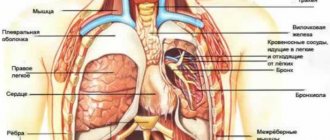
Dyspnea is a pathological disorder in the respiratory system, characterized by changes in the frequency, depth and rhythm of breathing.
Often accompanied by the following symptoms:
- feeling of lack of air;
- noise when inhaling and exhaling;
- feeling of tightness in the chest;
- increased heart rate during exercise;
- attacks of suffocation.
Content:
- Symptoms of pathology
- Options for shortness of breath after Covid-19
- How to assess lung function after COVID-19 3.1. Difficulties in self-diagnosis
- How to treat shortness of breath after coronavirus 4.1. Medicines for shortness of breath 4.2. Oxygenation 4.3. Inhalations 4.4. Physiotherapeutic procedures 4.5. Breathing exercises
- Ways to improve lung function on your own
COVID-19 takes its toll throughout the body, but it most commonly affects the lungs. Shortness of breath after Covid is common. It occurs both in people who have had pneumonia and in those who have not encountered serious complications during their illness.
Scientists have found that in approximately 20% of those recovering, the function of the lung tissues has worsened. Patients gasp for air if they are in a hurry, are unable to lie on their back for a long time, and quickly get tired when doing even simple physical work. Things are especially bad for people diagnosed with pulmonary fibrosis, which leads to scarring of the paired organ.
Under normal conditions, fibrosis is rare. It is most often encountered by people over the age of sixty. With this diagnosis, shortness of breath is a concern. It can be so strong that it is difficult for a person to talk and move.
We suggest you figure out why difficulty breathing after coronavirus bothers you, and how to recognize and eliminate dangerous symptoms. It is important to know this information to prevent complications from Covid-19 from progressing.
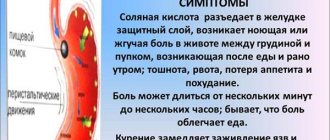
Symptoms of pathology
With difficulty breathing, the patient cannot take a deep breath. He makes at least 22 breathing movements per minute. This is typical for moderate pneumonia. In severe cases of the disease, the number of inhalations and exhalations per minute exceeds 30.
A severe inflammatory process is recorded in the lung tissues. A person’s body temperature rises and a nonproductive dry cough occurs. It also happens that there are no accompanying symptoms. Then we can assume that shortness of breath is caused by panic attacks, psychosomatics, and fear.
If, when listening to the lungs, the doctor hears wheezing or whistling, it means there is coronavirus pneumonia and the bronchi are affected. This clinical picture is often observed in individuals with concomitant bronchitis, bronchial asthma, and secondary bacterial infection. It often precedes pulmonary edema.
Difficulties with breathing after coronavirus can be described as follows:
- feeling of tightness in the chest;
- rapid breathing;
- performing shallow breathing movements;
- heaviness when trying to take a deep breath.
Shortness of breath in itself is not a disorder in healthy people. Runners and athletes encounter it. If the onset of the symptom was preceded by difficult physical work, then shortness of breath is the norm. During and after coronavirus, the problem manifests itself even at rest. And this is a dangerous sign. It indicates that the body is suffering due to oxygen deficiency. As you know, in conditions of oxygen deficiency, not a single internal organ works fully.
Respiratory neurosis
There are many types of neuroses, each of which is distinguished by a specific group of symptoms. One of them is respiratory neurosis, which is characterized primarily by neurogenic breathing disorder.
The concept was introduced into use in 1871 by the American scientist Da Costa. It has several related names: “respiratory neurosis”, “neurorespiratory syndrome”, “respiratory dystonia”. But the term most often used is “hyperventilation syndrome” (HVS) . It accounts for approximately 10% of cases. Among the patients there are both children and adults. It is worth noting that women suffer from this disease several times more often than men.
The causes of the syndrome are divided into mental, organic, and mixed. Of course, the majority (about 60%) is due to psychogenic factors.
5% of cases include organic etiology. These include disorders of the structure of the central nervous system: encephalopathy, hydrocephalus, inflammation of the meninges, as well as diseases such as diabetes, hypertension, chronic bronchitis. Sometimes the reason is taking certain medications.
During the course of the disease, there are 3 groups of signs:
- respiratory;
- psycho-emotional;
- muscular.
Group I has several forms of manifestations:
- Empty breathing is a feeling of lack of air, its pace quickens.
- It seems that air is forced into the lungs, and there is a lump in the throat. Accessory muscles are involved in the respiratory act.
- A premonition of breathing stopping appears, and the person is forced to control its process by consciously inhaling.
- Yawning, moaning, sighing.
Group II symptoms include nervous tension and concern about one’s condition. The patient cannot relax. He develops phobias, in particular, a fear of open areas and places with large crowds of people.
Symptomatic group III includes muscle hypertonicity, various tactile sensations in the form of tingling, burning, and “goosebumps.”
This triad of symptoms is a typical, leading manifestation of the disease.
The disease is characterized by a chronic course, in which exacerbations occur.
