The main focus of the study is the registration of the electrocardiogram of the heart (atria, His bundle, ventricles), and the use of diagnostic stimulation to assess the electrophysiological parameters of the heart. There are non-invasive and invasive cardiac EPI.
Transesophageal electrophysiological study (TEC cardiac EPS)
– a non-invasive method of electrophysiological examination of the heart, by introducing a diagnostic esophageal electrode through the nasopharynx (oropharynx) to a depth of 40-50 cm and recording an ECG. The examination is performed under local anesthesia (although more often without it) of the nasopharynx, the patient is in a supine position. The procedure usually does not require hospitalization. The study is performed on an outpatient basis (an EPI room or a cath lab) and usually takes no more than 20 minutes. Complications, as a rule, are not observed.
The essence of the method, advantages and disadvantages
The essence of an EFI examination of the heart is as follows:
- Typically, various heart rhythm disturbances or coronary heart disease can be determined based on a standard electrocardiogram.
- If arrhythmia or myocardial ischemia cannot be detected using a single ECG, the doctor prescribes 24-hour monitoring of blood pressure and Holter ECG. Under conditions of normal household activity, the indicated diseases can be registered in most cases during the day.
- If it is not possible to track them on the monitor, the patient performs exercise tests. As a rule, based on such tests (bicycle, treadmill, 6-minute walk test), an accurate diagnosis is established, since the heart is under conditions of increased stress, but increased naturally (walking, running).
- When the above methods do not reliably establish the diagnosis of arrhythmia or ischemia, and the patient still has cardiac complaints, he is prescribed EPI (electrophysiological study of the heart)
.
With EPI, the load on the heart also increases, but not as a result of physical activity, but as a result of electrical stimulation of the myocardium
.
Such stimulation is carried out using electrodes, which begin to supply electrical currents of physiological power to the heart muscle, but at a high frequency. As a result, the myocardium contracts faster, causing a provoked increase in heart rate. And at a high heart rate, either arrhythmia or ischemia occurs if a person already has pathological processes in the myocardium, which are prerequisites for the development of these diseases. In other words, EPI allows you to provoke the desired diseases and register them on an ECG for the purpose of further treatment of the patient.
But depending on how the electrodes are applied to the heart muscle, there are three types of techniques:
insertion of an electrode during transesophageal EPI
- Transesophageal EPI (TEPI)
.
The electrodes are supplied using a probe inserted into the lumen of the esophagus. It is a non-invasive technique, and its technique is similar to conventional fibrogastroscopy. Performed more often than the next two types of EFI. (We will not dwell on the technique of conducting PPE in this article in too much detail; there is a separate material about it). - Endocardial EPI (endoEPI)
. It is an invasive technique; electrodes are inserted into large vessels using a sterile probe and advanced under the control of X-ray equipment. Refers to high-tech types of medical care (HTMP). Despite the complexity of implementation, as well as the need to use high-quality personnel and expensive technical equipment, it is a very informative diagnostic method, and it identifies cardiac diseases better than TEE. - Epicardial EPI (epi-EPI)
. It is also an invasive technique when myocardial stimulation is performed during open-heart surgery with an incision into the chest (thoracotomy). In terms of information content, it is not inferior to endoEFI. Due to such a disadvantage as the need for thoracotomy, it is performed mainly during heart surgery for other diseases.
insertion of a catheter into the heart during invasive endoESI
Heart rhythm disturbances
At the National Medical Research Center of Sports Sciences named after. A.N. Bakulev diagnoses heart rhythm disturbances, as well as their effective elimination using modern minimally invasive treatment methods. The center uses modern high-tech equipment and methods for treating arrhythmias, including life-threatening ones.
Invasive arrhythmology does not involve open heart surgery, but interventional endovascular (through blood vessels) intervention. This method of treatment allows us to minimize the volume of intervention, reduce the operation time and, most importantly, the patient’s stay in the center’s hospital to 3-5 days.
The Department of X-ray Surgical Interventional Diagnostics and Treatment of Arrhythmias treats the entire spectrum of heart rhythm disturbances: NVT - supraventricular tachyarrhythmias (junctional tachycardia, pre-excitation syndrome (Wolf-Parkinson-White syndrome), atrial tachycardia, atrial extrasystoles, atrial flutter, atrial fibrillation; ventricular arrhythmias (ventricular extrasystoles of various locations, ventricular tachycardia), as well as disorders that arose after open heart surgery.
