As part of the implementation of the program of state guarantees of free medical care, an appointment with cardiologist Iskra M.A. was organized. to resolve the issue of the need to perform coronary angiography , make an appointment by calling 234-41-81, 234-41-64.
Coronary angiography is radiographic visualization of the coronary arteries after the administration of radiocontrast agents. In terms of its significance and value, diagnostic coronary angiography occupies a leading place in the diagnosis of coronary artery disease. Visualization of the coronary arteries allows you to make the right choice in terms of treatment tactics and determine the specific type of treatment.
Assessment of the anatomical variant of coronary artery lesions allows one to make a choice in favor of coronary artery bypass grafting or percutaneous coronary intervention, and in some cases limit oneself to drug therapy. When performing coronary angiography and percutaneous coronary intervention, the use of intravascular ultrasound, optical coherence tomography, intravascular thermography, determination of the intravascular pressure gradient and coronary blood flow reserve significantly improves the quality of diagnosis and the results of percutaneous coronary intervention. The risk of significant complications during coronary angiography is less than 1%.
Coronary angioplasty and stenting
What is coronary angioplasty?
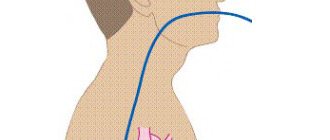
This is a treatment method in which percutaneous coronary intervention (PCI) is performed to open cholesterol-blocked coronary arteries (most likely caused by coronary heart disease - CAD) and restore arterial blood flow to the heart tissue without open-heart surgery. A special catheter (a long, hollow tube) is inserted into the coronary artery that needs to be treated to free it from the blockage. This catheter has a tiny balloon at the end. The balloon is inflated once the catheter is placed in the narrowed (ie, damaged, unhealthy) area of the coronary artery. The inflating balloon compresses the fatty tissue in the artery and frees the artery from blockage, leaving it open inside, which improves blood flow.
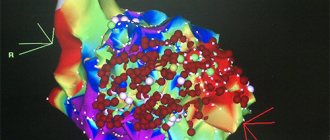
Application of fluoroscopy. A special type of X-ray helps the doctor more accurately assess the extent of damage to the vessel, exactly where the blockage in the coronary artery is located, and show how the contrast agent passes through the arteries.
Intravascular ultrasound is a technique that uses a computer and a transducer to send sound waves to create images of blood vessels. These images can be used during PCI. The use of intravascular ultrasound (IVUS) provides direct visualization and measurements inside blood vessels. IVUS can help the physician select the appropriate size of balloons and/or stents (a thin metal structure that helps keep a blood vessel open), so that the stent, if used, is properly exposed, and can also help evaluate the use of other angioplasty tools.
What is a stent?
Coronary stents are now almost universally used in percutaneous coronary intervention procedures, often after balloon angioplasty, which opens the narrowed artery and facilitates advancement of the stent. A stent is a tiny, expandable, coiled piece of metal that is inserted into an open section of an artery during surgery to keep the artery from narrowing or closing. Once the stent is placed, tissue begins to form over it within a few days of the procedure. The stent will be completely covered with tissue within a month or so. You may need to take medications—Aspirin, Clopidogrel (Plavix), Prasugrel (Effient), or Ticagrelor (Brilinta)—that reduce the “stickiness” of platelets (special blood cells that clump together to stop bleeding) to prevent blood clots from forming inside the stent. The doctor should give the patient specific instructions about what medications to take and for how long.
The new generation of stents are coated with a drug to prevent scar tissue from forming inside them. The drug inhibits tissue growth that can occur within the entire length of the stent. The effect of the medicine is to prevent new narrowing of the stented blood vessels. Because stents can become clogged, it is important to talk to a doctor about what a patient should do if they experience chest pain after having a stent placed. If the scar tissue is inside the stent, a repeat procedure can be done with either balloon angioplasty or a second stent, and sometimes local radiation therapy (called brachytherapy) to clear the scar area and open the vessel.
Indications for angioplasty and stenting
Main indications
Percutaneous coronary intervention is performed to restore coronary blood flow to the arteries when the arteries are narrowed in a place that can be achieved just by angioplasty and stenting. However, not all coronary artery diseases can be treated with percutaneous coronary intervention.
