Bradycardia is the medical term for an abnormally slow heartbeat. An abnormal baby's heart rhythm during pregnancy or childbirth is called fetal arrhythmia.
During pregnancy and childbirth, fetal bradycardia is often an important first sign that the baby is at risk. Fetal bradycardia occurs when the baby's heart rate drops below 110 for more than 10 minutes or 100 for 5 minutes.
The normal fetal heart rate is usually between 120 and 160 beats per minute. There are several different types of fetal bradycardia: sinus bradycardia, atrial ectopic block, and atrioventricular (AV) block. Early fetal bradycardia can be particularly concerning because if the baby's heart beats too slowly, he may not be getting enough oxygen in the blood to the brain.
general information
Modern medicine does not identify a decrease in heart rate as an independent disease, but regards it as a symptom of certain pathological processes. As a rule, in children (including newborns) and adolescents, a sinus form of cardiac bradycardia is detected, which may also be accompanied by arrhythmia.
Assessing the presence or absence of pathology requires an integrated approach, since heart rate norms depending on age are only average values.
Deadly pregnancy complication: who is at risk
Monitoring the course of pregnancy is 50% highly artistic pasting tests into a card, and 50% - performing completely routine procedures: weighing, measuring the abdomen with a centimeter tape, examining the limbs and measuring blood pressure (BP). On two hands. Necessarily. From an early date.
Once upon a time, the USSR managed to significantly reduce maternal mortality rates in a simple but surprisingly effective way.
A midwife was stationed in every small settlement who could measure a pregnant woman’s blood pressure and independently boil a portion of urine in order to find protein in it.
Simple midwives in the USSR and highly educated obstetrician-gynecologists in modern Russia are doing the same thing - persistently looking for signs of impending preeclampsia - a formidable and deadly complication of pregnancy.
What is preeclampsia?
This is a serious complication of pregnancy, in which the functioning of the entire body is seriously disrupted. In addition to the increase in blood pressure, a large amount of protein appears in the urine, the number of platelets in the blood decreases, the functioning of the liver and kidneys suffers, epigastric pain, visual disturbances, and severe headaches appear.
The condition can rapidly progress and lead to convulsions with loss of consciousness - eclampsia.
Preeclampsia begins after 20 weeks of pregnancy. The sooner, the more dangerous. Preeclampsia that develops before 32 weeks of pregnancy is considered early; pregnancy always ends prematurely, because attempts to preserve it can kill both mother and child.
Sometimes preeclampsia develops in the postpartum period, which is why obstetrician-gynecologists never relax.
Why is this happening?
Science still cannot give an exact answer to this question, despite the fact that the pathogenesis of the disease is well studied.
In some cases we can predict the development of the disease, but almost never we can prevent it.
At risk:
- primigravida;
- women who had preeclampsia in a previous pregnancy;
- preeclampsia in relatives (mother, sister);
- women who suffered from arterial hypertension before pregnancy or experienced an increase in blood pressure for the first time before 20 weeks;
- women with a history of kidney disease;
- women with diabetes mellitus, autoimmune diseases (systemic lupus erythematosus, scleroderma, antiphospholipid syndrome), thrombophilic conditions;
- obese women;
- women aged 40+ (another hello to all fans of the idea of delayed motherhood);
- multiple pregnancies;
- pregnancy after IVF
What is the child's risk?
Preeclampsia may require emergency delivery at any stage of pregnancy. This is often the only way to save the mother's life.
Severe prematurity in a newborn is a heavy burden that can affect the rest of a person’s life. Despite the breakthrough successes of modern neonatology, which has made it possible to nurse 500-gram babies, the mortality rate among premature babies is very high.
What does a woman risk?
Women who experience preeclampsia are likely to experience the condition in each of their pregnancies, with subsequent preeclampsia always more severe than the previous one.
Despite the fact that preeclampsia goes away with pregnancy, the risks of developing cardiovascular diseases, hypertension, stroke and heart attack remain.
