransplantation of healthy hematopoietic stem cells is possible, which are taken from the patient before starting chemotherapy and stored until the end of the course. If it is no longer possible to remove your own healthy cells, they are taken from a donor, but there is a fairly high risk of transplant rejection: the transplanted immune cells begin to attack the body of the new host, which is foreign to them.
- Palliative care is most often used for elderly patients who cannot tolerate severe treatment. Its goal is not recovery, but to inhibit tumor growth and reduce the rate of production of pathological leukocytes. For this purpose, low doses of chemotherapy, radiation therapy, targeted and immunostimulating drugs are prescribed.
In the list of clinical recommendations for acute leukemia, the most important place is the exclusion of any infections during treatment. Before starting the course, the patient must get rid of carious teeth, treat respiratory tract infections, etc. During treatment, he is in a hospital, where a strict aseptic regime is maintained to exclude accidental infection.
Publications in the media
Acute leukemia is a malignant disease of the hematopoietic system; morphological substrate - blast cells. Frequency. 13.2 cases per 100,000 population among men and 7.7 cases per 100,000 population among women.
CLASSIFICATION FAB classification (Franco-American-British) is based on the morphology of leukemic cells (structure of the nucleus, ratio of the sizes of the nucleus and cytoplasm) • Acute myeloblastic (non-lymphoblastic) leukemia (AML) •• M0 - without cell maturation, myelogenous differentiation is proven only immunologically •• M1 - without cell maturation •• M2 - AML with cell differentiation, •• M3 - promyelocytic •• M4 - myelomonocytic •• M5 - monoblastic leukemia •• M6 - erythroleukemia •• M7 - megakaryoblastic leukemia • Acute lymphoblastic leukemia (ALL): •• L1 - without cell differentiation (morphologically homogeneous cells) •• L2 - with cell differentiation (morphologically heterogeneous population of cells) •• L3 - Burkett-like leukemias • Undifferentiated leukemia - this category includes leukemias whose cells cannot be identified as myeloblastic or lymphoblastic (neither chemical, neither by immunological methods) • Myelopoietic dysplasia •• Refractory anemia without blastosis (in the bone marrow blasts and promyelocytes <10%) •• Refractory anemia with blastosis (in the bone marrow blasts and promyelocytes 10 30%) •• Refractory anemia with an excess of blasts in transformation •• Chronic myelomonocytic leukemia.
REAL classification (Revised European American classification of Lymphoid neoplasms), revised (European American) classification of lymphoid hemoblastoses • Pre B cell tumors •• Pre B lymphoblastic leukemia/lymphoma • Pre T cell tumors •• Pre T lymphoblastic leukemia/lymphoma • Peripheral B tumors cells •• chronic lymphocytic leukemia/small lymphocyte lymphoma •• Lymphoplasmocytic lymphoma •• Mantle cell lymphoma •• Follicular lymphoma •• Marginal zone cell lymphoma •• Hairy cell leukemia •• Plasmacytoma/plasmocytic myeloma •• Diffuse lymphoma of large lymphocytes• • Burkett's lymphoma • Tumors of peripheral T cells and NK cells •• T cell chronic lymphocytic leukemia •• Leukemia of large granular lymphocytes •• Mycosis fungoides and Sezary syndrome T cell lymphoma •• Angioimmunoblastic T cell lymphoma •• Angiocentric lymphoma (lymphoma of NK and T cells) •• Intestinal T cell lymphoma •• Leukemia/adult T cell lymphoma •• Anaplastic large cell lymphoma
Variants of AML (WHO classification, 1999) • AML with t(8;21)(q22;q22) • AML with t(15;17) (q22;q11 12) • Acute myelomonoblastic leukemia • AML with pathological bone marrow eosinophilia (inv( 16)(p13q22) or t(16;16) (p13;q11) • AML with 11q23 (MLL) defects • Acute erythroid leukemia • Acute megakaryocytic leukemia • Acute basophilic leukemia • Acute panmyelosis with myelofibrosis • Acute biphenotypic leukemia • AML with multilineage dysplasia • Secondary AML.