To eliminate areas of cardiac arrhythmia, not only radiofrequency and cryoablation are used, but also non-fluoroscopic navigation mapping with the construction of a three-dimensional model of the heart and obtaining an image of the source of arrhythmia in real time. Our center has unique experience in using all types of navigation systems from all leading manufacturers of electrophysiological equipment. The use of such equipment makes it possible to help patients with complex multi-stage correction of rhythm disturbances with concomitant organic heart pathologies with maximum efficiency.
For bradyarrhythmias and life-threatening cardiac arrhythmias, the center uses implantation of an artificial pacemaker (Electrocardiac pacemaker), thanks to which an adequate heart rate is normalized.
The list of bradyarrhythmias requiring pacemaker implantation includes:
- Atrioventricular (atrioventricular) blocks, both congenital and acquired;
- Sinoatrial blocks;
- Permanent form of atrial fibrillation with impaired atrioventricular conduction;
- Various manifestations of sick sinus syndrome.
In addition, implantation of a cardioverter-defibrillator is used to prevent sudden cardiac death and life-threatening conditions.
Arrhythmias requiring implantation of a cardioverter-defibrillator:
- Life-threatening ventricular tachycardia and ventricular fibrillation;
- Risk of sudden death in patients with coronary heart disease;
- Genetic ventricular arrhythmias.
Resynchronization devices and cardiac contractility modulation devices (Optimizer) are also widely used to treat chronic heart failure.
In the clinic of the National Medical Research Center for Cardiovascular Surgery named after. A.N. Bakulev regularly tests all types of implantable devices for electrical pacing.
When is EPI indicated?
Any type of EPI is carried out if the patient has certain complaints that the doctor cannot associate with disorders identified by the ECG or which arise in the patient with satisfactory examination results, or when certain diseases are suspected.
Thus, invasive cardiac EPI is performed when symptoms of the following nature occur:
- Paroxysmal interruptions in the work of the heart, especially short-term, but causing significant subjective discomfort,
- Interruptions in the heart, accompanied by severe general poor health, as well as shortness of breath and wheezing in the chest at rest, blue discoloration of the nasolabial triangle or the skin of other parts of the body (cyanosis), severe pallor of the skin, very high or low blood pressure, intense pain in the chest or in the chest on the left,
- Loss of consciousness and presyncope, with the exception of pathology of the central nervous system or other diseases (in the case of cardiac causes, loss of consciousness is called an attack or the equivalent of a Morgagni-Adams-Stokes attack, an attack of MES),
- Episodes of cardiac arrest (asystole) leading to clinical death with successful resuscitation of the patient.
Among the diseases that require invasive cardiac electrophysiology to clarify the diagnosis, the following can be noted:
- Paroxysmal types of arrhythmias - atrial fibrillation-flutter, supraventricular tachyarrhythmia, frequent ventricular extrasystole with transition to ventricular tachycardia,
- Sick sinus syndrome (SSNS), accompanied by alternating tachy- and bradycardia (tachy-brady syndrome), as well as bradycardia with the above-mentioned attacks of MES,
- Ventricular fibrillation with transition to asystole,
- Cardiac ischemia.
In the case where TEE does not help to reliably establish or exclude a diagnosis, that is, in diagnostically unclear cases, the patient undergoes endo- or epi-EPI.
In addition, endoEPI is carried out as part of an intraoperative examination when performing an intravascular RFA (radiofrequency ablation) operation, in which the pathological paths of the impulse that are the cause of one or another type of arrhythmia are destroyed by an intracardiac probe.
Radiofrequency catheter ablation of cardiac conduction tracts for tachyarrhythmias
Radiofrequency ablation (destruction) of cardiac conduction pathways is a minimally invasive method of radical treatment of tachycardia. A fairly young and effective method of minimally invasive treatment of tachycardia. This method is based on a local (point) effect of high-frequency electric current on the “center” of arrhythmia or a section of the circuit of circular motion of the pulse during tachycardias.
Symptoms (manifestations) of the disease:
- interruptions in heart function,
- attacks of tachycardia,
- episodes of weakness, dizziness, chest pain during an attack,
- loss of consciousness due to an attack
It is very important when a patient comes to the hospital for a consultation with a cardiac surgeon-arrhythmologist, the patient has an electrocardiogram with an attack of tachycardia, or an attack registered on the 24-hour electrocardiogram monitor.
To carry out the intervention, patients are hospitalized in the cardiology department of the hospital of St. Petersburg State Budgetary Healthcare Institution GB No. 40, before the operation it is necessary to perform a series of examinations and pass a list of necessary tests.
