© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
Transesophageal electrophysiological study (TEPE) is a technique for studying cardiac contractility and heart rhythm by applying physiological doses of electric current to the area of the heart most closely adjacent to the esophagus.
For the first time, the PPE technique began to be widely introduced into practice by arrhythmologists in the 70-80s of the last century. The study is otherwise called a non-invasive electrophysiological study, as opposed to an invasive one, in which electrodes are usually inserted through large arteries directly into the heart cavity from the inside. A little later, TEE began to be actively used in pediatrics, significantly expanding diagnostic capabilities in arrhythmology.
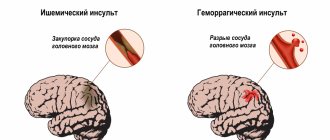
The essence of the method is based on the anatomical proximity of the esophagus and the heart. Often, in many patients, heart rhythm disturbances (arrhythmias) cannot be detected using a standard ECG or even with 24-hour blood pressure and ECG monitoring. Then stimulation of the heart muscle is applied, and if the patient has an arrhythmia, this will manifest itself during TEE. In other words, in some cases the myocardium must be “provoked” in order to understand whether electrical impulses are carried out correctly or whether there is a rhythm disturbance.
Using an electrode inserted through the esophagus, impulses are sent to the heart muscle, and electrodes placed on the chest record the rhythm during the study.
In addition, the rapid heart rate that occurs due to electrical stimulation can cause episodes of myocardial ischemia in patients suffering from coronary heart disease that is not detected on a standard ECG.
In addition to transesophageal EPI, there are invasive methods:
insertion of electrodes into the heart during invasive catheter EPI
- With endocardial EPI, a catheter with an electrode is delivered through the femoral vein into the ventricle or atrium, and the diagnostic procedure is often combined with subsequent RFA of pathological areas of the myocardium.
- EPI is also performed through open access (during cardiac surgery). Stimulation occurs epicardially - from the “outer” surface of the heart.
The essence of invasive procedures is generally similar to transesophageal procedures. Naturally, such interventions are correspondingly traumatic, but can be more effective.
Advantages and disadvantages of PPEFI
The undoubted advantage of this technique is a more accurate diagnosis of rhythm disturbances, especially short runs of supraventricular tachycardia . What is meant here is local diagnostics, that is, with the help of TEE, in 90-100% of cases (according to various studies), it is possible to establish the exact place in the conduction system of the heart in which conditions exist for the occurrence of tachycardia or, conversely, for blocking the propagation of an impulse through the heart . Both rhythm disturbances can be life-threatening (depending on the type of arrhythmia), so identifying them using TEE can save the patient’s life and health.
The method has no disadvantages (besides the patient’s sensations), and other advantages include low trauma, non-invasiveness, the possibility of repeating the study, and the accessibility of the method to the general population.
Research results
A test is considered normal if, when exposed to impulses supplied through the esophageal electrode, no rhythm disturbances are detected. If complaints of rapid heartbeat or attacks of loss of consciousness remain, and TPEFI is negative, then it is either repeated after 1 - 2 weeks, or an electrophysiological study is performed with an electrode inserted through the vascular network.
When rhythm disturbances are detected, its properties are recorded:
- type of arrhythmia,
- duration,
- appearance time,
- characteristics of electrical signals.
Example of PPEFI results
Indications for electrophysiological examination of the heart
The main indications are various rhythm disturbances. Thus, performing TEE is justified in diagnostically unclear cases when the doctor suspects the patient:
- Paroxysmal tachycardia - atrial or supraventricular,
- Paroxysmal atrial fibrillation,
- Bradyarrhythmia, accompanied by a heart rate of less than 50 per minute, for example, with sick sinus syndrome, with atrioventricular block, etc.
- Tachycardia with SVC syndrome (Wolf-Parkinson-White syndrome) or KLK syndrome (Clerk-Levi-Christesco) - paroxysmal types of tachycardia when the atria contract at a high frequency (more than 100 per minute), and due to the presence of additional conduction pathways between the atria and ventricles (Kent and James bundles), tachycardia can spread to the ventricles, which poses a threat to the patient’s life.
