Electrophysiological study
– a procedure aimed at obtaining a recording of biological potentials from the inner surface of the heart, using special catheter electrodes and recording equipment.
Carrying out special types of stimulation to study the electrophysiological properties of the conduction system, atrial and ventricular myocardium. Identification of arrhythmia substrates, their localization and electrophysiological characteristics. Monitoring drug and/or non-pharmacological therapy.
Invasive electrophysiological study of the heart (EPS)
has been used in clinical practice since the late 60s, when the technique for recording the His bundle potential was first described. Since then, various methods and methods of EPI, various types of stimulation and a large number of types of multipolar electrodes have found their application in clinical practice.
Currently, a huge number of centers and clinics use EPI for the diagnosis and treatment of various types of arrhythmias and cardiac conduction disorders.
The emergence of the ability for a doctor to conduct EPI allows one to study the basic mechanisms of arrhythmias and cardiac conduction disorders.
The use of EPI helps solve three main problems: diagnosis, treatment
(both therapeutic and surgical) and
prognosis
in many clinical situations.
Methodology
Early electrophysiological studies consisted of recording intrapolar electrical activity during spontaneous rhythm using conventional stimulation electrodes. Modern methods use electrodes installed at several points of the endocardium for simultaneous stimulation and recording. Thus, various electrophysiological parameters are determined both during the spontaneous rhythm and during stimulation. With the help of programmed stimulation, many different heart rhythm disturbances can be caused, the electrophysiological nature of which is determined by the mapping method.
Decoding the results
Advertising:
Interpretation of the results is carried out by the doctor performing the study and the attending physician who referred the patient for the procedure.
Normally, the electrogram obtained during EPI reveals sinus tachycardia with a heart rate of 100 to 120 per minute or more. Such tachycardia is transient and is not dangerous for the patient.
example of EFI results
If the study protocol contains the phrase that no rhythm disturbances were achieved using all types of stimulation, it means that the patient does not have a suspected type of arrhythmia, and the EPS results are regarded as normal. Also, normally there should be no depression or elevation of the ST segment and negative T waves, indicating myocardial ischemia.
If such changes are detected, their location is indicated, as well as the type of electrical stimulation in which they occurred.
When an arrhythmia is detected, its type is indicated (atrial fibrillation, ventricular tachycardia, frequent ventricular extrasystole, etc.), and the stimulation parameters that caused the rhythm disturbance.
Any of the disorders recorded on the electrogram requires careful medical supervision due to the need to prescribe certain antiarrhythmic drugs or perform RFA.
Carrying out, based on the results of EFI, RFA – “cauterization” of the area of pathological electrical activity of the heart
There are the following types of EFI:
1. invasive
invasive, in turn, is divided into three main types:
— endocardial (a study that is used for diagnostic purposes in a hospital setting, without anesthesia and preferably without premedication)
- epicardial (performed during open heart surgery)
— combined (use of two methods if indicated)
Invasive EPS allows ES to be performed in any part of all four chambers of the heart. Since the endocardium does not have pain receptors, ES is completely painless for the patient.
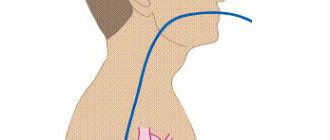
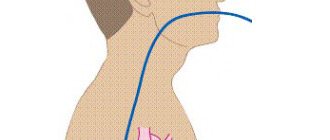
| EPI of the heart. Electrode placement | ChPEC. Electrode location |
2. non-invasive
(transesophageal) has a wide range of applications from outpatient clinics to inpatient units. The method for clinicians in their clinical activities is the most accessible and less burdensome for the patient.
The diagnostic capabilities of TEE are limited to stimulation of the left atrium. In some cases, stimulation of the left ventricle can be achieved, but for this it is necessary to apply a voltage with an amplitude of 30-60 V (mA), which is practically impossible without the use of anesthesia.
to the top of the page
Contraindications for endoEPI
- acute infectious diseases,
- acute myocardial infarction,
- unstable angina for 4 weeks,
- chronic heart failure III-IV f.k. according to NYHA,
- left ventricular aneurysm with thrombus,
- blood clots in the cavities of the heart,
- cardiac mechanical prostheses of the left chambers of the heart with access from the left.
When performing endoEPI, the incidence of complications does not exceed 1%. In order to prevent the latter, all necessary measures are taken at all stages of diagnosis and treatment.
The X-ray endovascular diagnostics and treatment room provides diagnosis and treatment of all types of arrhythmias (brady- and tachyarrhythmias). The department carries out operations within the framework of the state program for the provision of high-tech medical care (HTMC). This type of medical care is provided according to quotas allocated by the Russian Ministry of Health. Patients can also be operated on on a self-supporting basis, taking into account the cost approved by the Clinic.
Indications for EPI
Patients are referred for endocardial EPI of the heart from the therapeutic and arrhythmology departments of district hospitals. The category of patients with unclear etiology of loss of consciousness, paroxysmal forms of supraventricular and ventricular tachycardias, and refractoriness of tachyarrhythmias to antiarrhythmic drugs is determined.
