When a person has a heart attack, they need to know what to do and responding quickly can help them achieve a better outcome.
A heart attack occurs when there is a blockage in blood flow to the heart, blocking the delivery of oxygen and other nutrients. This situation can damage or even kill parts of the heart tissue.
Although movies may show heart attacks to occur suddenly, many heart attacks start slowly and have many warning signs.
Definition:
A heart attack is a condition that poses a serious threat to human life and health. A heart attack, also called a myocardial infarction, can be a fatal event. According to statistics, heart attacks are the most common cause of death and disability among the population in developed countries. A heart attack occurs when a blood clot blocks blood flow in a coronary artery (the vessel that supplies blood to the heart muscle). Interrupted blood flow to the heart can lead to damage and death of the heart muscle.
Unexpected situation
Many people are interested in whether a heart attack can develop in young people, as they say, out of the blue. “Yes, indeed, at a young age, myocardial infarction most often develops without previous heart pain. But, as we said above, if you pay attention in time to developing changes that at first glance are not related to the heart, you can begin to implement preventive measures in time and prevent the development of an attack,” says Galina Lazarenko.
Prevention of flaming motor. How to influence the age of the heart Read more
Causes
A heart attack is an acute condition that is accompanied by a sudden restriction of blood supply to the heart muscle. This happens with a disease associated with insufficient blood flow in the coronary vessels - coronary heart disease. The root cause is neoplasms and infections that lead to changes in the vascular walls. In most cases, heart attacks are caused by atherosclerosis of the heart vessels. This chronic disease affects large-caliber vessels: cholesterol deposits accumulate on their walls, which over time form dense plaques. They impede blood flow, causing oxygen deficiency in organ tissues. In addition, separated fragments of atheromatous plaque cause occlusion or stenosis. Atherosclerosis leads to the development of threatening conditions: acute coronary syndrome, heart attacks, strokes. Read more about the causes of a heart attack in the following publication.
Symptoms of myocardial infarction at different stages of the disease
Signs of myocardial infarction differ at different stages of pathology development. During the disease there are 4 stages:
- stage of ischemia or acute period;
- stage of necrosis (acute period);
- stage of organization or subacute period;
- post-infarction period (scarring stage).
About 40% of all recorded heart attacks come as a surprise to the patient. Most often, doctors explain these by people’s inattention to their health. In the remaining 60% of cases, the disease is preceded for a long time by angina attacks.
The first signal to show concern is the appearance of pain in the chest, back, left shoulder or forearm, sometimes radiating to the jaw, ear and, less often, to the stomach and lower back. The nature of the pain varies: from mild and sluggish to acute and cutting. Typically, such pain appears after playing sports or during everyday physical activity, during emotional experiences and stress. These are the first signs of coronary heart disease. In nine out of ten cases, IHD develops due to vascular atherosclerosis (deposits of cholesterol in the inner walls of blood vessels) that supply blood to the heart muscle.
Such attacks can be observed in a patient from several weeks to two, three or more years and often, if not intervened, end in myocardial infarction. Have you noticed these in yours? Contact specialists immediately! Timely measures taken, diagnosis and observation by doctors will help avoid the development of the disease.
If coronary heart disease is not treated, then the next stage may be the most acute period of a heart attack.
How to recognize a heart attack?
People put off seeing a doctor because they confuse the symptoms of a heart attack with non-serious illnesses (such as digestive problems). They try to tolerate their symptoms and end up getting medical help too late. Treatment of myocardial infarction has changed dramatically in recent years. It is important to recognize the symptoms immediately and see a doctor if you suspect you are having a myocardial infarction.
Seek help immediately if pain in the heart and chest (angina attack) lasts more than 10 minutes and does not go away either at rest or after taking nitroglycerin. Pain (or obvious discomfort) may move to the shoulder, shoulder blades, neck or jaw. In such a situation, the patient is taken to a specialized cardiology clinic, where there is everything necessary to conduct a full examination and provide emergency care. Emergency cardiology specializes in such conditions.
What to do
A heart attack requires emergency medical attention. If someone has a heart attack, they should immediately call 112 for emergency help before doing anything else. Act quickly - it could help save someone's life.