In some cases, the study is performed when diagnosing coronary heart disease, for example, in patients in whom it is not possible to register episodes of myocardial ischemia using an ECG or 24-hour monitoring. In addition, TEE helps in diagnosing ischemia in the presence of contraindications for testing with physical activity, for example, in the presence of severe deforming osteoarthritis or other osteoarticular pathology.
In addition to direct diagnosis of diseases, repeat TEE is performed to monitor drug treatment of arrhythmias or after surgery, for example, after radiofrequency ablation (RFA). TEE is also performed before installing an artificial pacemaker.
Assessment of coronary circulation using the TEES method
This stimulation program is the basis from which the TEES method began as one of the stress tests (rhythm load) in cardiology.
The use of a stimulation program allows you to gradually and dosedly increase the frequency of ventricular contractions with constant assessment of changes in the final part of the ventricular complex on the monitor and when recording an ECG.
The use of TEES to assess coronary circulation allows the cardiologist to solve a number of important problems:
1. establish the very fact that the patient has coronary heart disease (CHD) and its forms, in particular, determine painless myocardial ischemia; 2. determine the degree of coronary insufficiency; 3. determine the optimal effective dose of the antianginal drug and the frequency of its administration; 4. to identify a group of patients with coronary heart disease with severe coronary insufficiency, for whom coronary angiography and possible surgical treatment of coronary artery disease are strongly recommended; 5. determine the prognosis and management tactics for patients with coronary artery disease after myocardial infarction; 6. identify a group of patients with coronary artery disease who have a high risk of sudden cardiac death for the purpose of preventive treatment; 7. carry out differential diagnosis of post-infarction cardiosclerosis in patients with Wolff-Parkinson-White syndrome; 8. identification of hidden forms of rhythm and conduction disorders; 9. when dynamically performing TES in the same patient with coronary artery disease, indirectly judge the rate of progression of coronary atherosclerosis and the effectiveness of the treatment.
In addition to general contraindications, performing TES according to the coronary circulation assessment program is not advisable in the following cases:
1. in the presence of persistent complete blockade of the left bundle branch; 2. when recording an obvious (manifesting) syndrome of premature excitation of the ventricles caused by the functioning of the Kent bundle on a resting ECG; 3. a patient with coronary artery disease with 3-4 functional class; 4. in a patient with new-onset angina during the first 4 weeks and in a patient with unstable angina; 5. during the first 3 weeks of uncomplicated myocardial infarction; 6. with pronounced hypertrophy of the left ventricular myocardium with secondary changes in the final part of the ventricular complex on the ECG. TEES is carried out as prescribed by the attending physician 2 hours after a meal against the background of withdrawal of coronary drugs in the case of a diagnostic study. In this case, the patient’s consent to perform TES, recording a resting ECG and echocardiogram (EchoCG) is required.
The stimulation program for the purpose of assessing coronary circulation is quite simple. After obtaining a stable pacemaker rhythm that exceeds the natural heart rate by 20 pulses/min, continuous stepwise stimulation is performed. The duration of each stage is 1 minute.
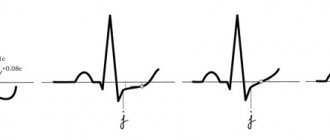
If there are no changes at the end of the step, the stimulation frequency is increased by 10-20 pulses/min. until a maximum frequency of 160 pulses/min is reached. After each stage of stimulation, the coronary circulation is assessed by changes in the ST segment on the ECG.
If, after reaching the maximum frequency (160 pulses/min.), no ischemic changes are observed on the ECG, then the stimulation time is extended to 2 minutes, after which a final assessment of the study is carried out. It is considered inappropriate to assess coronary circulation at a stimulation frequency of more than 160 pulses/min. at the same time, the number of false-positive results increases significantly, which is partly due to the so-called post-depolarization syndrome.