Immunohistochemical study (determination of cellular phenotype) is necessary to clarify the immunological variant of leukemia, which affects the treatment regimen and clinical prognosis
• Acute lymphoblastic leukemia (247640, , mutation of somatic cells) - 85% of all cases, accounts for up to 90% of all childhood leukemias. It develops quite rarely in adults. Cytochemical reactions: positive for terminal deoxynucleotidyl transferase; negative for myeloperoxidosis, glycogen. The use of cell membrane markers made it possible to identify subtypes •• B-cell - 75% of all cases •• With the absence of rosette formation •• T-cell •• Other variants (rare). Differential diagnosis of subtypes is important for prognosis, because T-cell variants are difficult to treat.
• Acute myeloid leukemia occurs more often in adults, the subtype depends on the level of cell differentiation. In most cases, the myeloblast clone originates from hematopoietic stem cells capable of multiple differentiation into colony-forming units of granulocytes, erythrocytes, macrophages or megakaryocytes, therefore, in most patients, malignant clones do not show signs of lymphoid or erythroid lineages •• AML is most often observed; has four variants (M0 - M3) •• M0 and M1 - acute leukemia without cell differentiation •• M2 - acute with cell differentiation •• M3 - promyelocytic leukemia, characterized by the presence of abnormal promyelocytes with giant granules; often combined with DIC caused by the thromboplastic effect of granules, which casts doubt on the advisability of using heparin in therapy. The prognosis for M3 is less favorable than for M0–M1 •• Myelomonoblastic and monoblastic leukemia (M4 and M5, respectively) are characterized by a predominance of non-erythroid cells such as monoblasts. M4 and M5 account for 5–10% of all AML cases. A common symptom is the formation of extramarrow foci of hematopoiesis in the liver, spleen, gums and skin, hyperleukocytosis exceeding 50–100109/l. Sensitivity to therapy and survival are lower than with other types of acute myeloblastic leukemia •• Erythroleukemia (M6). A variant of acute myeloblastic leukemia, accompanied by increased proliferation of erythroid precursors; characterized by the presence of abnormal blast nucleated red blood cells. The effectiveness of treatment for erythroleukemia is similar to the results of treatment for other subtypes or slightly lower • Megakaryoblastic leukemia (M7) is a rare variant combined with bone marrow fibrosis (acute myelosclerosis). Doesn't respond well to therapy. The prognosis is unfavorable. Pathogenesis is caused by the proliferation of tumor cells in the bone marrow and their metastasis to various organs. Inhibition of normal hematopoiesis is associated with two main factors: • damage and displacement of the normal hematopoietic germ by poorly differentiated leukemic cells • production of inhibitors by blast cells that suppress the growth of normal hematopoietic cells.
Stages of acute leukemia • Primary active phase • Remission (with treatment) - complete clinical and hematological •• The content of blasts in the bone marrow is less than 5% with normal cellularity •• There is no proliferative syndrome in the clinical picture • Relapse (early and late) •• Isolated bone marrow - the content of blasts in the bone marrow is more than 25% •• Extramarrow ••• Neuroleukemia (neurological symptoms, cytosis of more than 10 cells, blasts in the cerebrospinal fluid) ••• Testicular (increase in the size of one or two testicles, the presence of blasts is confirmed by cytological and histological studies) •• Mixed • Terminal phase (in the absence of treatment and resistance to therapy)
The clinical picture of acute leukemia is determined by the degree of infiltration of the bone marrow by blast cells and inhibition of hematopoietic sprouts • Inhibition of bone marrow hematopoiesis •• Anemic syndrome (myelophthisis anemia) •• Hemorrhagic syndrome (due to thrombocytopenia, skin hemorrhages are noted - petechiae, ecchymoses; bleeding from the mucous membranes - nosebleeds, internal bleeding) •• Infections (leukocyte dysfunction) • Lymphoproliferative syndrome •• Hepatosplenomegaly •• Enlarged lymph nodes • Hyperplastic syndrome •• Bone pain •• Lesions of the skin (leukemids), meninges (neuroleukemia) and internal organs • Intoxication syndrome • • Weight loss •• Fever •• Hyperhidrosis •• Severe weakness.