The operation is performed in an X-ray operating room (Department of X-ray endovascular diagnostics and treatment; Head: Candidate of Medical Sciences S.V. Vlasenko) under the constant supervision of an anesthesiologist and monitoring of blood pressure and electrocardiogram.
The procedure is performed by experienced x-ray surgeons-arrhythmologists A.V. Kamenev, Ph.D., A.M. Osadchim, electrophysiologists Ph.D., T.A. Lyubimtseva, M.A. Vander. The group works under the guidance of prof. RAS D.S. Lebedeva.
Procedure (operation) of catheter ablation for tachycardia.
Radiofrequency ablation usually does not require general anesthesia (anesthesia).
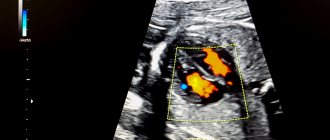
Immediately before ablation, an invasive electrophysiological study of the heart is performed to determine the mechanism of arrhythmia formation and its localization. It is carried out using diagnostic catheter-electrodes inserted through large veins (femoral, subclavian) or arteries, which make it possible to accurately determine the location of the “pathological focus” of arrhythmia.
Previously, under local anesthesia (“freezing”), hemostatic introducers (“tubes”) are introduced into these large vessels, which help protect the vessel.
Then, using a special “ablation” electrode, a search is carried out (“mapping” using the modern Carto 3 navigation system; Fig. 1.) and “cauterization” of the source of arrhythmia.
The electrodes are delivered to the heart and the procedure is performed under fluoroscopic control (Fig. 2).
The operation lasts from 45 to 150 minutes and it all depends on the location of the source of arrhythmia, quick search and its depth. As a rule, on the 1st-2nd day after surgery the patient can be discharged from the hospital.
| Figure 1. RFA of the focus of ventricular tachycardia during an electrical storm | Figure 2. Rg-freeze frame when performing RFA of a VT focus in the LV, transseptal approach |
Radiofrequency ablation of the arrhythmogenic zone can radically cure:
- Paroxysmal atrioventricular-nodal re-entry tachycardia.
- Paroxysmal atrioventricular reentrant tachycardia involving an accessory pathway (WPW syndrome).
- Paroxysmal form of typical atrial flutter.
- Paroxysmal form of atrial fibrillation (AF) with no effect from antiarrhythmic therapy (efficacy up to 92%).
- Persistent tachysystolic AF with ineffectiveness of drug therapy (the effectiveness of the first procedure is up to 67%).
- Paroxysmal atrial tachycardia.
- Ventricular monomorphic (from one focus) tachycardia.
- Ventricular monomoral extrasystole with clinical symptoms (frequent, more than 7-10 thousand/day).
Contraindications for catheter ablation for tachycardia:
- acute infectious diseases,
- acute myocardial infarction,
- unstable angina for 4 weeks,
- chronic heart failure III-IV f.k. according to NYHA,
- left ventricular aneurysm with thrombus,
- blood clots in the cavities of the heart,
- cardiac mechanical prostheses of the left chambers of the heart with access from the left.
When performing catheter ablation for arrhythmias, the rate of complications does not exceed 1%. In order to prevent the latter, all necessary measures are taken at all stages of diagnosis and treatment.
The advantages of this method are that it is minimally invasive (low-traumatic), as a rule, hospitalization does not take more than 3 days, patients quickly resume their normal lifestyle and rehabilitation does not take more than a week. Operations are performed under a quota (VMP) (for residents of St. Petersburg) and modern equipment and expensive consumables are used to perform them within the framework of funding from the federal budget.
| Radiologist consultations are carried out: on Wednesdays from 17:00 to 19:00, arrhythmologist on Thursdays from 15:00 to 17:00 in the rehabilitation building, 4th floor, room 424. Make an appointment with specialists by calling 200-16-88. Osadchiy Andrey Mikhailovich (surgeon-arrhythmologist) +7 (911) 126-36-64; Decoration in room No. 340 of clinic No. 68, third floor. Bring with you a referral for consultation from the clinic, a compulsory medical insurance policy, a passport and SNILS. If available, have medical documentation (early discharge notes, EchoCG, 24-hour ECG monitor, ECG with arrhythmia). |
← Back
In what cases is EPI contraindicated?