Post-depolarization syndrome is expressed in the occurrence of ST segment depression and T wave inversion on the ECG after the cessation of high ventricular frequency. The development of this syndrome after relief of paroxysm of ventricular tachycardia is well known.
In the absence of verified coronary artery disease in a patient, this syndrome indicates disturbances in the processes of ventricular repolarization not associated with deterioration of coronary circulation.
to the top of the page
What symptoms may indicate the need for TEE?
Rhythm disturbances requiring transesophageal pacing can be suspected based on the presence of the following signs in the patient:
- Attacks of sudden rapid heartbeat with rapid pulse (more than 100-120 per minute), also suddenly stopping spontaneously or stopping only after the administration of antiarrhythmic drugs,
- Feelings of irregular heartbeat with a rare pulse (less than 50 per minute),
- Attacks of loss of consciousness that are not associated with neurological problems or with situationally occurring conditions (stuffiness in the room, stress, etc.), but are caused by rhythm disturbances and are called Morgagni-Edams-Stokes attacks (MES episodes).
If a doctor, while examining a patient, hears about the presence of the symptoms described above, then he should think about a more accurate diagnosis of heart rhythm disturbances. And if the ECG and 24-hour monitor do not reveal any types of arrhythmias, and the patient’s complaints persist, it is necessary to perform TEE. If it was possible to register an arrhythmia on the ECG, for example, a delta wave, characteristic of latent SVC syndrome, the patient should be further examined.
In any case, the need for this technique is determined only by a doctor during an in-person examination of the patient.
1.General information
Electrocardiostimulation (ECS) – conduction of additional, external electrical impulses to the heart muscle. As is known, the rhythmic contractile activity of the myocardium is controlled and controlled in the body by a bioelectrical method, which has made it possible to develop a number of well-known diagnostic, therapeutic and resuscitation methods built precisely on electrophysiological principles.
Modern high-tech pacemakers, implanted inside and designed for long-term automatic operation, are equipped with a microprocessor controller that records the main indicators of the electrical activity of the heart and connects additional stimulating discharges only if necessary.
Transesophageal cardiac pacing is one of the non-invasive modifications of the pacemaker method, which is used both for diagnostic purposes and for the relief of certain dangerous conditions.
A must read! Help with treatment and hospitalization!
Contraindications
Regarding electrical stimulation of the heart, contraindications include the presence of obvious disturbances in heart rhythm and conduction detected on the electrocardiogram. Thus, the impact of impulses on the heart muscle is contraindicated in the case of atrioventricular block of 2 and 3 degrees, as well as in the presence of existing atrial fibrillation-flutter.
In addition, an absolute contraindication is the presence of a blood clot in the atrial cavity, identified by the results of an ultrasound of the heart, since rapid heartbeat at the time of the study can lead to the separation and spread of the blood clot through the bloodstream.
Regarding the insertion of a probe into the lumen of the esophagus, contraindications are the presence of tumors in the patient, strictures (adhesions) of the esophagus, scar narrowing of the esophagus and an inflammatory process - esophagitis.
Transesophageal electrophysiological examination is also contraindicated in the presence of acute infectious processes in the body, fever and severe mental disorders in the patient.
Application of TEES for cardiac arrhythmias
The use of TEES for cardiac arrhythmias was justified as a result of the rapid development of arrhythmology and based on its problems.
The use of TEES in this category of patients solved many problems of supraventricular arrhythmias and fully replaced such a research method as intracardiac electrophysiological study (EPS).
Therefore, indications for EPI are currently narrowed and can be determined by the following conditions:
1 Clarification of the diagnosis and selection of therapy for patients with ventricular tachycardia. 2. Syncope, unknown etiology. 3. Before surgical treatment of arrhythmias. 4. Before implantation of a pacemaker or cardioverter-defibrillator in patients with tachyarrhythmias. 5. To carry out cryodestruction of abnormal conduction pathways in case of their right-sided passage. 6. Patients with WPW syndrome and paroxysmal atrial fibrillation, which occurs with loss of consciousness and the threat of transformation into ventricular fibrillation.