First aid for myocardial infarction
Myocardial infarction is a type of ischemic heart disease characterized by irreversible damage to the heart muscle as a result of deterioration of blood flow through the coronary arteries
Characteristic signs (symptoms) of a heart attack (myocardial infarction):
- • sudden (paroxysmal) pressing, squeezing, burning, aching pain in the chest (behind the sternum) lasting more than 5 minutes;
- • similar pains are often observed in the left shoulder (forearm), left shoulder blade, left half of the neck and lower jaw, both shoulders, both arms, the lower part of the sternum along with the upper abdomen;
- • lack of air, shortness of breath, severe weakness, cold sweat, nausea often occur together and sometimes follow or precede discomfort/pain in the chest;
- • it is not uncommon for these manifestations of the disease to develop against the background of physical or psycho-emotional stress, but more often with some interval after them.
Uncharacteristic signs that are often confused with a heart attack:
- • stabbing, cutting, pulsating, boring, constant aching pain for many hours and not changing its intensity in the heart area or in a specific clearly defined area of the chest
Algorithm of actions in case of a heart attack
If you or someone else suddenly has the above characteristic signs of a heart attack, even with weak or moderate intensity, which last more than 5 minutes, do not hesitate, immediately call an ambulance team. Do not wait more than 10 minutes - in such a situation it is life-threatening.
If you have symptoms of a heart attack and there is no way to call an ambulance, then ask someone to take you to the hospital - this is the only right decision. Never drive yourself unless you have no other choice.
In the most optimal scenario, if a heart attack occurs, you must act according to the following algorithm:
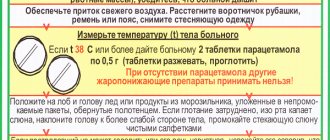
- • Immediately after an attack occurs, sit down (preferably in a chair with armrests) or lie in bed with the head of the bed raised, take 0.25 g of acetylsalicylic acid (aspirin) (chew the tablet, swallow) and 0.5 mg of nitroglycerin (spray one inhalation dose into the cavity mouth while holding your breath, place one tablet/capsule under the tongue, first bite the capsule, do not swallow); free your neck and provide fresh air (open the vents or windows).
- • If after 5-7 min. After taking acetylsalicylic acid (aspirin) and nitroglycerin, the pain persists, it is imperative to call an ambulance team and take nitroglycerin a second time.
- • If pain persists 10 minutes after taking the second dose of nitroglycerin, it is necessary to take nitroglycerin a third time.
- • Give the patient a sedative (motherwort or valerian). There should be silence in the room, not allowing the sick person to become nervous.
- • If after the first or subsequent doses of nitroglycerin there is severe weakness, sweating, shortness of breath, you need to lie down, raise your legs (on a bolster, etc.), drink 1 glass of water and then, as with a severe headache, do not take nitroglycerin.
- If a person with a heart attack is unconscious and there is someone nearby who knows how to provide first aid in this situation, then you need to do it immediately!
What to do if you see a person with a developing myocardial infarction?
If you encounter an unconscious person due to a suspected myocardial infarction, call an ambulance. If you are trained in first aid, begin cardiopulmonary resuscitation (CPR). This will help deliver oxygen to the body and brain.
Begin CPR with chest compressions. Press down on the chest about 5 cm with each compression at a rate of about 100 compressions per minute. If you are trained in CPR, check the person's airway and give breaths every 30 compressions. If you are not trained in CPR, continue to perform chest compressions only.
Action tactics
If you suspect a heart attack, you should act immediately. First of all, you need to provide rest to the patient, stop performing any exercise, take a half-sitting or half-lying position, which will make breathing easier. You also need:
open a window or provide ventilation to the room;- free your neck, throat and chest from tight clothing;
- breathe steadily, taking deep, calm breaths in and out;
- if chest pain occurs, take a nitroglycerin tablet, placing it under the tongue (not recommended for pressure below 110/70 mmHg;
- if the pain lasts for more than 7–10 minutes, or if it intensifies or worsens, call someone for help, call an ambulance;
- for arrhythmia (rapid, uneven pulse and heartbeat), washing with cold water, a compress on the face or forehead can help;
- in case of dizziness and a state close to loss of consciousness, it is necessary to raise the position of the legs, which will ensure better blood flow to the upper body;
- if vomiting or nausea occurs, do not lie down to avoid aspiration (choking) of vomit;
- While waiting for a doctor, you should not take other medications or attempt self-medication.