Without adequate help, you may develop eclampsia, a severe seizure disorder similar to epilepsy. Acute renal failure, pulmonary edema are rapidly increasing, stroke or myocardial infarction, placental abruption, sudden intrauterine fetal death, retinal detachment with loss of vision can occur.
What is HELLP syndrome?
HELLP syndrome was first described in 1954. This is an abbreviation made up of the first letters: hemolysis - intravascular destruction of red blood cells (Hemolysis), increased activity of liver enzymes (Elevated Liver enzymes) and thrombocytopenia (Low Platelet Count).
This serious and potentially fatal condition is accompanied by severe blood clotting disorders, necrosis and rupture of the liver, and cerebral hemorrhages.
Dangerous symptoms
You should immediately consult a doctor if swelling appears on the face and hands, headaches that do not go away after taking conventional medications, blurred vision - blurred vision, “veil and fog”, flashing “spots” before the eyes.
Preeclampsia can manifest itself as pain in the epigastric region, right hypochondrium; nausea and vomiting in the second half of pregnancy, difficulty breathing are dangerous. A sudden weight gain (3-5 kg per week) may be a warning sign.
Preeclampsia is not mild
The most difficult thing for an obstetrician-gynecologist is not to panic ahead of time. Sometimes the situation allows you to delay time a little to allow the fetal lungs to ripen.
Up to 34 weeks, corticosteroids are administered to prevent respiratory distress syndrome. Sometimes the situation quickly worsens and requires immediate action and delivery.
How to prevent preeclampsia?
Unfortunately, doctors can predict many obstetric complications, but cannot prevent them. Over the years of research, a long list of disappointments has accumulated. The bed-rest regimen (resting in a lying position during the day), limiting table salt, fish oil or taking garlic tablets will definitely not help prevent the development of preeclampsia.
Neither taking progesterone medications, nor using magnesium sulfate, nor taking folic acid, nor using heparins, including low molecular weight ones (Clexane, Fraxiparin) is not a preventive measure. However, all of these drugs can be used during pregnancy for other purposes.
If the risk of preeclampsia is high, your doctor may suggest taking acetylsalicylic acid daily after the 12th week of pregnancy.
Pregnant women with low calcium intake (<600 mg per day) are advised to take supplemental calcium in the form of medications.
The best thing you can do is take care of prevention before pregnancy. Hypertension should be well controlled before conception.
Obesity requires weight loss, diabetes requires compensation and reliable control. Unfortunately, this is the right but difficult path.
Most often, women come into pregnancy with a whole bunch of problems that require urgent solutions.
Obstetricians and gynecologists around the world continue to measure blood pressure. On two hands. On every visit. And they ask you not to forget to regularly take a general urine test. This is a life-saving strategy.
Oksana Bogdashevskaya
Photo depositphotos.com
The opinion of the author may not coincide with the opinion of the editors
Symptoms of bradycardia in children
A mild form of sinus bradycardia in a child or adolescent does not cause any pathological symptoms.
The body tissues receive a sufficient amount of oxygen, so that the baby does not experience discomfort. With a significant slowdown in heart rate, signs of tissue oxygen starvation appear: fatigue, drowsiness, decreased performance at school, and forgetfulness. As the disease progresses, dizziness of varying severity appears, leading to falls and loss of consciousness. In this case, the skin becomes pale with a bluish tint, blueness appears around the mouth and cold, sticky sweat appears. As a rule, the attack lasts a few seconds. With constant bradycardia, fainting often occurs due to being in a stuffy room, stress, or physical overload.
Causes of bradycardia in children
Bradycardia is, first of all, a reaction of the heart to certain conditions. In this regard, the list of reasons that can cause such a problem is very long. The most important factors are:
- physiological: natural causes that do not indicate the presence of pathology;
- cardiac: associated with heart pathology;
- endocrine: associated with disruption of the endocrine glands;
- neurological: caused by a malfunction of the nervous system;
- intoxication: acute or chronic poisoning;
- genetic: hereditary pathology, for example, constitutional familial bradycardia;
- other reasons: gastrointestinal pathology.