Rice. Transesophageal electrogram, bipolar recording
When starting a study on the rhythm disturbance program using the TEES method, the doctor conducting it must be sure that everything is prepared in case of resuscitation measures: the defibrillator is prepared and turned on, there is the necessary set of resuscitation drugs and supplies.
In addition, the doctor conducting the study must be well trained in such disciplines as clinical cardiology with arrhythmology, clinical electrocardiography, know the electrophysiology of the myocardium, issues of emergency cardiology and resuscitation.
It should be especially emphasized that the study of PPES according to the program for cardiac arrhythmias must be carried out in the presence of at least two medical workers - a doctor and a nurse who have undergone special training.
TEES can be performed for diagnostic and therapeutic purposes. In the event of a diagnostic study, all antiarrhythmic drugs should be discontinued.
Rice. A. Paired stimulation of the atria causes paroxysm of AV reciprocal orthodromic tachycardia. The RP'-interval on TEE is less than 1/2 the RR-interval and = 120 ms. B. Relief of paroxysm by paired stimulation.
to the top of the page
How to prepare for the procedure?
The patient must prepare for the study as follows:
- Stop taking prescribed antiarrhythmic drugs no later than a week before the test, but only in agreement with the doctor who referred you for TPE,
- Of the prescribed drugs, it is permissible to use only short-acting nitroglycerin under the tongue for angina attacks,
- A few weeks or days before the examination, perform an ECG, ultrasound of the heart and 24-hour monitoring of blood pressure and ECG,
- It is advisable not to smoke or drink alcohol during the week before the procedure.
- On the eve of the study, a light dinner is allowed, it is advisable to exclude coffee,
- On the day of the study, the patient must appear for the procedure on a completely empty stomach, even drinking water is excluded.
Possible complications
Most patients tolerate the examination well, as this technique is safe. But you still need to consider the possibility of the following complications:
- hypersensitivity to the anesthetic solution (swelling, laryngeal spasm, anaphylactic reaction, up to shock), therefore, if you are prone to allergies, tests are carried out first;
- myocardial infarction;
- attack of rhythm disturbance;
- pulmonary embolism;
- pain in the heart like angina pectoris.
To prevent such situations, it is necessary to undergo a complete cardiac examination before TEE..
Reasons why you shouldn't put off getting a heart exam
How is the procedure performed?
TPEFI can be performed in a clinic or in a hospital, depending on the personnel and technical equipment of the institution. Typically, such techniques are carried out in the department of functional diagnostics.
equipment for CPEFI (photo: doktora.by)
At the appointed time, after pre-registration, the patient visits this department. In the TPE room, he is placed on a couch, and after preliminary measurement of blood pressure and recording of a standard ECG, the procedure begins. To do this, the doctor treats the root of the tongue with a solution of a local anesthetic - lidocaine or dicaine to reduce discomfort when inserting the probe.
The probe used is thin and sterile, and is most often inserted through the nasopharynx, in some cases through the mouth. This procedure at this stage is no more unpleasant than examining the stomach during fibrogastroscopy. The probe contains an electrode as a tip that will send signals to the heart muscle. Electrodes that read the electrical activity of the heart are placed on the chest wall, similar to a regular ECG.
The probe is placed approximately 30-35 cm from the nasopharynx, and signals begin to be sent to the heart. During this time, the patient may experience a rapid heartbeat or a burning sensation in the chest, and such sensations are normal. At the same time, an ECG is recorded using electrodes on the chest.
probe and TEE
After the end of stimulation, the doctor interprets the results and draws up his conclusion in the form of a protocol, which the patient must provide to the treating arrhythmologist or cardiologist. The entire procedure takes no more than 40 minutes and does not cause significant pain in the patient.
Complications during TEES
It should be noted right away that paroxysmal rhythm disturbances, which were previously considered as a complication of the TEES method, are not currently such.