An exacerbation of hyperventilation syndrome is called a hyperventilation crisis. This is a condition in which the manifestations of the disease intensify. Characterized by an increased sense of fear. The patient is suffocating, hysterical, and feels “near death.” At the same time, he is accompanied by chills, dizziness, nausea, and becomes covered in sticky cold sweat.
A crisis is caused by a negative psychological environment. A unique way to relieve an attack is to breathe into a bag. In this case, carbon dioxide is concentrated in it, which the neurotic inhales. Gas balance is restored, breathing is leveled out. This is the first aid in this situation.
As for children, they are also characterized by such a pathology as respiratory neurosis, which is also caused by stress, phobias and anxiety disorders. But it is worth noting that the main role in their occurrence is played by an unfavorable situation in the family, and this applies not only to rude and inadequate attitude towards the child, but also to the relationship between parents. Constant quarrels and conflicts in the family, aggression can provoke the development of psychogenic shortness of breath in children.
Such children are characterized by anxiety and lability (instability) of mood. They experience outbursts of anger over trifles, general nervousness, refusal to communicate with friends, and sleep disturbances.
Parents should be more vigilant and sensitive in raising their children.
Options for shortness of breath after Covid-19
To date, doctors have described two types of difficulty breathing after coronavirus:
- Gradual. A person feels that he is breathing “insufficiently.” Difficulties with inhalation and exhalation occur even at rest. The situation gets worse at night. If the patient raises his hands up, he feels a little better. Worried about decreased performance.
- Sudden. At first the patient feels well, but at some point his body temperature rises, severe headache, and sweating occur. Full breathing becomes impossible. There is a panicky fear of dying from suffocation.
Both the first and second options require receiving qualified medical care. At the same time, you cannot hesitate, since even with mild symptoms, a moment may come when full breathing becomes impossible.
How to assess lung function after COVID-19
There is a no-false breath test that anyone can do on their own. According to its terms, it is necessary:
- Take a deep breath through your nose.
- Hold your breath for ten seconds.
- Exhale slowly.
If during testing no discomfort arises, a cough does not start, or a strong sore throat does not appear, then everything is fine with the lungs. If your health worsens when you try to hold in air, a medical examination is indicated.
Difficulties in self-diagnosis
Shortness of breath, which occurs due to narrowing of the nasal passages and swelling of the mucous membranes during a runny nose, and which manifests itself due to deterioration of the lungs - these are two completely different problems. A person is not able to independently understand what causes his illness.
Therefore, if you have difficulty breathing, you should still seek help from a therapist or pulmonologist. Self-medication for such symptoms is unacceptable.
How to treat shortness of breath after coronavirus
When helping people who have difficulty taking deep breaths, doctors use:
- drug therapy;
- oxygenation;
- inhalation;
- physiotherapy;
- breathing exercises.
Let's look at each method in more detail.
Medicines for shortness of breath
To improve pulmonary function, doctors prescribe drugs belonging to such pharmacological groups as:
- antiviral;
- immunomodulators;
- bronchodilators;
- expectorants;
- thinning phlegm;
- antibiotics.
Drugs and their dosages are always selected individually, taking into account the severity of the symptoms of the disease and the patient’s health status.
Oxygenation
It is inhaled oxygen therapy. Used if a person is unable to breathe on their own. Then oxygen is introduced directly into the respiratory tract through a special catheter.
Oxygenation is required only for seriously ill patients. If a person controls his condition and follows all medical prescriptions, the risk of sudden suffocation will be minimal.
Inhalations
During inhalation, a nebulizer is used, breaking the medicinal solution into tiny particles that easily penetrate into the deep tissues of the lungs. A good effect can be achieved by:
- agents that thin viscous sputum;
- antiseptics;
- sea water;
- saline solution;
- bronchodilators;
- coughing
Inhalations should not be carried out unless prescribed by a doctor, since if the inhaled drug is selected incorrectly, lung function may deteriorate.
Physiotherapeutic procedures
To speed up the resorption of inflammatory foci and abnormal compactions, during and after coronavirus, you need to do the following:
- massage of the chest area;
- UHF therapy;
- electrophoresis with enzyme solutions;
- SMT.
It is important to follow the physiotherapy course to the very end. If you abandon the procedures immediately after you feel better, the negative symptoms will most likely return again.
Breathing exercises
You should do breathing exercises during illness and for at least one month after receiving a negative test for COVID-19. They activate the muscles of the chest and increase blood flow to the lung tissues.
If a patient suffers from severe shortness of breath, the doctor may recommend using a respirometer, a device that measures the intensity in cells and tissues.
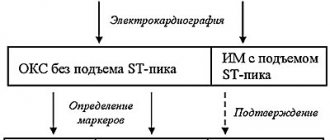
Diagnosis of chest pain
In order to make a correct diagnosis explaining the causes of pain, it is necessary:
- Consult a cardiologist
- Take a blood test - general and biochemical; in addition, it is necessary to check the blood for markers of myocardial infarction
- If you have a severe cough, you need to do a sputum test.
- Take an electrocardiogram
- If necessary, supplement with cardiac ultrasound examination
If you experience pain in the chest, you cannot make a diagnosis based on knowledge obtained from the Internet. It is necessary to consult a doctor who will identify the exact cause and prescribe adequate treatment.