Advertising:
Any type of cardiac EPI has a number of contraindications. These include the following:
- The patient develops an acute heart attack or stroke,
- The occurrence of fever, acute infectious disease,
- Unstable angina (new or progressive),
- Suspicion of pulmonary embolism (PE),
- Acute surgical pathology,
- Severe decompensation of chronic diseases (diabetes mellitus, bronchial asthma),
- Development of acute heart failure (cardiac asthma, pulmonary edema), or severe decompensation of chronic heart failure,
- Decompensated heart defects,
- Stage III of chronic heart failure,
- Severe dilated cardiomyopathy with low ejection fraction (less than 20=30%).
TEE (transesophageal examination of the cardiac conduction system)
If you experience sudden attacks of rapid heartbeat, which immediately knock you out of your usual life rut, require you to freeze, stop, hold your breath, take medicine, and sometimes even call an ambulance; if the heart beats unevenly – “freezes”, “tumbles”, “quivers”; if sudden dizziness or even loss of consciousness sometimes occurs, you need to contact a cardiologist-arrhythmologist who will prescribe examinations. Among them may be the well-known ECG, ultrasound of the heart - EchoCG, 24-hour ECG-Holter monitor, ultrasound of the thyroid gland, but in some cases, to make a diagnosis it is impossible to do without a specific study of the conduction system of the heart - TEE (transesophageal examination of the conduction system of the heart).
ChPEFI at the Medservice clinic
Transesophageal examination of the cardiac conduction system - TEE - is carried out by a cardiologist. The patient lies on the couch, electrodes are applied to the arms and legs (as when taking an ECG). The esophageal electrode (it is small, 2 mm in diameter) is inserted through the nose into the esophagus and placed next to the heart. He takes a special ECG, on which all the waves are registered more clearly. The strength and amplitude of the impact is selected, effective for the study and painless for the patient. Various stimulation programs determine the operating parameters of the main centers that set the heart rhythm.
An electrocardiograph “Vector” (Nizhny Novgorod) is used for the study. The program for processing research data has been updated in 2021.
The experience of conducting this study in the clinic is 10 years. We try to reduce the time of the procedure itself as much as possible and obtain complete information about your heart.
Indications
Indications for performing TPE are:
- sinus bradycardia, pauses in heart function;
- attacks of sudden palpitations;
- fainting of unknown cause;
- identification of additional pathways in the heart;
- assessment of the effectiveness of the operation performed - ablation of additional pathways of the heart;
- assessment of the effectiveness of medications taken to prevent arrhythmia;
Contraindications
The procedure has a number of contraindications, if present, another diagnostic method should be chosen. Contraindications for TEE are:
- acute damage to the heart muscle - heart attack, myocarditis, pericarditis;
- acute and chronic heart failure;
- life-threatening heart rhythm disturbances detected by other research methods (if necessary, the procedure is carried out in a hospital setting);
- damage, diseases of the esophagus;
- pronounced gag reflex
Preparing for research
In preparation for the study, it is necessary to stop taking antiarrhythmic drugs 5 days before, and before the procedure, fast for 3 hours.
Before the procedure, the doctor will talk with you, look at all the results of examinations done earlier and determine the need and possibility of conducting the study.
Sometimes during the study it is not possible to obtain complete information about the causes of cardiac dysfunction. Then a drug test is used - intravenous administration of atropine. The drug begins to act within 1-2 minutes from the moment of administration and continues for 20-30 minutes. The same indicators are determined again as in the original test. This makes it possible to distinguish pathological changes found during the study from changes that are acceptable as a variant of the norm.
Research results
After completing the diagnosis, the patient is given a transcript of the procedure result with a detailed explanation and recommendations from the doctor.
How to prepare for the procedure?
Advertising:
All nuances of preparation for the study must be carefully explained by the doctor to the patient. Firstly, the patient (under the supervision and as directed by a doctor!) must stop taking any antiarrhythmic drugs, as they can distort the results of the study. Secondly, before the TPE procedure, a patient experiencing even slight discomfort from the stomach must undergo fibrogastroscopy in order to exclude acute gastroesophageal pathology.
Before the endoEPI procedure for attacks of loss of consciousness, a neurologist must exclude brain pathology that could cause fainting, and this may require a CT scan or MRI of the skull.
Due to the fact that endo- or epi-EPI requires hospitalization in a hospital, a patient undergoing a routine examination must provide the doctor with the results of tests for HIV, syphilis, hepatitis and blood clotting no later than two weeks ago (different institutions have their own deadlines) .
The study is carried out strictly on an empty stomach. The need for epi-EPI on an empty stomach is due to the fact that during general anesthesia, vomiting of eaten food or liquid and aspiration of vomit may occur.