— Coronary heart disease (CHD). CAD is a narrowing of the coronary arteries (blood vessels that supply oxygen and nutrients to the heart muscle) caused by the accumulation of fat in the artery walls. CAD is a process that causes a narrowing inside an artery, limiting the supply of oxygen-rich blood to the heart muscle.
The heart is a kind of pump. The heart is made up of specialized muscle tissues called the myocardium. The main function of the heart is to pump blood throughout the body so that all tissues in the body can receive oxygen and nutrients.
Like any pump, the heart requires fuel to operate. The myocardium requires oxygen and nutrients, like any other tissue in the body. However, the blood that passes through the chambers of the heart travels to the rest of the body. This blood does not provide oxygen and nutrients to the myocardium. The myocardium receives oxygen and nutrients from the coronary arteries, which lie outside the heart.
- Angina pectoris. When heart tissue does not receive adequate blood supply, it cannot function as it should. If the blood supply to the myocardium decreases for some period, then ischemia develops. Ischemia can reduce the pumping ability of the heart because the lack of nutrients and oxygen weakens the heart muscle.
Unfortunately, a patient may not have any symptoms of early CAD, but the disease may continue to progress until severe blockage of the arteries occurs, resulting in angina (this is chest pain or discomfort due to CAD). Symptoms of angina include: chest or arm pain, chest pressure, fatigue, upset stomach, palpitations and shortness of breath.
- Myocardial infarction. If a coronary artery is completely blocked by a blood clot, a myocardial infarction (heart attack) can occur. A blood clot can occur due to plaque (a buildup of fatty tissue in the artery walls) or rupture, which causes clots to rapidly accumulate in the area and block blood vessels. If blood flow to a specific area of the damaged heart muscle cannot be restored quickly, the tissue dies.
Angioplasty and coronary stenting are indicated for the following categories of patients:
- With a low level of narrowing of the coronary vessel,
- If there is access to the site of vessel narrowing during angioplasty,
- When the narrowing is not in the main artery of the heart, which delivers to the left side of the heart,
- In the absence of heart failure.
Before angioplasty and stenting, angiography is performed - an X-ray method for studying the condition of the coronary arteries, which is carried out, in principle, in the same way as angioplasty itself.
Angioplasty and coronary stenting operations are so-called minimally invasive interventions, that is, they are not associated with classical incisions, opening of the chest and pericardial cavity, which allows the patient to undergo the operation much easier. Consequently, the patient can move on to the next stage of treatment—cardiac rehabilitation—earlier.
CARDIOLOGICAL REHABILITATION AFTER ANGIOPLASTY AND CORONARY STENTING
Rehabilitation after angioplasty and coronary stenting is similar in its basic principles to rehabilitation after other surgical and non-operative methods of treating coronary heart disease (CHD).
Therapeutic exercise is the main link in cardiac rehabilitation after angioplasty and coronary stenting. An excellent means of rehabilitation after angioplasty and stenting is health path.
A path is a walking ascent measured in distance, time and angle of inclination. Simply put, health path is a treatment method of dosed walking along specially organized routes.
Such walking with a measured load allows you to gradually train the heart and restore its function. In addition to walking and health paths, other types of physical activity are actively used - physical exercises, which in our sanatorium are individually selected for each patient, taking into account his general condition. Exercises on simulators are also used.
Physical exercise is the main thing in rehabilitation for heart disease. The fact is that the heart is a muscular organ, and like all other muscles, it can be trained, which, of course, restores its condition. In addition, physical activity is also useful in terms of combating excess weight. The more the patient moves, the more fat is “burned” in the body. And obesity, as is known, is one of the important risk factors for coronary heart disease.
Physical activity, as scientists have found, also has a positive effect on the patient’s emotional state, which is important in terms of combating stress and depression that occur in such situations. During physical activity, the blood supply to all organs and tissues in the body improves, and the delivery of oxygen to all cells of the body is normalized.