The diagnosis of acute leukemia is confirmed by the presence of blasts in the bone marrow. To identify the subtype of leukemia, histochemical, immunological and cytogenetic research methods are used.
Laboratory tests • In peripheral blood, the level of leukocytes can vary from severe leukopenia (below 2.0109/l) to hyperleukocytosis; anemia, thrombocytopenia; the presence of blast cells up to total blastosis • Hyperuricemia due to the accelerated life cycle of cells • Hypofibrinogenemia and increased content of fibrin destruction products due to concomitant DIC. The influence of drugs. GCs should not be prescribed until a definitive diagnosis has been made. High sensitivity of blast cells to prednisolone leads to their destruction and transformation, making diagnosis difficult. Treatment is complex; the goal is to achieve complete remission. Currently, hematology centers use various chemotherapy protocols based on the principles of polychemotherapy and intensification of treatment.
• Chemotherapy consists of several stages •• Induction of remission ••• For ALL - one of the schemes: a combination of vincristine intravenously weekly, prednisolone orally daily, daunorubicin and asparaginase for 1-2 months continuously ••• For AML - a combination of cytarabine in /drip or subcutaneous injection, daunorubicin intravenously, sometimes in combination with thioguanine. More intensive post-induction chemotherapy, which destroys remaining leukemia cells, increases the duration of remission •• Consolidation of remission: continuation of systemic chemotherapy and prevention of neuroleukemia in ALL (endolumbar methotrexate in ALL combined with radiation therapy to the brain with involvement of the spinal cord [C1-C2]) •• Maintenance therapy: periodic courses of remission reinduction.
• AML M3 is treated with retinoic acid (tretinoin). • Bone marrow transplantation is the method of choice for acute myeloblastic leukemia and for relapses of all acute leukemia. The main condition for transplantation is complete clinical and hematological remission (the content of blasts in the bone marrow is less than 5%, the absence of absolute lymphocytosis). Before surgery, chemotherapy can be administered in ultra-high doses, alone or in combination with radiation therapy (to completely destroy leukemia cells) •• The optimal donor is an identical twin or sibling; Donors with a 35% Ag HLA match are more often used. In the absence of compatible donors, autotransplantation of bone marrow taken during remission is used •• The main complication is graft-versus-host disease. It develops as a result of transplantation of donor T-lymphocytes, which recognize the recipient's Ags as foreign and cause an immune reaction against them. An acute reaction develops within 20–100 days after transplantation, a delayed reaction occurs after 6–12 months ••• The main target organs are the skin (dermatitis), gastrointestinal tract (diarrhea) and liver (toxic hepatitis) ••• Treatment is long-term, usually limited prescribing combinations of prednisolone, cyclosporine and small doses of azathioprine •• The course of the post-transplantation period is also influenced by preparatory treatment regimens, the development of interstitial pneumonia, and graft rejection (rarely).
• Replacement therapy •• Transfusion of red blood cells to maintain the Hb level not lower than 100 g/l. Transfusion conditions: unrelated donor, use of leukocyte filters •• Transfusion of fresh platelets (reduces the risk of bleeding). Indications: platelet count less than 20109/l; hemorrhagic syndrome with platelet content less than 50109/l.