After the necessary preparation, the patient is hospitalized in a hospital. He must have the results of the examination (ultrasound of the heart, 24-hour monitor), as well as an extract from the outpatient card or discharge summary from the institution where he received examination and treatment before. The extract must indicate the rationale for the need for EFI with a detailed clinical diagnosis.
Carrying out EPI of the heart
Advertising:
Due to the fact that the essence of electrical stimulation of the myocardium is the same for all three methods, and TPEPI is similar in technique to FEGDS, it makes sense to dwell in more detail on invasive EPI methods.
So, invasive endoEPI
is carried out in the department of x-ray and surgical diagnostic methods, while the patient is undergoing inpatient treatment in the cardiology, cardioarrhythmology or cardiac surgery department.
After a little preparation in the form of intravenous administration of sedatives, the patient is transported on a recumbent gurney to the X-ray surgery. The doctor conducting the examination, under conditions of complete sterility, accesses the femoral (less often the subclavian) vein under local anesthesia. A small incision is made in the vein in the most favorable place for the technique (called venesection).
Next, through the resulting incision, a thin plastic or metal conductor called an introducer is inserted into the patient's vein. A probe with electrodes at the end, which has X-ray contrast properties and is therefore visible on the screen, is passed along it. After the probe gradually moves through the vein to the right atrium, controlled on the screen, and the probe reaches the chamber of the heart (atrium or ventricle) necessary for examination, the myocardium is stimulated in a physiological mode.
The probe typically has three to five miniature electrodes that are connected to a device that can switch their operation from stimulation mode to recording mode, and vice versa. The resulting cardiograms are recorded using a computer device.
example of electrode placement for EndoEPI
The duration of the procedure is half an hour or more, without causing significant pain. The patient remains conscious throughout the operation. After removing the probe, a pressure aseptic bandage will be applied to the skin in the venesection area.
EpiEPI
carried out in the department of cardiac surgery. After putting the patient into a medicated sleep (general anesthesia), the chest is dissected with access to the pericardial cavity. The issue of using a heart-lung machine (ACB) is decided strictly individually. After exposing the inner layer of the outer layer of the heart (epicardium), electrodes are applied to it, and stimulation begins with simultaneous recording of the response received from the heart muscle. The study takes more than an hour. After all the necessary manipulations have been carried out, the wound is sutured layer by layer, and drainage remains in the pleural cavity and is removed on the 2-3rd day.
After any of the invasive EPI methods, the patient remains under observation in the intensive care unit for a period of one day or more, depending on the severity of the patient’s condition.
Electrophysiological study of the heart - EPS
Contraindications
This type of research is strictly prohibited under the following circumstances:
- acute infectious disease or simply the presence of fever;
- heart attack or stroke in the acute stage;
- severe angina that occurs for the first time and progresses;
- in acute surgical pathology;
- in severe chronic heart failure or in its acute form;
- the presence of certain types of heart defects;
- if there is a suspicion of pulmonary embolism;
- diseases of the esophagus;
- the presence of cardiac or aortic aneurysms.
Proper preparation for the procedure
To undergo this procedure, the patient is referred after a complete examination by a cardiologist, arrhythmologist or cardiac surgeon. Before performing EPI, the attending physician conducts the following studies:
The patient will first of all have to carry tests for HIV, hepatitis, syphilis and blood clotting. These tests are necessary, since diagnosis using the electrophysiological study method will take place in a hospital, and the patient will have to be hospitalized.
- MRI or CT, these examinations are especially necessary if the patient experiences fainting, the doctor excludes the presence of brain pathologies;
- Ultrasound of the heart;
- 24-hour Holter monitoring;
- discharge summary with justification for the need for this procedure.
In addition, the patient himself must prepare for the upcoming examination. To do this he will need:
- fast for 8 – 10 hours;
- within a few days, stop drinking caffeine, alcohol and cigarettes;
- The doctor will stop the use of any medications.
Progress of the procedure
Considering that there are two types of research - invasive and non-invasive, there will be two ways to carry out the procedure.
Methodology for non-invasive EPI
The most commonly used non-invasive examination method, in which a catheter with an electrode is inserted through the nose or mouth, which is used somewhat less frequently. This method is also called transesophageal EPI or TEE. It is carried out in functional diagnostic departments, usually in the morning. The examination takes place as follows:
- Preliminary blood pressure measurement.
- Taking an ECG.
- The doctor explains the procedures and specifies what the patient will experience during the examination. There is usually a burning sensation in the chest, and this is normal.
- All manipulations usually take about half an hour.