Secondary prevention is an integral measure for the prevention of recurrent myocardial infarction and cardiac rehabilitation. This includes strict control of blood pressure and lifestyle, giving up bad habits - smoking and alcohol, regular exercise and diet.
Diet is another important aspect of rehabilitation.
A proper diet is important for the prevention of atherosclerosis, the main cause of coronary artery disease. A nutritionist will develop a diet especially for you, taking into account your taste preferences. Of course, you will have to give up certain foods. Eat less salt and fat, and more vegetables and fruits. This is important, since if excess cholesterol continues to enter the body, physical therapy will be ineffective.
Our body produces the cholesterol it needs on its own. And with animal food we inevitably get additional cholesterol. Therefore, it is important to limit, first of all, fatty foods - fatty meat, lard, butter, sour cream. Of course, it is hardly possible to completely give up fatty foods, but everyone can sharply limit their fat intake.
Psychological rehabilitation is an important link in the chain of all cardiac rehabilitation. Constant stress is a risk factor for the development of coronary artery disease, myocardial infarction and stroke. Professional psychologists can help you cope with stress and depression.
Stent thrombosis after PCI
In patients with acute coronary syndrome with ST segment elevation (STES), primary percutaneous intervention (PCI) results in a 47% reduction in mortality compared with thrombolytic therapy (4.3% vs 9.2%). In NSTE-ACS, invasive revascularization improves the prognosis in patients at high and intermediate risk of death. The increasing number of PCI with stenting in ACS is accompanied by the risk of complications in the form of stent thrombosis. To illustrate this problem, we present a clinical case. Key words: acute coronary syndrome; OKSpST; ACS without pST; PCI; stenting. In recent years, there has been a continuous increase in the number of primary percutaneous interventions (PCI) for acute coronary syndrome (ACS) [4,5]. However, simultaneously with the increase in the frequency of PCI with stenting, the problem of the development of stent thrombosis and stenosis is growing [1, 6]. The incidence of stent thrombosis is 0.87–2.2% and occurs more often during the first year after surgery [3]. Stent thrombosis is verified if angiographic or pathological confirmation is available. Angiographic confirmation of stent thrombosis based on TIMI flow status is sufficient if there is a new acute onset of resting ischemic symptoms; new ischemic ECG changes, typical increase in markers of myocardial necrosis [7]. Stent thrombosis can develop during the first 24 hours after its installation (acute stent thrombosis), during the 1st month (subacute thrombosis) or from the 1st to 12th month after the intervention (late stent thrombosis). The primary factors contributing to its occurrence are the initial occlusion of the coronary arteries, a long (more than 25 mm) stented segment of the coronary artery, and discontinuation of dual antithrombotic therapy after endovascular intervention [3, 6].
Patient T., 72 years old, was hospitalized with a diagnosis of Unstable angina. Upon admission, he complained of periodically occurring pressing pain in the chest, of moderate intensity, occurring at rest during the last week and relieved by taking nitrates for 5 minutes. Hospitalized by gravity.
From the anamnesis: For a long time, the patient notes increases in blood pressure, maximum blood pressure figures = 180/100 mmHg. usual numbers BP = 110-130/70 mmHg. Since 1980, pressing pain in the chest appeared during exercise, and in 1985 he suffered a myocardial infarction. In 2011, he suffered a hemorrhagic cerebral infarction in the right hemisphere, focal neurological symptoms regressed. Repeatedly underwent PCI on the coronary arteries: TLBAP and LAD stenting in 2001 and 2003, TLBAP and VTK stenting in 2021. After VTK stenting in 2021, the clinical course of angina regressed, chest pain occurred very rarely. Since September 2021, the patient has returned to the angina clinic; a coronary angiography (CAG) was performed at the Federal State Budgetary Institution of the Federal Clinical Clinical Center for Medical and Internal Medicine (FMBA), LAD restenosis was detected, and TLBAP of restenosis was performed, without stenting. Over the past month, the patient's angina symptoms have progressed, tolerance to physical activity has sharply decreased, pain began to occur at rest, and the need for nitrates has increased. Last hospitalization at the Federal State Budgetary Institution National Medical Research Center for Cardiovascular Surgery named after. A.N. Bakulev from 06/13/2018 to 06/18/2018. On June 15, 2018, coronary angiography was performed, it was revealed: the left coronary artery trunk is not changed, previously implanted stents in the s/3 LAD are patent, further restenosis is 90%, a. intermedia stenosis p/3 from the mouth 90%, LMZHV OV stenosis p/3 to 55%, RCA is not changed.