Emergency care algorithm
In case of a prolonged attack of angina with chest pain or atypical symptoms lasting more than 5–15 minutes, medical intervention is necessary, otherwise there is a high risk of developing the most acute stage of a heart attack.
In the event of a heart attack, an emergency medical technician or a hospital emergency department doctor urgently provides the following measures:
If the pain syndrome persists, the patient is given one dose of Nitroglycerin, in a tablet, capsule or aerosol under the tongue. The drug is contraindicated in case of a sharp drop in blood pressure, hypotension or collapse.- Another necessary remedy is Acetylsalicylic acid (Aspirin Cardio or an analogue) in a dosage of 325 - 300 mg.
- At the same time, an electrocardiogram is taken to identify signs of myocardial ischemia (insufficient blood supply) to the heart area, confirming or refuting the diagnosis of unstable angina or heart attack. And an oxygen mask is put on to prevent hypoxia.
- In case of a heart attack with severe chest pain, the patient can be given an intravenous painkiller (Analgin 2.0 - 4.0 50% solution or Promedol, Morphine in a dosage of 1.0 - 2.0 ml 1%).
- For high blood pressure, medications to lower blood pressure are indicated: Propranolol 10-30 mg per day, or Metoprolol 50 mg.
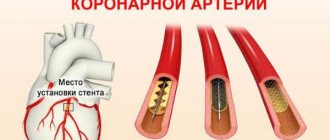
In a hospital setting, the issue of further treatment of the patient is decided. If a heart attack is confirmed and an attack is detected in the first hour, the specialist may prescribe diagnostic coronary angiography or stenting at the Cardiology Center for Vascular Surgery. These minimally invasive surgical techniques are carried out with the aim of identifying a clear area of blockage of a heart vessel, expanding it with the help of a stent to restore patency, blood flow and nutrition of the heart muscle.
In the absence of signs of a heart attack and confirmation of unstable angina, inpatient treatment is required for a period of 10–14 days and subsequent prophylaxis to prevent complications.
Complications
Complications of myocardial infarction are associated with myocardial damage. This damage leads to the following conditions:
- Heart rhythm disturbances (arrhythmias). Types of arrhythmia are bradycardia and tachycardia. As a result of damage to the heart muscle due to a heart attack, electrical instability of the myocardium develops. It manifests itself as an abnormal heart rhythm and can be serious, even fatal. In this case, the patient is advised to install a pacemaker.
- Cardiogenic shock. Another deadly condition that accompanies myocardial infarction. In severe heart attacks, the heart loses its ability to pump blood—cardiogenic shock occurs.
- Myocardial rupture. An area of the myocardium weakened by the infarction may rupture, creating a hole in part of the heart. This complication is fatal.
- Heart failure. The amount of damaged heart muscle as a result of a heart attack can be so great that the remaining part of the myocardium is not able to adequately perform its job of delivering blood to the organs and tissues of the body. Reduced blood flow to organs and tissues leads to shortness of breath, increased fatigue and swelling of the legs. Heart failure is temporary and resolves after some of the damaged myocardium (stunned myocardium) has recovered, usually within a few days or weeks. There is also a chronic condition if a large area of the myocardium is irreversibly damaged.
- Heart aneurysms. Necrotic areas of the heart muscle are replaced by connective tissue. As a result, post-infarction cardiosclerosis develops, which leads to protrusion of the heart wall - an aneurysm.
- Problems with the heart valves. If parts of the heart valve apparatus are damaged as a result of a myocardial infarction, this leads to serious or even life-threatening valvular insufficiency.
Symptoms of a heart attack in women
Experts estimate that heart disease is the No. 1 killer of American women. These diseases are also the main cause of disability in women. According to a 2004 American study, one in every four women over 65 died from a heart attack, which is about 60%, more than the death rate from all cancers combined.