This is due to the rapid development of arrhythmology and changes in ideas. However, it must be borne in mind that the doctor conducting the study may encounter two problems:
1. when conducting TEES, the doctor consciously tries to provoke a paroxysm of supraventricular tachyarrhythmia using various stimulation modes, i.e. induction of tachycardia is the goal of the study itself. It is unlikely that this situation should be considered as a complication of the method;
2. when conducting TEES, the induction of tachycardia is a surprise for the doctor conducting the study and occurs for the first time in the patient’s life. Paroxysmal tachycardia can occur when using any stimulation mode. In this situation, the issue is not resolved unambiguously, but depending on the specific form of paroxysm.
The very fact of the possibility of provoking tachycardia indicates that all the necessary prerequisites for the implementation of the re-entry mechanism have been formed in the patient’s heart and only a trigger is needed for the occurrence of tachycardia.
This triggering mechanism was PPES. However, the same paroxysm can occur independently when certain conditions arise - most often the appearance of a supraventricular extrasystole in a certain phase of the cardiac cycle. Thus, provoking tachycardia for the first time in a patient’s life confirms only what may happen to him in the future and, to a certain extent, helps the doctor adjust treatment taking this fact into account.
The specific form of provoked paroxysm should also be taken into account, based on the complexity of treatment and possible complications of this paroxysm. Thus, a paroxysm of nodal AV tachycardia or a paroxysm of reciprocal AV tachycardia in a patient with WPW syndrome (orthodromic or antidromic variant) can be quite easily stopped using the TEES method and, as a rule, does not require intravenous administration of drugs (we must not forget about the possibility of stopping these paroxysms with using vagal tests).
Inducing a paroxysm of atrial fibrillation for the first time in a patient’s life requires further use of medications to stop it, since the TEES method does not stop atrial fibrillation.
Provocation of atrial fibrillation in a patient for the first time in his life often indicates either critical dilatation of the atria or pronounced dystrophic changes in the atrial myocardium [after myocarditis or chronic alcohol intoxication), after which maintaining sinus rhythm becomes a difficult task.
Particular attention should be paid to the development of two forms of paroxysmal tachyarrhythmia - ventricular tachycardia and atrial fibrillation in a patient with WPW syndrome, which, if they develop, should undoubtedly be considered as a complication of the method, associated in turn with a possible error in the study.
These situations should be reviewed and studied in detail to avoid their recurrence in the future. Provoking ventricular tachycardia using the TEES method is a difficult task due to many circumstances. It must be remembered that when affecting the atria, TES can provoke the development of ventricular tachycardia only indirectly through a combination of two unfavorable factors - deterioration of coronary circulation and electrical instability of the ventricles.
Knowing this, the doctor should be especially careful when, with the appearance of significant ischemic depression of the ST segment, ventricular extrasystole of high gradations (according to Lown) appears - frequent, paired, early. In this situation, the study should be stopped immediately, and the identified violations are reflected and emphasized in the study protocol as dangerous in terms of the development of paroxysm of ventricular tachycardia, and the patient himself should be considered as at risk of sudden cardiac death. Thus, the situation with the development of paroxysm of ventricular tachycardia during TEES can and should be controlled, the main thing is that the doctor conducting the study knows about it.
Complications of the TEES method
The problems that a doctor conducting a study may encounter are:
1. Insertion of the esophageal electrode into the trachea instead of the esophagus.
This complication usually occurs among doctors who are just beginning to independently conduct TEES research and is usually associated with their haste when inserting the probe into the esophagus. This complication extremely rarely occurs when the probe is slowly inserted at the moment of swallowing saliva, when the epiglottis rises and the trachea closes.
If the probe gets into the trachea, the patient experiences sudden suffocation, coughing, and redness of the face - the probe should be immediately removed, and the probe should be reintroduced only a few minutes after the described symptoms cease. In extremely rare cases, the erroneous insertion of a probe into the trachea is not accompanied by pronounced reactions on the part of the patient and stimulation is carried out from the trachea. In our practice, we observed one such patient (a former mountaineer, Honored Master of Sports).