• Prevention of infections is the main condition for the survival of patients with neutropenia resulting from chemotherapy •• Complete isolation of the patient •• Strict sanitary and disinfection regime - frequent wet cleaning (up to 4-5 times a day), ventilation and quartzing of rooms; use of disposable instruments, sterile clothing for medical personnel •• Prophylactic use of antibiotics, antifungal and antiviral drugs (if the content of segmented neutrophils is less than 0.5109/l, prevention of Pneumocystis pneumonia is indicated) ••• If the body temperature increases, clinical and bacteriological studies are carried out and immediately begin treatment with combinations of broad-spectrum bactericidal antibiotics: cephalosporins, aminoglycosides and semi-synthetic penicillins ••• For secondary increases in body temperature that occur after treatment with broad-spectrum antibiotics, antifungal agents (amphotericin B) are empirically used •• Colony-stimulating agents can be prescribed for the prevention and treatment of neutropenia factors (for example, molgramity).
Prognosis • The prognosis for children with acute lymphocytic leukemia is good: 95% or more experience complete remission. 70–80% of patients have no manifestations of the disease for 5 years and are considered cured. If a relapse occurs, in most cases a second complete remission can be achieved. Patients in second remission are candidates for bone marrow transplantation with a long-term survival rate of 35–65% • The prognosis for patients with acute myeloid leukemia is poor. 75% of patients receiving adequate treatment using modern chemotherapy regimens achieve complete remission, 25% of patients die (remission duration is 12–18 months). There are reports of cure in 20% of cases with continued intensive therapy after remission. The prognosis for the M3 variant of AML improves with treatment with retinoic acid drugs. Patients under 30 years of age can undergo bone marrow transplantation after achieving the first complete remission. 50% of young patients who have undergone allogeneic transplantation develop long-term remission. Encouraging results have also been obtained with autologous bone marrow transplants.
Age characteristics • Children •• 80% of all acute leukemias are ALL •• Adverse prognostic factors for ALL ••• Age of the child under 1 year and over 10 years ••• Male gender ••• T-cell variant of ALL ••• Leukocyte content at the time of diagnosis more than 20109/l ••• Lack of clinical and hematological remission against the background of induction •• Prognosis and course. 80% of clinical and hematological remission. 5-year survival rate is 40–50%.
• Elderly . Reduced tolerance to allogeneic bone marrow. The maximum age for transplantation is 50 years. Autologous transplantation can be performed in patients over 50 years of age in the absence of organ damage and general somatic well-being.
Abbreviations • MDS - myelodysplastic syndrome • ALL - acute lymphoblastic leukemia • AML - acute myeloid leukemia.
ICD-10 • C91.0 Acute lymphoblastic leukemia • C92 Myeloid leukemia [myeloid leukemia] •• C93.0 Acute monocytic leukemia
Forecasts
A few decades ago, being diagnosed with acute leukemia was essentially a death sentence. Currently, the situation has improved significantly; the use of new, effective drugs makes it possible to achieve a cure for more than half of the patients. With timely treatment, complete remission occurs in 45-80% of patients. The best indicators are in children under 10 years of age, among whom up to 86% of patients recover completely, the worst are in older people, whose five-year survival rate does not exceed 30%.
Consequences (remission and relapse)
Just a few decades ago, acute leukemia led to the death of the patient within 2-3 months after diagnosis. Today, the situation has changed dramatically thanks to the emergence of new drugs for treatment.
At the moment, the clinic of acute leukemia distinguishes the following stages:
- The first attack - during this period, tumor cells actively multiply in the bone marrow and enter the blood. It is at this stage that the diagnosis is made. Symptoms of the disease will be determined by which hematopoietic germ is affected. As a rule, these are persistent infections, anemia, general weakness, enlarged lymph nodes, etc.
- Remission period. If acute leukemia has responded to chemotherapy, the tumor cells are destroyed and hematopoiesis is restored. The number of blasts in the bone marrow returns to normal and does not exceed 5% of the total number of cells. There are several types of remission, depending on how completely the tumor clone is suppressed. Currently, the goal of treatment is to achieve complete remission within 5 years. After this period, the patient is considered completely healthy.
- Relapse. Some patients experience a relapse, in which the number of blasts increases again. They again enter the bloodstream and can form extramarrow foci of infiltration. There may be several relapses, and each time it becomes more and more difficult to put them into remission. However, many patients achieve a complete five-year remission, even after several relapses.