Women of all ages should be concerned about heart health, although the risk increases as they get older. Also, as with any disease, in case of heart disease it is always better to carry out prevention than treatment, since two thirds of women who suffered a heart attack were unable to return to their normal lifestyle. Ideally, treatment for a heart attack should begin within one hour of the onset of symptoms. You should learn to recognize the symptoms and warning signs of an impending heart attack in women. There comes a time when women must take control of their heart health.
Heart diseases
Heart disease is described as an abnormal condition affecting the heart and the blood vessels of the heart. This could be coronary artery disease, heart failure, or cardiac arrhythmia.
Coronary artery disease (CAD) is the most common type of heart disease that causes a heart attack. Arteries thicken and narrow during CAD and blood has difficulty flowing to the heart, causing chest pain or angina and, as a result, a heart attack. Heart failure occurs when the heart cannot cope with pumping blood throughout the body. The result is shortness of breath, swollen feet, ankles and legs, and extreme fatigue. These visible symptoms suggest the onset of heart failure. Cardiac arrhythmia refers to changes in the heart cycle that can lead to dizziness, fatigue and shortness of breath, and at times chest pain.
Women's Heart Health
Women develop heart problems about seven to eight years later than men. But by age 65, women face the same risk of disease as men. What's important is that women die from heart attacks, unlike men. African, Hispanic and Latin American women should take more care of their heart health. Mainly because women of color are predisposed to obesity, lack of exercise and are therefore at high risk for high blood pressure and diabetes.
Risk factors that cannot be controlled include the following:
- Family history of early heart disease before age 60. Be extremely careful if anyone in your family has had a heart attack. If your brother or father had a heart attack before the age of 55, or your sister or mother before the age of 60, then the chances are high that you will also have a heart attack.
- 55 years of age or older
- The period after menopause or after removal of ovaries
Controlled risk factors:
- Obesity and a sedentary lifestyle are two of the most common risk factors faced by postmenopausal women. Regular exercise will help combat inactivity and obesity, which are significant risk factors for heart disease.
- Smoking: Smoking is a cause of heart attack in women under 45 years of age. Smoking and birth control pills increase the risk of the disease 20-fold.
- Hypertension, or high blood pressure, is considered a cardinal cause of many heart diseases. While a blood pressure reading below 120/80 is considered normal, high blood pressure of 140/90 or higher can cause a heart attack.
- Cholesterol: Too much low-density lipoprotein (LDL) in the blood can cause blood to clot in the artery walls, which can cause a heart attack. All women over 20 years of age are recommended to have their cholesterol and triglyceride levels checked at least once every three years. Total cholesterol levels should ideally be less than 200 mg/dL.
- Diabetes: The risk of heart disease increases 6 times in women with diabetes. Diabetes is a disease of glucose metabolism that significantly increases the risk of cardiovascular disease in women.
- Metabolic syndrome: It is common among post-menopausal women, and can be diagnosed by the presence of the following characteristics, especially obesity with a waist size greater than 35 inches, triglyceride levels greater than 150 mg/dL, HDL cholesterol less than 50 mg/dL, glucose fasting - 110 mg/dl or higher, and a hypertension value greater than or equal to 140 / 85. Exercise, diet and weight loss become mandatory for women to control the metabolic process.
- Elevated C Reactive Protein (CRP): This is a relatively new factor that is more associated with women than men. Elevated CRP levels indicate active inflammation in the blood vessels, which can lead to rupture of the coronary artery.
- Pregnancy with complications such as hypertension, diabetes or low birth weight may increase a woman's risk of premature cardiovascular disease and death.
- Recent research has shown that hypothyroidism, or low thyroid levels, already a common problem in women, may be a risk factor for heart disease.
Signs and Symptoms of Heart Disease A heart attack can happen suddenly, or it can occur in the hours, days, or even weeks before the attack. Although heart disease has no symptoms, per se, there should still be some signs. In men and women, chest or arm pain or discomfort may indicate heart disease. The pain can be sharp or moderate, it can last from several minutes and return again. Pain can also be a potential warning sign for a heart attack.