To avoid such cases, it is necessary to pay attention to the extremely low amplitude of the “P” wave on the esophageal electrogram at the beginning of the study, as well as the appearance of cough when stimulation is turned on.
2. A burning sensation in the esophagus, behind the sternum.
The appearance of these sensations is mandatory when stimulation is turned on, and their absence in the patient should be associated with a malfunction of the equipment. The patient's level of sensation is usually low or easily tolerated. If the sensations are pronounced and the patient refuses the study, the study is stopped.
3. During stimulation, the patient feels pain in the back associated with contraction of the spinal muscles. In case of severe pain, the study is stopped.
4. When the stimulator is turned on, effective stimulation of the diaphragm occurs, which is accompanied by its rhythmic contractions with the frequency that the stimulator gives at a given time. The patient feels frequent hiccups or shortness of breath, and the doctor conducting the study observes frequent contractions of the diaphragm, which disappears immediately after the stimulator is turned off.
This complication most often occurs in patients with a hypersthenic physique or obesity, because the location of the heart in the chest in such patients is such that the heart practically lies on a highly located diaphragm and the poles of the esophageal electrode during TEES are located in close proximity not only to the atria, but also to the diaphragm. As a rule, the study is stopped when this complication occurs.
A technique in which the esophageal electrode is advised to be pulled up, thereby removing the electrode poles from the diaphragm, rarely gives a positive result, because by removing the probe from the diaphragm, we thereby remove the electrode poles from the zone of their optimal location in relation to the left atrium, and this in turn will require an increase in current strength and, as a result, the re-emergence of effective stimulation of the diaphragm. We observed a patient in whom contraction of the diaphragm during TEES occurred at the very minimum voltage and from the upper part of the esophagus.
5. Electrode getting stuck in the nose is the most unpleasant complication during TEES, as it injures the patient and leads to loss of the electrode.
The esophageal electrode gets stuck in the nose, usually when it is removed after stopping the study. The electrode gets stuck in the area of their poles, because their diameter is larger than the diameter of the probe itself. Electrode getting stuck is associated with injury to the nasal mucosa and its swelling when the probe is inserted. If it is impossible to remove the electrode after applying vasoconstrictor drops into the nose, it is removed as follows: holding the distal part of the probe through the mouth with a special clamp (used in the ENT office), bite the probe near the wings of the nose and remove the probe through the patient’s mouth. It should be emphasized that this complication occurs only among doctors who begin to independently perform TEES, who often forget the “golden rule” - insertion of the probe through the nose should be free and painless for the patient, and therefore atraumatic for the nasal mucosa. This is why anesthesia of the nasal mucosa not only does not help, but also harms when inserting a probe, since it is very important to know about pain when inserting a probe.
In conclusion of the presentation of this topic, it should be said that if the doctor conducting the study has good knowledge of TEES, arrhythmology, issues of cardiology, myocardial electrophysiology, the TEES method is safer compared to other methods of functional diagnostics that use physical activity or the administration of drugs as a load .
to the top of the page
Interpretation of results
The doctor who performed cardiac EPI and the attending doctor should tell the patient what was revealed during the examination. If the patient has not achieved any type of arrhythmia using all cardiac stimulation protocols, the electrogram is considered normal. However, if the patient, despite normal EPI results, continues to complain about heart failure in the future, it is necessary to be observed by the attending physician, and, if necessary, undergo a repeat transesophageal electrophysiological study or endocardial (invasive) EPI.
If, as a result of the procedure, rhythm disturbances were identified and registered, the functionalist doctor gives a complete description of the arrhythmia - the time of occurrence, type, duration of the rhythm disturbance and the stimulation parameters that provoked this arrhythmia.
PPEFI result. Rapid heartbeat (tachycardia) is a normal, transient condition during electrical stimulation of the heart.
Information for patients.