Upon discharge, the patient is recommended to take the following medications: acuside 20/12.5 x 2 times, physiotens 0.4 mg x 2 times, Co-Plavix 100/75 mg in the morning, Preductal OD 80 mg in the morning, atorvostatin 40 mg in the evening, Cardura 4 mg in the evening .
After discharge from June 19, 2018, the patient’s symptoms of angina pectoris and chest pain at rest progressed, and he was forced to use sublingual nitrates several times a day. He sought medical help at Clinical Hospital No. 1 of the UDP and was sent to the ICU with the diagnosis: “IHD: unstable angina. PEAKS. Multivessel coronary lesion."
Objectively: The condition is serious. Position in bed with a low headboard. Body type – normosthenic. Increased nutrition. Height - 168cm, weight - 80kg. BMI-28.3 kg/m2, Overweight.
The skin is of normal color, dry, warm. Normothermia. There is no cyanosis of the lips, no acrocyanosis. There is no swelling. L/U are not enlarged. There are no varicose veins.
CNS: Oriented to place, time, self. Conscious, communicative, adequate. Memory and intelligence are preserved. Pupils D=S. Tongue in the midline. Sensitivity and movement in the limbs are fully preserved. No paresis or paralysis was detected. In the neurological status, focal and meningeal symptoms are not detected.
Respiratory organs: Breathing is independent, nasal, adequate. NPV 18 per minute. SpO2 97% in atmospheric air. Percussion sound is pulmonary with a boxy tint.
Auscultation: vesicular breathing, carried out in all departments. Single dry pneumosclerotic rales on both sides.
Cardiovascular system: The veins of the neck are not swollen. Pulsation of the carotid arteries without any features. The borders of the heart are expanded to the left by 1.5 cm. Heart sounds are muffled and rhythmic. The ECM records sinus rhythm. Heart rate=62, PS=62 per minute, blood pressure 140/76 mmHg. No pathological noises are heard. The pulsation in the arteries of the feet is reduced, more on the right.
Gastrointestinal organs: The tongue is moist. Appetite preserved. The abdomen is soft and painless on palpation in all parts. The liver does not protrude from under the edge of the costal arch and is painless on palpation. The spleen is not palpable. Bowel sounds are heard. The chair is a regular color, decorated.
Urinary organs: Independent urination. There is no dysuria. The effleurage symptom is negative on both sides.
Blood tests for cardiac biomarkers: 06/22/18 12:31 (1st analysis) Troponin-I quantitatively: 28.3 ng/ml; KFK-MB (CK-MB): 27 units/l; Total cholesterol: 2.5 mm/l; LDL: 1.51 mm/l 06/22/2018 23:11 (2nd analysis): Troponin-I quantitatively: 163.8 ng/ml; KFK-MB (CK-MB): 27 units/l; 06/23/2018 06:19: Troponin-I quantitatively: 10235 ng/ml; KFK-MB (CKMB): 755 units/l;
CAG dated 06.22.18: Access: right transradial Study results: LCA. Barrel Not changed. LAD The previously implanted stent in p/3-s/3 is passable, restenosis is 99%, further unchanged. DV Wellhead narrowing 45%, further unchanged. A. intermedia Irregularities of contours in n/3 (small-diameter artery). OS Without hemodynamically significant changes. VTK The previously implanted stent is passable from the orifice, without signs of restenosis, and further without changes. WPV OS Without hemodynamically significant changes. RCA Without hemodynamically significant changes. WMA of RCA Without hemodynamically significant changes. LMWH RCA Without hemodynamically significant changes. Type of blood supply: Balanced.