When a woman experiences angina pectoris, which means a disruption in the functioning of the coronary artery, it manifests itself in the form of hot flashes, pain when touching the back, shoulders, hands and jaw, but there is no pain in the chest. In the United States, approximately two-thirds of heart attack deaths occur in women, but these cases are not reported. In addition, shortness of breath, dizziness, nausea and abnormal heartbeats, fatigue and a feeling of tiredness are all symptoms of heart disease. If these symptoms continue, consult your doctor.
Women who have had a myocardial infarction or heart attack behave a little differently from men. They experience vomiting, indigestion, shortness of breath and fatigue, but do not complain of chest pain. Women experience myocardial infarction (MI) more silently than men, and MI without clear symptoms may be diagnosed later when subsequent cardiac symptoms appear. It has been estimated that 8 million women in the United States are currently living with heart disease and 4 million women suffer from angina.
Common signs of a heart attack in men and women:
- Discomfort and pain in one or both arms, back, neck, jaws and stomach.
- Cold sweat.
- Shortness of breath before or with chest pain.
- Feeling stomach pain or vomiting.
- Feeling tired
In addition, women express more common signs of a heart attack, which have been labeled "typical" symptoms. Here are some of them:
- Back, neck, or jaw pain
- Heartburn
- Feeling weak
- Cough
- Fluctuations in the heart or diagnosis
Tests and diagnostics
If you have had or are suspected of having a heart attack, your diagnosis is most often made by emergency physicians. You will be asked to describe your symptoms and your blood pressure, pulse and temperature will be taken. You will be connected to a monitor and will immediately begin to diagnose your myocardial infarction.
Healthcare professionals will listen to your heart and lungs with a stethoscope. You will be asked about your medical history and your family history of heart disease. A subsequent cardiac examination will help determine what is causing the pain.
Examinations include:
- Electrocardiogram (ECG). This is the first test that is performed to diagnose myocardial infarction. It is carried out while you are being asked about the symptoms of the disease. This test records the electrical activity of the heart using electrodes attached to the skin. Electrical impulses are recorded as a waveform and recorded on a monitor or paper. Since myocardium damaged by a heart attack does not conduct electrical impulses in the normal way, an ECG will show that a myocardial infarction has occurred or is progressing.
- Blood analysis. If myocardial infarction develops, the content of cardiac enzymes in the blood increases. Emergency room doctors will take blood samples from you to check for these enzymes.
Symptoms and signs of myocardial infarction in men
In men, the course of the disease has all the characteristic signs:
- sharp pain behind the sternum, in the left arm, shoulder and forearm;
- sticky cold sweat;
- weakness, dizziness, pale gray skin color;
- shortness of breath, rapid pulse;
- high blood pressure.
Despite the development of medicine, acute myocardial infarction is increasingly being diagnosed in both men and women under 40 years of age. The reason for this is a sedentary lifestyle; a diet with a predominance of unhealthy fats, which are rich in fast food products; obesity; smoking; diabetes. Young patients often have an asymptomatic form of heart attack.
Additional Research
If you have a heart attack, your cardiologist will begin immediate treatment efforts. Additional research:
- X-ray examination of the chest organs. A chest x-ray will help the doctor evaluate the size of your heart and the vascular pattern of your lungs and the presence of fluid in the pleural cavity.
- Echocardiography. This test is based on the emission and recording of reflected sound waves that create an image of the heart on a monitor. Echocardiography helps visualize the part of the myocardium that is damaged as a result of a heart attack and is not able to normally push blood through the vessels.
- Coronary angiography (catheterization of the coronary arteries). This type of coronary exam will show narrowing or blockage in the arteries that supply blood to the heart (coronary arteries). A liquid X-ray contrast agent fills the arteries supplying blood to the heart through a long, thin catheter. It is at the mouth of the coronary arteries through the femoral artery (in the groin area) or the radial artery (in the wrist area). When the arteries are filled with contrast, they become visible under X-ray guidance, revealing narrowing of the lumen and its complete blockage. In addition, since the artery is accessible, the doctor can treat coronary artery disease by performing coronary angioplasty and coronary artery stenting. During angioplasty, thin balloons are used that are delivered to the site of narrowing of the artery and inflated, expanding the lumen. In most cases, a mesh tube called a stent is then placed in this area of the artery. It keeps the artery open and prevents re-stenosis of the vessel lumen in the future.