- Terminal stage. They talk about it when all the used methods for treating acute leukemia lose their effectiveness and it is no longer possible to restrain tumor growth. The body's hematopoietic system is completely suppressed.
Rehabilitation
Recovery after severe chemotherapy is aimed at reducing the risk of complications of acute leukemia, and primarily at restoring the functions of the immune system with the help of:
- general strengthening treatment - vitamin complexes, iron supplements, immunomodulators;
- restoration of intestinal microflora with the help of probiotics;
- detoxification procedures;
- improve sleep, strengthen the nervous system;
- psychotherapy.
Diagnosis and treatment of acute leukemia in Moscow
If you have symptoms of acute leukemia, contact the Medicina clinic. We offer our patients;
- accurate and fast diagnostics using the most modern equipment;
- treatment by highly qualified specialists - oncologists, hematologists, chemotherapists;
- stay in a comfortable, excellently equipped hospital;
- world-class medical service.
Call us to schedule an initial consultation with one of the best oncologists in Moscow.
Questions and answers
How long do people live with acute blood leukemia?
If left untreated, death occurs within 1-2 years after acute leukemia is diagnosed. Modern methods and effective drugs make it possible to achieve complete remission in 80% of patients, depending on their age, current condition, stage of the process and other factors. More than half of patients live more than 10 years after treatment.
How does leukemia manifest?
The external manifestations of the disease at the initial stage resemble the symptoms of a common cold, so they are often ignored. If the elevated temperature does not decrease within two weeks, weakness, malaise, sweating and other “cold” sensations do not go away, you must contact an oncologist for examination as soon as possible.
Can acute leukemia be cured?
In case of acute leukemia, timely initiation of treatment greatly increases the patient’s chances of recovery. Therefore, if you notice any disturbing signs, you should visit an oncologist, because they may turn out to be symptoms of a serious and dangerous, rapidly developing disease. In this case, you cannot waste time, because every day reduces the chances of treatment success.
Attention! You can cure this disease for free and receive medical care at JSC "Medicine" (clinic of Academician Roitberg) under the State Guarantees program of Compulsory Medical Insurance (Compulsory Medical Insurance) and High-Tech Medical Care. To find out more, please call +7(495) 775-73-60, or on the VMP page for compulsory medical insurance
What causes acute leukemia and can it be prevented?
A risk factor is something that increases the likelihood of disease. Some risk factors, such as smoking, can be eliminated. Other factors, such as age, cannot be changed.
Smoking is a proven risk factor for acute myeloid leukemia (AML). Although many people know that smoking causes lung cancer, few realize that smoking can affect cells not directly exposed to smoke.
Cancer-causing substances found in tobacco smoke enter the bloodstream and spread throughout the body. One fifth of AML cases are caused by smoking. People who smoke should try to quit smoking.
There are some environmental factors that have been linked to the development of acute leukemia. For example, long-term exposure to gasoline is a risk factor for AML, and exposure to high doses of radiation (atomic bomb explosion or nuclear reactor incident) increases the risk of AML and acute lymphoblastic leukemia (ALL).
People who have had other cancers and were treated with certain anticancer drugs are at increased risk of developing AML. Most of these cases of AML occur within 9 years of treatment for Hodgkin's disease (lymphogranulomatosis), non-Hodgkin's lymphoma (lymphosarcoma), ALL, or other malignancies such as breast and ovarian cancer.
There is some concern regarding high-voltage transmission lines as a risk factor for leukemia. According to some data, in these situations the risk of leukemia is not increased or increased slightly. What is clear is that most cases of leukemia are not associated with high-voltage transmission lines.
A small number of people with very rare diseases or the HTLV-1 virus have an increased risk of developing acute leukemia.
However, most people with leukemia have no identified risk factors. The cause of their illness remains unknown to this day. Due to the fact that the cause of leukemia is unclear, there are no methods of prevention, with the exception of two important points: avoid smoking and contact with substances that cause cancer, such as gasoline.