Progress of the operation: Under local anesthesia sol. Lidocaini 2% - 5.0 the right radial artery was punctured. 10 thousand units were introduced. heparin. A 6F guiding catheter was passed into the ascending aorta and installed at the ostium of the left coronary artery. The coronary guidewire was placed in d/3 of the LAD. Next, after preliminary dilatation with a 2.0x20 mm balloon catheter (12 atm), stenting of the p/3-s/3 LAD was performed. A Resolut stent 2.73x18 mm (14 atm) was implanted. Postdilatation of the implanted stent was performed using a 2.75x15mm (20 atm) balloon catheter. Angiography revealed extravasation of n/3 LAD. A 3.0×23 (14 atm) Aneugraft stent-gravity was implanted in the segment of artery extravasation (n/3 LAD). During control angiography, there is no extravacation. The patient is hemodynamically stable.
. EchoCG dated June 22, 2018: PPT 1 Myocardial mass g LV MM index g/m2 AORTA: 27 mm (N up to 40 mm). AORTIC VALVE: opening amplitude: 18 mm (N > 15 mm); Blood flow speed 1.33 m/sec. Gradient 7.2 mmHg; LEFT ATRIUM: D 45X61 mm (N up to 4.0 cm); V= 81 ml. LEFT VENTRICLE: CDR 4.7 cm (N up to 5.6 cm); DAC cm (N up to 3.7 cm); KDO 124 ml; KSO 47 ml; EF 62%. Relative wall thickness = (norm up to 0.42) IVS THICKNESS 1.4-1.7 cm (N up to 1.1 cm); THICKNESS OF THE ZSLZH 1.3 cm (N up to 1.1 cm). RIGHT ATRIUM: 36 mm. RIGHT VENTRICLE: D 29 mm. MITRAL VALVE: Regurgitation: max. speed of peak E: 0.6 cm/s, peak A 0.9 cm/s; mitral orifice area cm2; diameter of the annulus fibrosus SIGNS OF PULMONARY HYPERTENSION: NO; MPAP 17 mm Hg. PERICARDIAL: NO effusion. Conclusion: Atherosclerosis of the aorta. Calcification of the aortic and mitral valves. Dilatation of the left atrium. Local and global contractility is preserved. Concentric hypertrophy of the LV myocardium.
06/22/18 16:50 The patient was delivered from the cath lab after endovascular intervention - LAD stenting. During the stenting process, extravasation was detected, and therefore a stent-gravt was installed with a positive angiographic effect.
Complaints of intense pressing pain in the heart area, weakness, moderate shortness of breath associated with the inability to breathe deeply due to pain in the heart area.
ECG: sinus rhythm, ST elevation from V1-V, ST depression in II, III, AVF.
Infusion of neoton, isoket, and non-narcotic pain relief was started. It was decided to refrain from carrying out a massive anticoagulant therapy due to the risk of internal bleeding from the site of LAD injury.
At the moment, based on the clinical picture, the characteristic ECG picture, the echocardiographic picture, the clinical picture is interpreted as an acute type IV myocardial infarction in the region of the anterolateral wall of the LV with ST segment elevation.
06/23/18 00:30
A condition with negative dynamics in terms of the resumption of intense chest pain.
Due to severe pain, a decision was made to use narcotic painkillers.
When recording an ECG, pronounced negative dynamics were revealed in terms of expansion of the ischemic zone and an increase in ST segment elevation.
In agreement with endovascular surgeons, a decision was made to repeat CAG.
06/23/18 2:00
The patient was delivered from the cath lab after endovascular intervention - re-stenting of the LAD due to restenosis in the area of the previously implanted stent.
Against the background of revascularization, complaints of pressing pain in the heart area significantly regressed.
The ECG shows positive dynamics in terms of reducing ST elevation from V2-V4.