- Through the nasal opening or, in rare cases, through the mouth, the doctor inserts a probe with an electrode into the patient, which is connected to special devices. Using equipment, stimulation of the heart muscle is carried out with electrical impulses. During this procedure, the heart begins to contract vigorously, as if under increased stress. All received data is recorded.
- An electrogram is recorded.
- The doctor carefully removes the catheter.
- A complete analysis of the collected information is carried out and a conclusion is made, which is sent to the attending physician.
- The tachycardia caused by the procedure will go away after some time, but if the discomfort continues for a long time, the doctor can provide medication.
Method of performing invasive EPI
In cases where TEE does not produce results or for some reason it is contraindicated, the doctor will prescribe endocardial or epicardial EPI.
Endocardial EPI
Before the procedure, the patient is placed in the department of cardiology, cardiac surgery or cardiac arrhythmology. EndoEPI itself is done in the department of X-ray surgical diagnostic methods. The patient is given an antisedative and taken to the operating room. Local anesthesia is performed. In complete sterility, the doctor makes an incision to insert a catheter into the femoral or subclavian vein. An introducer (metal or plastic guide) is inserted into the incision. A probe with an electrode is passed through it. The passage of the probe is observed on the screen. This is possible due to the available contrast agent. The probe is passed to the atrium or ventricle. The doctor performs electrical stimulation. All data is recorded using a computer.
This entire medical procedure lasts approximately half an hour. The patient should feel absolutely no discomfort. After removing the probe, apply a tight bandage to the insertion site.
Epicardial EPI
This study is carried out in the cardiac surgery department. The entire operation is performed under general anesthesia. The doctor dissects the chest and gains access to the pericardial cavity. Using electrodes, the doctor stimulates the epicardium. All data is recorded and then the wound is sutured. Typically, the operation lasts about an hour and is the most difficult area of examination using the EPI method.
Are there any complications?
Advertising:
As with any invasive research method, complications of endo- and epi-EPI are possible, but they occur in extremely rare cases. The main types of adverse consequences are cardiac acute conditions provoked by artificially created tachycardia. These include:
- Angina attack
- Development of acute myocardial infarction,
- Thromboembolic complications caused by the entry of a blood clot that has broken away from the heart cavity, if the latter was not identified before the procedure using echocardiography (ultrasound of the heart).
Prevention of this kind of complications is a thorough examination of the patient before surgery, as well as competent determination of indications for examination.
In the postoperative period, there is an extremely low probability of developing inflammatory and thromboembolic complications, as well as the occurrence of life-threatening arrhythmias.
Decoding the results
Advertising:
Interpretation of the results is carried out by the doctor performing the study and the attending physician who referred the patient for the procedure.
Normally, the electrogram obtained during EPI reveals sinus tachycardia with a heart rate of 100 to 120 per minute or more. Such tachycardia is transient and is not dangerous for the patient.
example of EFI results
If the study protocol contains the phrase that no rhythm disturbances were achieved using all types of stimulation, it means that the patient does not have a suspected type of arrhythmia, and the EPS results are regarded as normal. Also, normally there should be no depression or elevation of the ST segment and negative T waves, indicating myocardial ischemia.
If such changes are detected, their location is indicated, as well as the type of electrical stimulation in which they occurred.
When an arrhythmia is detected, its type is indicated (atrial fibrillation, ventricular tachycardia, frequent ventricular extrasystole, etc.), and the stimulation parameters that caused the rhythm disturbance.
Any of the disorders recorded on the electrogram requires careful medical supervision due to the need to prescribe certain antiarrhythmic drugs or perform RFA.
Carrying out, based on the results of EFI, RFA – “cauterization” of the area of pathological electrical activity of the heart
Approximate cost of EFI
Cardiac EPI can be performed in any large medical institution that has the appropriate personnel and technical equipment. Typically, EFI is carried out in regional or district centers, as well as in city hospitals in large cities (Moscow, St. Petersburg, Tyumen, Chelyabinsk, etc.).
Typically, EPI of the heart is carried out according to a quota from the Ministry of Health using funds from the federal budget. However, if the patient can pay for the procedure on his own, then there is no need to wait several weeks, since EFI can be performed for paid services.
Prices for cardiac electrophysiology testing vary widely. Thus, the cost of PPE is from 2000 to 4000 rubles, depending on the institution and equipment. The cost of endoEPI is much higher and amounts to 60-180 thousand rubles, depending on the payment for the probe and catheters, as well as the payment for the subsequent stay in the clinic.