- Stress test with load. Several days or weeks after your heart attack, you may be given a stress test. A stress test diagnoses how your heart and blood vessels respond to stress. You will walk on a treadmill or pedal a bicycle ergometer while an ECG or ECHO is recorded. If the patient is not ready for exercise, he is prescribed medications that stimulate the heart. A stress test will help your doctor determine the best treatment option. If your doctor wants to see an image of your heart during exercise, he will order a myocardial scintigraphy, a test similar to an exercise stress test that uses a special radiopharmaceutical and special imaging techniques.
- Coronary computed tomography (CT) or magnetic resonance imaging (MRI). This test is used to diagnose heart disease, including damage due to myocardial infarction. During a CT scan, you will lie on a table inside a tunnel-like machine. An X-ray machine rotates in this tunnel, recording and creating a series of images of your heart and chest organs. During this test, a radiopaque contrast agent is sometimes injected to visualize the coronary arteries. During an MRI, the patient lies on a table inside a similar tube-like machine that creates a magnetic field. The magnetic field arranges the atoms of cells in a certain way, and the device registers radio waves as a result of this rearrangement, depending on the type of tissue. These signals are processed and create an image of the heart.
Medications
- Aspirin. You will receive aspirin from emergency personnel or upon arrival at a medical facility. Aspirin reduces blood clotting and helps maintain blood flow through a narrowed vessel.
- Other antiplatelet drugs. The emergency room doctor may give you other drugs that work similar to aspirin and prevent blood clots. These are clopidogrel (Plavix), ticagrelor (Brilinta) and other drugs - platelet aggregation inhibitors.
- Thrombolytics. These drugs, also called “clot killers,” are widely used in the treatment of cardiac ischemia. They help dissolve blood clots that block blood flow in the coronary arteries. The earlier treatment with thrombolytics is started during myocardial infarction, the greater the chance of survival and the smaller the area of damaged myocardium.
- Other drugs that thin the blood. These include heparin, which makes the blood less “viscous” and less capable of dangerous blood clots. Heparin is given intravenously or subcutaneously in the first few days after myocardial infarction.
- Medicines that relieve pain. If you experience severe chest pain, you will be prescribed painkillers such as morphine. This will reduce the unpleasant symptoms of vascular diseases.
- Beta blockers. These drugs help relax the heart muscle, slow the heart rate, and lower blood pressure, making it easier for the heart to pump. Beta blockers limit damage to the heart and prevent future heart attacks.
- Nitroglycerine. The drug is used to treat angina pectoris. It temporarily widens the arteries, improving blood flow to and from the heart.
- Cholesterol-lowering drugs. These are statins, niacin, fibrates and bile acid sequestrants. They help lower levels of unwanted blood cholesterol and are useful soon after a heart attack to improve survival.
Remember the following signs and symptoms of myocardial infarction:
- The first symptom of myocardial infarction is acute, squeezing or pressing pain in the chest, radiating to adjacent organs, the left ear, jaw, left arm, and sometimes the upper abdomen. The pain can last from half an hour to a day and, unlike angina, is not relieved by taking nitroglycerin;
- patients with the first signs of a heart attack may complain of toothache;
- the painful condition is accompanied by chills, weakness and dizziness, sometimes shortness of breath and cold sweat;
- arrhythmia develops, the pulse increases noticeably;
- the skin becomes pale gray due to lack of blood supply.
The nature and severity of pain during a heart attack depend on the location of the muscle damage. The larger it is, the stronger the pain. Sometimes the only symptom of a heart attack is sudden cardiac arrest.
The acute period is one of the most dangerous stages of the disease. Some of the cardiac muscle tissue is already dead, and the heart, finding itself in unusual conditions, may not withstand the load and stop. If you feel such symptoms and make sure that the usual remedies for angina pectoris do not help, immediately call an ambulance.
Symptoms during the acute stage of myocardial infarction become less pronounced. The pain subsides. As a result of tissue necrosis, the patient's temperature rises, which, depending on the focus of necrosis, may not subside for up to 7-10 days.