CAG 06.23.18 01:20: Name of operation: Recanalization, balloon vasodilation with installation of a stent in the anterior interventricular branch. Type of anesthesia: local anesthesia
Research results: LCA. Barrel Not changed. LAD Occluded from the mouth. DV Wellhead narrowing 45%, further unchanged. A. intermedia Irregularities of contours in n/3 (small-diameter artery). OS Without hemodynamically significant changes. VTK The previously implanted stent is passable from the orifice, without signs of restenosis, and further without changes. WPV OS Without hemodynamically significant changes. RCA Without hemodynamically significant changes. WMA of RCA Without hemodynamically significant changes. LMWH RCA Without hemodynamically significant changes. Type of blood supply: Balanced.
Progress of the operation: Under local anesthesia sol. Lidocaini 2% - 5.0 the right radial artery was punctured. 10 thousand units were introduced. heparin. A 6F guiding catheter was passed into the ascending aorta and installed at the ostium of the left coronary artery. Conductor recanalization of n/3 LAD from the mouth was performed. The coronary guidewire was placed in d/3 of the LAD. Next, after preliminary dilatation with a 2.0x20 mm balloon catheter (12 atm), stenting of the LAD from the orifice was performed. A 3.5x30 mm Resolute stent (14 atm) was implanted. A good angiographic result was obtained.
Over the past period, the overall dynamics of the patient’s condition can be characterized as negative due to the development of acute myocardial infarction, accompanied by severe pain, requiring the use of narcotic painkillers, and a decrease in EF to 42%. Following repeated endovascular intervention, the patient's condition stabilized.
During the therapy, the patient's condition remains stable, with satisfactory hemodynamic parameters, no progression of cardiac/respiratory failure, and no cardiac arrhythmias. A repeat echocardiography study is planned. There were no signs of internal bleeding into the pericardial cavity due to damage to the LAD.
06/23/2018 Echocardiography: AORTA: 27 mm (N up to 40 mm). AORTIC VALVE: opening amplitude: 18 mm (N > 15 mm); Blood flow speed 1.33 m/sec. Gradient 7.2 mm Hg; LEFT ATRIUM: D 45X61 mm (N up to 4.0 cm); V= 81 ml. LEFT VENTRICLE: CDR 4.7 cm (N up to 5.6 cm); DAC cm (N up to 3.7 cm); KDO 101 ml; KSO 52ml; EF 49%. Relative wall thickness = (norm up to 0.42) IVS THICKNESS 1.4-1.7 cm (N up to 1.1 cm); THICKNESS OF THE ZSLZH 1.3 cm (N up to 1.1 cm). RIGHT ATRIUM: 36 mm. RIGHT VENTRICLE: D 29 mm. MITRAL VALVE: Regurgitation: max. speed of peak E: 0.6 cm/s, peak A 0.9 cm/s; mitral orifice area cm2; diameter of the annulus fibrosus SIGNS OF PULMONARY HYPERTENSION: NO; MPAP 21 mm Hg. PERICARDIAL: NO effusion. Conclusion: Atherosclerosis of the aorta. Calcification of the aortic and mitral valves. Dilatation of the left atrium. Hypokinesis of the apical segment of the lower wall and IVS. Global contractility is slightly reduced. Concentric hypertrophy of the LV myocardium. For DKG: MR-1-11 st., TR-1 st. Type 1 diastolic dysfunction. Behind the apex of the heart and the lateral wall of the LV, there is separation of the pericardial layers up to 3-4 mm (a small amount of fluid).
Diagnosis: Main diagnosis: IHD: repeated infarction (type IV) in the area of the anterior wall of the LV and the interventricular septum from 06.22.18. Post-infarction cardiosclerosis (MI in 1985) TBAP and LAD stenting in 2001 and 2003, TBAP and VTK stenting in 2021. Selective coronary angiography dated 06/15/2018: the left artery trunk is not changed, previously implanted stents in the s/3 LAD are patent, then restenosis is 90%, a. intermedia stenosis n/3 from the mouth 90%, LMZHV OV stenosis from/3 to 55%, RCA is not changed.
Balloon vasodilation surgery with installation of a 2.73x18 mm Resolut stent in the anterior interventricular branch of the left coronary artery on June 22, 2018, paravasation, installation of a LAD stent graft on June 22, 2018.
LAD stent thrombosis, recanalization, balloon vasodilation with installation of a 3.5x28 mm Xience stent in the anterior interventricular branch on June 23, 2018.