Ways to improve lung function on your own
What can a person suffering from shortness of breath after coronavirus do? There are simple ways to normalize pulmonary activity:
- Eating foods that increase lung capacity. Preference should be given to fruits and vegetables. Tomatoes, blueberries, nuts, onions, and citrus fruits are especially useful. Spices and fatty foods should be avoided.
- No smoking. Tobacco smoke and the toxins it contains make the lungs extremely vulnerable. In order for the tissue to recover and the inflammatory process to stop progressing, it is important to stop smoking.
- Do cardio workouts. You need to start them only if you are in good physical health. Cardio increases lung capacity, normalizes blood circulation, and increases heart rate. It is good if the exercises are performed in the fresh air. But the load should be increased gradually.
- Respiratory protection from environmental pollution. A person who has recently had Covid-19 should not be in polluted conditions. If his professional activity involves being in harmful conditions, it is better to take a long vacation.
Patients who strictly follow the doctor's instructions, take medications, perform breathing exercises and eat properly quickly stop suffering from shortness of breath. Take care of your health and don't let the coronavirus deprive you of your ability to breathe deeply.
Relief from anxiety
Shortness of breath can cause feelings of fear. Some people say they feel anxious when they start to feel short of breath. However, anxiety can make breathing even more difficult.
Breathing exercises from this material can help you relax. You may also want to know other ways to help relieve anxiety. Talk to your doctor about any anxiety you have. He may prescribe anti-anxiety medications such as alprazolam (Xanax®) or lorazepam (Ativan®) to help you.
Our Integrative Medicine Service also offers relaxation programs that may be beneficial for you.
to come back to the beginning
Literature:
- COVID-19, coronavirus infection caused by SARS-CoV-2 / 2020 / ORGZDRAV: News. Opinions. Education. VSHOUZ Bulletin.
- COVID-19: respiratory infection caused by a new coronavirus: new data on epidemiology, clinical course, patient management.
- Medical rehabilitation for new coronavirus infection (Covid-19) / Ivanova G. E., Balandina I. N., Bakhtina I. S., Belkin A. A., Belyaev A. F., et al. / 2021 / Physical and rehabilitation medicine, medical rehabilitation
The text was checked by expert doctors: Head of the socio-psychological service of the Alkoklinik MC, psychologist Yu.P. Baranova, L.A. Serova, a psychiatrist-narcologist.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!
When to see a doctor?
In some cases, if shortness of breath and weakness occur, emergency medical attention is needed. An ambulance should be called in the following cases 2.7:
- severe sudden shortness of breath, accompanied by severe weakness, sweating;
- the appearance of sharp chest pain, palpitations, fainting, nausea;
- convulsions;
- impairment or complete loss of vision;
- speech disorder.
In other cases, a routine consultation with a general practitioner or family doctor is necessary to find out the cause of the ailment, conduct a diagnosis and begin correct treatment. To establish a diagnosis, the doctor may prescribe a number of examinations:
- laboratory tests - blood and urine tests;
- instrumental studies - ultrasound, sometimes MRI, CT.
If necessary, the doctor prescribes consultations with specialized specialists - a cardiologist, pulmonologist, hematologist, geneticist and others. Once the diagnosis is made, treatment is prescribed.
References
- Mukhambetova G. A. et al. Diagnostic criteria for Pompe disease // Bulletin of the Almaty State Institute for Advanced Medical Studies, 2013. No. 3.
- Shortness of breath. Mayo clinic. URL: https://www.mayoclinic.org/symptoms/shortness-of-breath/basics/causes/sym-20050890 (accessed 10/18/2019).
- Chikina S. Yu. Principles of assessing shortness of breath in the practice of a pulmonologist // Practical Pulmonology, 2006. No. 2.
- Avdeev S. N. Thromboembolism of the pulmonary arteries // Practical Pulmonology, 2009. No. 3.
- Carbon monoxide poisoning. MSD Handbook. URL: https://www.msdmanuals.com/ru/%D0%BF%D1%80%D0%BE%D1%84%D0%B5%D1%81%D1%81%D0%B8%D0%BE %D0%BD%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B9/%D1%82%D1%80%D0%B0%D0%B2%D0%BC% D1%8B-%D0%BE%D1%82%D1%80%D0%B0%D0%B2%D0%BB%D0%B5%D0%BD%D0%B8%D1%8F/%D0%BE% D1%82%D1%80%D0%B0%D0%B2%D0%BB%D0%B5%D0%BD%D0%B8%D1%8F/%D0%BE%D1%82%D1%80%D0 %B0%D0%B2%D0%BB%D0%B5%D0%BD%D0%B8%D0%B5-%D1%83%D0%B3%D0%B0%D1%80%D0%BD%D1% 8B%D0%BC-%D0%B3%D0%B0%D0%B7%D0%BE%D0%BC (accessed 10/24/2019).
- Federal clinical guidelines for the diagnosis and treatment of iron deficiency anemia, 2015.
- Stroke. Mayo clinic. URL: https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113 (accessed 10/24/2019).
GZEA.PD.18.09.0435t