In the subacute period, the signs of myocardial infarction disappear, heartbeat and body temperature normalize. A week or two after a heart attack, the dead portion of the heart muscle begins to scar.
In the post-infarction period, there are no symptoms of the disease. But angina attacks will not simply disappear, so if measures are not taken, there is a high probability of developing a recurrent myocardial infarction. To avoid this, it is necessary to treat the root causes of the pathology: coronary disease and atherosclerosis. Due to damage to blood vessels by cholesterol plaques, not only the heart suffers, but also the limbs, digestive organs and brain (cerebral infarction).
Surgical methods
In addition to drug therapy, the following procedures are offered for effective treatment of myocardial infarction:
- Coronary angioplasty and stenting;
An emergency angioplasty procedure aims to open a blocked artery, allowing blood to flow freely to the myocardium. The doctor will insert a special long, thin tube (catheter) into the blocked coronary artery through an artery in the leg in the groin area or in the arm in the wrist area. Through this catheter, a special guide and balloon are brought to the affected area of the artery.
The balloon is guided through a guidewire to the affected area of the artery and inflated, facilitating the opening of the vessel. After this, a metal stent is implanted into this section of the artery - it will maintain the artery in a straightened state for a long time. It is better to implant a stent with a drug coating, which prevents restenosis - repeated narrowing of the vessel in this area. Read more about the benefits of balloon angioplasty here.
- Coronary bypass surgery;
In difficult cases, cardiac surgeons perform emergency coronary bypass surgery during a myocardial infarction. Coronary bypass surgery involves suturing a vein or artery to a coronary artery in a place after blockage or narrowing of the latter, thus restoring blood flow through the vessel.
General Israeli statistics
Every year, statistical data obtained from cardiac centers in Israel is systematized and studied within the framework of the Israeli program for the study of myocardial infarction. Two recent large-scale studies included data on 4,000 heart attack patients. About 9% of the total were people under 45 years of age. In the professional literature, the main risk factors are smoking (about 70%) and heredity (45%). It should be emphasized that at a young age they play a much more important role than at an old age. Young patients were also prone to obesity in combination with low levels of high-density lipoprotein (HDL) in the blood.
The mortality rate from myocardial infarction in young patients during hospitalization and during the first year is clearly lower than in older patients. At the same time, re-morbidity and the need for re-hospitalization do not differ significantly in both age groups.
Early diagnosis and timely provision of medical care helps prevent the development of cardiac diseases and increase life expectancy.
Lifestyle changes and home rehabilitation
Your lifestyle affects your heart health. By following the recommendations for the prevention of coronary heart disease, you can not only prevent the development of myocardial infarction, but also improve your condition after it:
- Stop smoking. If you smoke, do one simple thing that will help your heart - stop smoking. Quitting smoking on your own can be difficult, so ask your doctor for a treatment plan. He will help you cope with a bad habit.
- Avoid secondhand smoke. Being around people who smoke is a potential trigger for heart attack because many of the chemicals in tobacco smoke damage arteries.
- Control your blood cholesterol levels. Get your cholesterol blood tested regularly and monitor it with your doctor. If your bad cholesterol levels are elevated, your doctor will prescribe dietary changes. He will prescribe medications that lower cholesterol and prevent vascular disease. How often you should test your cholesterol depends on how high your cholesterol levels are.
- Visit your doctor regularly and undergo preventive examinations. Some of the main risk factors for heart attack—high cholesterol, high blood pressure, and diabetes—do not appear in the early stages. Your doctor will perform tests to help identify these conditions. If a problem is detected, you and your doctor will begin treatment for early stages of cardiovascular disease. This will protect against the development of myocardial infarction in the future.
- Monitor your blood pressure levels.
- Exercise regularly. Regular exercise helps the heart muscle recover after a myocardial infarction. Exercise is an important part of a medical rehabilitation program after a heart attack. Physical activity helps prevent the onset of symptoms of coronary artery disease and the development of myocardial infarction. This is achieved by maintaining a healthy weight and controlling blood glucose levels, cholesterol levels and blood pressure. Walking for 30 minutes every day, five days a week, will improve your health.