Transesophageal electrophysiological examination (TEPE) is carried out only as prescribed by a doctor.
Patients with attacks of tachycardia (fast pulse) are indicated for this study if they experience episodes of rapid heartbeat that cannot be recorded on an ECG.
During the study, an attack of tachycardia is provoked, which is recorded and analyzed. As a result, the presence of tachycardia is not only confirmed and documented, but its type is also determined. This is an important point in the further treatment of the patient, as well as in determining the indications for radical treatment of tachycardia - radiofrequency ablation of the tachycardia focus.
It is important to know that most tachycardias can now be completely cured. But to do this, you first need to make sure that they really exist and make a diagnosis, which is why a transesophageal electrophysiological study is performed.
In patients with bradycardia (slow pulse), TEE can provide additional information useful for clinical assessment of the disease and choice of treatment. In this case, during the study, the function of the sinus node, which is the source of normal heart rhythm, is assessed. An assessment of the conduction of impulses through the heart through the atrioventricular node is also performed. Typically, patients are referred for TPE if a rare pulse is detected based on ECG data and 24-hour heart rate monitoring.
TPEFI is carried out as follows:
The study is performed in a specially equipped room using a modern automated complex “Astrocard-Polysystem EP/L” (Moscow, Russia) and a bipolar electrode PEDSP-2 from SKB MET (Kamenetsk-Podolsky, Ukraine). This equipment is rightfully considered the most convenient and informative for conducting research.
Transesophageal electrophysiological study is performed strictly on an empty stomach. Before the study, it is necessary to discontinue antiarrhythmic drugs, because they change the electrophysiological parameters of the heart. The doctor must tell you how long you should not take the medication, since it depends on the type of drug.
To conduct the study, a special electrode is inserted into the esophagus. Usually the electrode is inserted through one of the nasal passages, less often through the mouth. Next, the electrode is connected to the complex for performing TPE. When the electrode is installed correctly, its tip is located in the esophagus at the level of the heart.
The study is based on the anatomical features of the location of the esophagus, which is a hollow collapsed tube closely adjacent to the posterior surface of the left atrium and partly the left ventricle. The mucous membrane of the esophagus has relatively low pain sensitivity. A special transesophageal ECG is recorded from the tip of the electrode, which clearly shows processes that are difficult to assess on a regular ECG. After correct installation of the electrode, the transesophageal electrical stimulation protocol is carried out. It involves step-by-step execution of different pacing modes to determine cardiac electrophysiological parameters. To do this, short series of electrical pulses are applied across the electrode. Typically, the applied pulses have an amplitude of 12-25 mA with a duration of 10 ms. During stimulation, patients may feel a tingling and slight burning sensation behind the sternum, but there is no severe pain if the procedure is performed correctly. During stimulation episodes, the patient is asked not to swallow.
During the study, some patients are tested with intravenous atropine. The question of whether this test is necessary is decided during the research process, based on the results obtained.
After receiving all the data, a research protocol is drawn up. Typically, the entire study with registration of results takes 30-60 minutes.
There are contraindications for conducting transesophageal electrophysiological studies:
- inability to insert the electrode into the esophagus (high gag reflex);
- diseases of the esophagus (tumors, strictures, diverticula, esophagitis, varicose veins and others);
- atrial fibrillation at the time of examination, persistent AV block of the third degree;
- circulatory failure II b – III stage;
- valve prostheses;
- acute infectious diseases.
Over the years of successful work, doctors in our department for the surgical treatment of arrhythmias and pacemakers have acquired unique experience in conducting research not only in adults, but also in children.
Doctors perform TPE and also program pacemakers (PACs):
- Ivashkova Irina Yurievna - cardiologist,
- Shupan Emilia Dmitrievna – Ph.D. cardiologist,
- Pushkareva Irina Alekseevna – cardiologist.
Registration for studies is carried out by nurse coordinator Zinaida Vasilievna Zueva by phone (812) 24-600-14 (from 09:00 to 16:00 on weekdays).