Depending on the age of the baby, certain groups of factors predominate among the most likely causes.
Bradycardia in premature and newborn babies
A reduced heart rate at premature birth is physiological and is associated with the immaturity of heart rate regulation systems. With proper care and medication support, the condition gradually improves. The most common causes of bradycardia in a newborn child are heart defects, various types of encephalopathy, and birth injuries. Sometimes a pronounced decrease in heart rate indicates the development of transverse atrioventricular block (AV block). This is a dangerous condition that requires immediate medical attention.
Bradycardia in children of the first year of life (infants)
At this age, the pathological condition can be caused by the same reasons as in newborns. In addition, it is worth paying attention to the level of thyroid hormones. Hypothyroidism often causes a slow heart rate.
Bradycardia in preschool children
Bradycardia in a child aged 2 to 7 years is often associated with infectious diseases that are complicated by myocarditis - inflammation of the heart muscle. Poisoning and drug overdoses are also common at this age. The third common cause of bradycardia in a child aged 3–4 years and older is adenoids. Difficulty in nasal breathing leads to chronic hypoxia, causing a decrease in heart rate.
Bradycardia in schoolchildren and adolescents
A decrease in heart rate at school age may be due to the same reasons as in preschoolers, but they are accompanied by various types of gastritis and duodenitis associated with changes in diet.
Teenagers often encounter the manifestation of vegetative-vascular dystonia, which can occur according to the vagotonic type. A decrease in heart rate is accompanied by a drop in blood pressure, dizziness, and fainting. At the same age, autoimmune diseases and sick sinus syndrome often manifest.
Sinus bradycardia of the heart in adolescent athletes, which is not a symptom of the disease, stands apart. Regular intense exercise leads to the development of a physiological decrease in heart rate at rest, as the heart adapts to the additional work during exercise.
Fetal heart rate norms
The fetal heart rate is monitored throughout pregnancy. The duration of the checks depends on the health status of the woman and the fetus. If increased or decreased parameters are detected, measurements are carried out more often; in the normal course of pregnancy - less often. Standard heartbeat rates in an embryo are from 110 to 170 beats/min. It depends primarily on the duration of pregnancy. Indicators below the lower norm indicate bradycardia, and those exceeding the upper parameters indicate tachycardia.
In the early stages
The embryo's heart develops starting from the 2nd week, beats from the 3rd week, you can listen to it from the 6th, and sometimes from the 8th, when all the heart chambers are already formed. In the early stages of pregnancy, fetal heart rate norms are relative. The doctor's job is to make sure he is alive. At the very first stages of the formation of a child’s heart in the womb, it beats very slowly - 15-40 beats per minute.
The baby's heartbeat must be within a certain range. Deviation from the norm affects the development of the fetus.
Gradually, the beating of the fetal heart in the womb due to the formation and development of veins, blood vessels, and the aorta becomes more frequent by 3-4 points every day. On the 5th week it is 81-103 beats/min, on the 6th - 104-126, on the 7th - 127-149, on the 8th - 149-172, on the 9th - about 175. Further, due to the development of the nervous system, which is responsible for the functioning of internal organs, it begins to gradually decrease - to 170 beats/min. at the 10th week, 165 - at the 11th, 162 - at the 12th, 159 - at the 13th, 157 - at the 14th. Considering that the size of the embryo at the same time differs among different women, another definition of the variant of the heart rate norm is used. If the length of the fetus is about 5 mm, then the optimal indicators for it are about 100 beats per minute, and if it is longer - 120-130. An alarming symptom is if, when the size of the embryo is 8 mm or more, its heartbeat cannot be heard. Most often this indicates fetal freezing.
In the later stages
Starting from the 20th week, the doctor can determine the state of fetal development based on the heart rate.