- Maintain your weight within a healthy range. Excess weight increases stress on the heart and is associated with high cholesterol, high blood pressure and diabetes. Losing weight will reduce your risk of heart disease.
- Manage your stress. To reduce your risk of heart attack, reduce the number of stressful situations in your daily activities. Rethink your lifestyle at work and find a healthy way to minimize stressful situations in your life.
- Eat healthy. High levels of saturated animal fat and cholesterol in the diet lead to narrowing of the arteries of the heart. If you have had a myocardial infarction, limit your intake of fat, cholesterol, and salt. A diet with high salt levels increases blood pressure levels. Ask your doctor or nutritionist for advice on foods recommended for preventing atherosclerosis. Prepare healthy meals with your family members. Fish is one of the components of a healthy diet. It contains omega-3 unsaturated fatty acids, which help improve cholesterol levels and prevent blood clots. Eat enough vegetables and fruits. Fruits and vegetables contain antioxidants, components that help prevent damage to the wall of the coronary arteries.
- If you drink alcohol, consume it in moderation. Don't start drinking alcohol if you haven't done so before. Moderate alcohol consumption helps increase the level of high-density cholesterol, “good” cholesterol, and has a protective function in the development of myocardial infarction. Men are advised to drink no more than two drinks a day, and women no more than one. Excessive alcohol consumption increases blood pressure and triglyceride levels, increasing the risk of heart attack. One serving of alcohol is equivalent to 350 ml of beer, 120 ml of wine or 45 ml of spirits.
Symptoms and signs of myocardial infarction in women
Female heart attacks have a number of atypical features and are less studied compared to male ones. The thing is that women are less likely to suffer from coronary heart disease. They are helped in this by estrogen, a hormone that is produced by the female body almost throughout life. It prevents the development of atherosclerosis. After menopause, the amount of estrogen in the body decreases and the chances of developing coronary heart disease in women increase.
Precursors of myocardial infarction in women are often swelling of the extremities that appear at the end of the day, chronic fatigue, shortness of breath, and digestive problems.
Often, a heart attack in women occurs without severe chest pain and may be accompanied by nausea, high fever and high blood pressure. Sometimes a false toothache develops. There are also cases of asymptomatic heart attacks.
This course of the disease is much more dangerous, since the patient can endure the first signs of the disease without attaching much importance to them. Some patients who have experienced a heart attack find out about it only after a while, undergoing diagnostics.
Patient support
Myocardial infarction is an unpleasant experience. Even if your doctor says everything is fine, you may still feel anxious. How will this affect your life? Will you be able to return to work or resume activities that bring you satisfaction? Will this happen again? Fear is one of the many experiences you and your loved ones will face. Other experiences after a heart attack include:
- Anger. You get angry and wonder, “Why did I have a heart attack and why now?” Feeling resentful after a myocardial infarction is a normal human reaction.
- Guilt. Family members feel guilty about your illness or take responsibility for actions that they believe caused the heart attack.
- Depression is common after myocardial infarction. You will feel that you are no longer able to do things that were previously acceptable, that you are no longer the same person you were before. Medical rehabilitation programs are effective in preventing and treating depression after myocardial infarction. It is important to tell your doctor about the signs and symptoms of depression.
These experiences arise most often and discussing them openly at a consultation with a cardiologist, with family members or a close friend will help to cope with them more effectively. You must take care of your physical and mental rehabilitation. Exercise and group activities with people who have also had heart attacks can help you cope with negative experiences and feelings.
What is a “silent heart attack”?
In people over 75 years of age and with diabetes, a “silent heart attack” may occur, which is not accompanied by pain at all.
Experts estimate that approximately one fifth of such heart attacks are not diagnosed. Damage to the heart muscle in survivors of a “silent heart attack” progresses because it is not detected and treated. Abdominal fat destroys the heart
The maximum permissible waist circumference for women is 94 centimeters, for men – 102 centimeters. Exceeding these values increases the risk of cardiovascular disease. Find out more about the dangers of visceral (intra-abdominal) fat and how to get rid of it.