Clinical indications
- Assess sinus node function in symptomatic patients with suspected sinus node dysfunction.
- Repeated syncope - if no cause is found on neurological or non-invasive cardiac evaluation
- Atrioventricular block (AV block) - asymptomatic block of unknown level
- Bundle branch blocks - syncope of unknown etiology
- Tachycardias with wide QRS complexes - differentiation between VT and supraventricular tachycardias with aberrant QRS
- Sustained VTs
- Supraventricular tachycardia - (AV - nodal, hidden accessory pathways, WPW - syndrome and atrial fibrillation)
to the top of the page
Diagnostic application of EPI
The use of EPI in the diagnosis of arrhythmias and conduction disorders depends not only on the nature of the rhythm disturbances, but also on its clinical consequences. A number of tachyarrhythmias require immediate contact with a cardiac surgeon, since their therapeutic treatment is futile and even dangerous.
Before proceeding with invasive diagnostic tests, it is necessary to carefully review the results of noninvasive electrophysiological tests, ranging from 12-lead ECG to dynamic studies such as ambulatory Holter monitoring or exercise testing.
Necessary procedures for EPI
| Procedure | Target |
| History and physical examination | Detection and differential diagnosis of cardiac and neurological pathologies Determining the factors that provoke episodes of arrhythmia Detailing syncope |
| Neurological examination | |
| EEG | Exclusion of pathological activity of the central nervous system |
| CT/MRI | Identification of pathological foci |
| Carotid Dopplerography | Detection of significant cerebrovascular insufficiency |
| ECG in 12 standard leads | Cicatricial changes in the myocardium Intraventricular conduction disorders QT prolongation Ventricular preexcitation syndromes |
| Daily ECG monitoring | Correspondence between the occurrence of symptoms and changes on the ECG Quantification of ectopic activity Daily dynamics of arrhythmias |
| Orthostatic tilt test | Diagnosis of vasovagal/vasodepressor syncope |
| EchoCG | Determining the size of the heart chambers Contractility assessment Detection of local hypo- and akinesias Detection of intracardiac pathology |
| Stress test | Detection of transient ischemia Assessment of the arrhythmogenic function of catecholamines |
| CT – computed tomography; MRI – magnetic resonance imaging; CNS – central nervous system; EchoCG – echocardiography; EEG – electroecephalography. | |
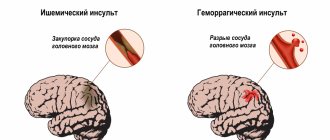
Supraventricular tachycardia in young and practically healthy people sometimes causes minor symptoms or does not cause any symptoms. The same arrhythmia in a sick person with damage to the coronary arteries can cause angina, heart attack or congestive heart failure.
Rhythm disturbances can cause various neurological, cardiac, pulmonary and general symptoms. Reduced reserve capacity of the heart in cardiovascular and pulmonary diseases can aggravate existing clinical manifestations.
to the top of the page
Research methods
EPI of the eye has four research options, including:
- Electrooculography (EOG) is a study of the muscles of the eye and the outer layer of the retina by recording changes in constant potential during eye movement and electrical stimulation of the retina. The results of EOG are directly related to the degree of preservation of the retinal pigment epithelium. Serious changes in the electrooculogram indicate the presence of pathology in Bruch's membrane, pigment epithelium and choriocapillaris layer of the retina.
- Electroretinography (ERG) is the study of retinal function by recording potentials that arise when the retina is irritated by light. ERG allows you to obtain graphs of the activity of retinal cells, depending on the number of intact photoreceptors and neurons. Each graph curve on the electroretinogram displays a layer of cells, the degree of functioning of which is then determined by the doctor based on the reaction to certain stimuli.
- Multifocal electroretinography (MERG) is a study of light sensitivity of the functionally most important central zone of the retina. When performing MERG, a three-dimensional map of this area of the retina is built, indicating both serious lesions and small areas of pathology.
- Visual evoked potentials (VEP) are a study of the response to light stimulation of the optic nerves of the occipital region of the cerebral cortex (according to Brodmann, from fields 17 to 19 of the cerebral cortex). Depending on the objectives of the study and the patient’s visual acuity, the stimuli in the study are flashes of light or structured photostimuli, consisting of alternating white and black cells of different sizes. As a result of the VEP, an electroencephalogram is produced, from which the functional state of the entire visual analyzer and each of its sections can be determined. That is why this method is considered one of the most informative in the topical diagnosis of the development of pathology.
Working closely, an ophthalmologist and an electrophysiologist who uses EPI of the eye develop a strategy and decide on an examination method for early or differential diagnosis of pathologies of the visual analyzer. It is with EPI of the eyes that specialists receive the most objective data about existing diseases, which are decisive when making a diagnosis.
The use of EPI in assessing the effectiveness of antiarrhythmic drugs
The transesophageal pacing (TEPS) method is predominantly used to evaluate antiarrhythmic drugs.
Electrophysiological serial drug testing allows for precise selection of medications that can effectively prevent arrhythmia paroxysms, as well as predict and monitor the duration of therapeutic success.