Background: Hypertension stage III, stage 3, risk 4. Diabetes mellitus type 2, moderate severity. Excess body weight. BMI=28.3 kg/m2.
Combined: Multifocal atherosclerosis: Stenosis of the left renal artery, stenting of the left renal artery in 2003, restenosis 95% (according to angiography dated June 15, 2018). Atherosclerosis of the vessels of the lower extremities: Thrombosis of the femoral artery on the left, operation ABBS in 2007. Angiography of the arteries of the lower extremities 06/15/2018: LEFT: OP stenosis 65%, IPA stenosis s/3 55%, BOTH, HBA, SPA and SFA without hemodynamically significant narrowings, RIGHT: SPA, IPA, IPA, BOTH and GBA are patent, SFA is occluded from the mouth, d/3 is filled along the collaterals.
Complications: Killip III AHF; recurrent left ventricular failure; NIV 06/25/18, 06/26/18.
Bilateral hypostatic polysegmental pneumonia. Acute aneurysm in the region of the LV apex. NRS: persistent form of atrial fibrillation-flutter.
Acute kidney injury, contrast-induced nephropathy.
Blockade of the right leg of the ganglion of Gis. NK IIA art. NYHA II FC. Nephroangiosclerosis. Nephropathy of mixed origin. CKD C3A, GFR according to the formula CKD-EPI=46 ml/min/1.73 m2.
Related: CVB. DEP II Art. ONMK from 2011
Cysts of the right kidney. Gastric ulcer, remission. COPD, moderate. Emphysema.
The course of the disease was complicated by acute left ventricular failure on June 23, 2018.
Discussion Thus, the patient had several reasons for the development of stent thrombosis - the presence of ACS itself, a decrease in EF, a long stented LAD segment, and initial subtotal arterial stenosis. The combination of male gender and age over 60 years were also additional predictors of stent thrombosis.
conclusions
1. After invasive revascularization in the scope of PCI with arterial stenting, additional stratification of patients is necessary according to the risk of developing stent thrombosis according to the presence of the most significant factors that increase the risk of its occurrence
2. Strict adherence to recommendations for DAPT in patients with ACS. The default duration of DAPT should be 12 months, regardless of the revascularization method. Ticagrelor is recommended for patients with ACS in the absence of drug contraindications. However, low-income patients require government support to purchase the drug, especially those with a high risk of developing stent thrombosis.
3. Work on maintaining patient compliance with drug therapy remains relevant.
Literature
1. Berezovskaya G. A., Ganyukov V. I., Karpenko M. A. Restenosis and stent thrombosis // Russian Journal of Cardiology. 2012. No. 6. pp. 91–95.
2. Ganyukov V.I. Evidence base for the priority role of primary percutaneous coronary intervention in revascularization of patients with ST-segment elevation myocardial infarction // Complex problems of cardiovascular diseases. 2013. No. 1. pp. 24–34.
3. Ganyukov V. I., Shilov A. A, Bokhan N. S., Moiseenkov G. V., Barbarash L. S. Causes of thrombosis of coronary artery stents // Interventional Cardiology. 2011–2012. No. 27/28. pp. 29–34.
4. Kashtalap V.V., Zavyrylina I.N., Barbarash O.L. Endovascular revascularization in acute coronary syndrome with ST segment elevation in Russia: problems and prospects for further development // Creative Cardiology. 2015. No. 3. pp. 5–15. BULLETIN OF BURYAT STATE UNIVERSITY. MEDICINE AND PHARMACY 2021. Vol. 4 50
5. ESC/EACT recommendations for the treatment of persistent ST-segment elevation myocardial infarction of the European Society of Cardiology. 2021. (escardio.ru).
6. Tereshchenko A. S., Mironov V. M., Merkulov E. V., Levitsky I. V., Samko A. N. Late and very late thrombosis of drug-eluting stents // Atherosclerosis and dyslipidemia. 2014. No. 1. pp. 9–14.
7. FDA Clinical Overview for Panel Packet DES Thrombosis Panel December 7-8, 2006. https://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4253b