In later stages, the possibilities for diagnosing the state of the fetal cardiovascular system expand. During the study, it is possible to listen not only to the number of heart rate beats, but also to the characteristics of the pulse and the position of the myocardium. Starting from the second trimester, the fetal heart rate should be 140-160 beats/min. both at the 22nd week and at the 33rd. Closer to 40, on average they range from 130 to 140 beats/min. Small deviations are possible, since these are still individual parameters that depend on the physiological characteristics of the pregnant woman, her emotional state, the size of the embryo, the genetic component and many other factors. The main thing is that they should not fall below 85 beats/min. and rise above 200.
Diagnosis of bradycardia in children
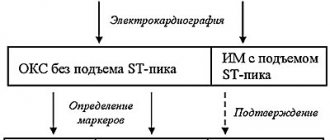
A pediatric cardiologist diagnoses bradycardia in children of any age. Its tasks include not only identifying the fact of a slow heart rate, but also searching for the cause of this condition, as well as selecting adequate treatment. In addition to a basic examination, listening to heart sounds, assessing pulse and measuring blood pressure, the examination includes:
- ECG;
- daily ECG monitoring (Holter);
- Ultrasound of the heart;
- stress tests: bicycle ergometry, treadmill test, atropine test;
- laboratory diagnostics: general blood test, assessment of hormonal status, etc.
Additional research and consultations may be aimed at finding a specific cause. Depending on the indications, an ultrasound scan of the thyroid gland and adrenal glands is performed, the content of electrolytes in the blood is assessed, etc.
Why does bradycardia develop in the fetus?
The main causes of bradycardia in the embryo on the part of a pregnant woman:
- anemia;
- oligohydramnios/polyhydramnios or multiple pregnancy;
- pathologies of the cardiovascular and respiratory systems;
- unhealthy lifestyle (bad habits, low physical activity);
- infections;
- taking toxic medications;
- hypotension, etc.
Causality of pathology from the fetus:
- prolapse of the umbilical cord or entanglement in the umbilical cord;
- intrauterine growth retardation;
- premature placental abruption;
- prolonged hypoxia;
- pelvic position of the fetus.
Treatment of bradycardia in children and adolescents
Treatment of mild or moderate bradycardia and arrhythmia in a child of any age is aimed at normalizing the heart rate, as well as eliminating the cause of the pathological condition.
Depending on the situation, emergency medications and ongoing medications may be used to stabilize the heart. The choice of treatment method for bradycardia is made by a cardiologist. If a child develops severe bradycardia, accompanied by frequent fainting, Morgagni-Adams-Stokes attacks and other conditions that disrupt the usual rhythm of life, surgical treatment is used. Experienced cardiac surgeons implant an electrical pacemaker that controls the functioning of the heart. This treatment is also relevant if the condition arose against the background of severe defects and blockades.
Prognosis and prevention
The prognosis for bradycardia in a child depends on its cause and severity. In some cases, it is enough to adjust lifestyle or hormonal status to normalize heart function, while in others complex treatment and lifelong monitoring are required. Prevention of the development of pathology includes, first of all, teaching the child to a healthy lifestyle, prevention and timely treatment of diseases that can provoke this condition.
If your child or teenager is experiencing bradycardia, do not wait for the disease to progress; make an appointment with the pediatric cardiologists of the SM-Doctor clinic. You will receive a comprehensive examination, modern and effective treatment if necessary, as well as regular supervision by an experienced specialist.
Decoding the results
The child's heart rate should be 120-160 beats per minute.
- If the fetal heart rate is below 110 bpm (bradycardia), doctors may suspect progressive fetal hypoxia.
- If the heart rate is more than 160 beats, the fetus has tachycardia (which can be caused by an intrauterine infection).
Such data allows specialists to quickly respond to alarm signals.
It is important to understand that an abnormal fetal CTG is not always an indicator of a problem! A result within the normal range is always a good sign, but if there are any warning signs, the specialist must take other factors into account. Sometimes increased or decreased indicators of fetal cardiac activity can even be caused by the mother’s uncomfortable position during the examination or her excessive anxiety.