EPI in order to determine the antiarrhythmic effectiveness of medications is carried out if there are positive answers to the following two questions:
Is provoked tachycardia identical to spontaneous tachycardia?
Do changes in electrophysiological parameters observed during EPS with intravenous drug administration allow us to predict the effectiveness of treatment?
In clinical practice, there are absolute and relative indications for electrophysiological testing of medications:
I. Absolute:
1) History of attacks of cardiac arrhythmias, confirmed by EPI results.
2) Absence or loss of antiarrhythmic effectiveness of drug treatment, especially if there is a history of loss of consciousness or other signs of hemodynamic impairment.
II. Relative:
1) During EPI, no indications are found for the implantation of a pacemaker, defibrillator, or radical surgical treatment.
2) Against the background of electrical stimulation treatment, paroxysms of tachycardia occur - the need for combination with drug treatment.
3) Recurrence of tachycardia after surgical treatment.
4) The purpose of drug testing during EPI is to find an antiarrhythmic drug that stops tachycardia that is identical to that occurring spontaneously, or prevents its provocation.
After determining the possibility of provoking and stopping tachycardia, an acute pharmacological test is performed. For this purpose, against the background of induced paroxysm, no less than 5 minutes after its onset, the patient is slowly administered an antiarrhythmic drug intravenously, under monitor control, and its effect on arrhythmia is determined by conducting a comparative assessment of the electrophysiological parameters of the heart.
before and after drug administration. The dose of the drug should not exceed the calculated one (slide 18), but if restoration of sinus rhythm occurs earlier, the infusion can be stopped.
Initially, the relief effect of the drug is assessed. If, after a period of time sufficient for its manifestation, sinus rhythm has not been restored, vagal maneuvers are performed again. If they are ineffective, paroxysm is stopped with the help of ES, which does not exclude further evaluation of the protective effect of the drug.
After restoration of sinus rhythm, the study preceding the drug test is repeated to assess the protective effect of the drug. It should be noted that, in some cases, the same drug can stop paroxysm and not prevent its occurrence, and vice versa.
It is recommended to study the effectiveness of only one, or less often two, drugs within one day. Studying the effectiveness of several medications during one study is acceptable only if it is possible to determine the concentration of the drug in the patient’s blood so that the previous drug does not affect the effect of the subsequent one.
There are three possible modes of action of the drug:
I. positive action;
1) tachycardia stops;
2) the use of the drug prevents the (previously possible) provocation of arrhythmia;
3) stable tachycardia becomes unstable;
4) the duration of the cardiac cycle increases (heart rate decreases) during paroxysm.
5) difficulty in provoking paroxysm (narrowing of the “window” of tachycardia by more than half, the need for more aggressive methods of stimulation, the emergence of sensitivity of tachycardia to vagal techniques).
II. Absence of any effect on tachycardia.
III. Negative effect (arrhythmogenic effect):
1) paroxysms of tachycardia become more severe;
2) the aggressiveness of methods for inducing tachycardia is reduced;
3) side effects appear (they are also possible with the first two options for influencing tachycardia).
The presence of a protective effect allows the drug to be prescribed for oral administration in doses that allow it to achieve concentrations in the blood similar to those for intravenous administration. A few days later (after reaching the required concentration of the drug in the blood serum), the study must be repeated.
Reliable criteria for the effectiveness of selected antiarrhythmic therapy are the absence of paroxysms or a significant reduction in their frequency and duration, facilitating the conditions for their relief.
In conclusion, the following generalizations can be made:
1) EPI allows you to select antiarrhythmic drugs to stop and/or prevent paroxysms of tachycardia;
2) drug testing with EPI significantly reduces the time to search for an effective drug, while other testing methods (without the use of stimulation) are quite lengthy;
3) if all antiarrhythmic drugs are ineffective, indications arise for non-drug treatment (electric stimulation or radical surgery).
to the top of the page
How to prepare for the procedure?
Advertising:
All nuances of preparation for the study must be carefully explained by the doctor to the patient. Firstly, the patient (under the supervision and as directed by a doctor!) must stop taking any antiarrhythmic drugs, as they can distort the results of the study. Secondly, before the TPE procedure, a patient experiencing even slight discomfort from the stomach must undergo fibrogastroscopy in order to exclude acute gastroesophageal pathology.
Before the endoEPI procedure for attacks of loss of consciousness, a neurologist must exclude brain pathology that could cause fainting, and this may require a CT scan or MRI of the skull.
Due to the fact that endo- or epi-EPI requires hospitalization in a hospital, a patient undergoing a routine examination must provide the doctor with the results of tests for HIV, syphilis, hepatitis and blood clotting no later than two weeks ago (different institutions have their own deadlines) .
The study is carried out strictly on an empty stomach. The need for epi-EPI on an empty stomach is due to the fact that during general anesthesia, vomiting of eaten food or liquid and aspiration of vomit may occur.
After the necessary preparation, the patient is hospitalized in a hospital. He must have the results of the examination (ultrasound of the heart, 24-hour monitor), as well as an extract from the outpatient card or discharge summary from the institution where he received examination and treatment before. The extract must indicate the rationale for the need for EFI with a detailed clinical diagnosis.