How to increase neutrophils in the blood
When a person has a low percentage of neutrophils, it is necessary to eliminate the problem that caused this condition. If this happened due to an infectious disease, then they recover on their own in a short period of time. In other circumstances, the only way to increase neutrophils in the blood of a child or adult is to eliminate the root cause of their decrease. The doctor may prescribe drug therapy, which is relevant for severe neutropenia. If the disease manifests itself moderately, then:
- leukopoiesis stimulants are prescribed;
- The use of Pentoxyl and Methyluracil is considered effective.
Therapy should be carried out after consultation with an immunologist under the supervision of an immunogram. When the body does not respond to treatment and white blood cells are still low, colony-stimulating factor medications are prescribed, for example, Lenograsti, Filgrastim. These same medications are immediately prescribed to patients with agranulocytosis. Such drugs are prescribed only under conditions of inpatient treatment, because this is a potent group of drugs.
Find out what the norm of leukocytes in the blood of women should be.
Ways to increase neutrophil levels
The most important thing is that you work with your doctor to learn about the reasons for your low neutrophil levels. And get a prescription from your doctor to treat the underlying cause or disease. Treatment for neutropenia will depend on the causes of the disorder.
Medical treatments that help reduce the impact of neutropenia:
Granulocyte-colony-stimulating factor (g-CSF): This is a glycoprotein that stimulates the bone marrow to produce neutrophils and other granulocytes to release into the bloodstream. The most commonly used version of g-CSF is a drug called filgrastim.
Granulocyte-macrophage colony-stimulating factor (GM-CSF): A naturally produced glycoprotein that has a similar role in stimulating neutrophil production. Factors are used to restore the number of neutrophils after chemotherapy.
Antibiotics : These medications may be prescribed prophylactically to reduce the chance of infection in neutropenic patients. They are often taken at a time when the neutrophil count is at its lowest.
Talk to your doctor about additional lifestyle changes listed below. None of these strategies should ever replace what your doctor recommends or prescribes.
Lifestyle changes to increase neutrophil counts:
Exercise , eat a healthy diet , quit smoking and avoid drinking alcohol .
It is important to have a balanced diet containing sufficient amounts of vitamins B12 and folate, which are necessary for the formation of white blood cells, including neutrophils. (, )
Regular moderate exercise can help improve neutrophil function and activity. ()
When your neutrophil count is low, you may be more vulnerable to infections. Proper hygiene can reduce the risk of these infections. ()
For what reasons do neutrophils decrease?
Most often, neutrophils decrease due to the occurrence of an inflammatory disease, viral infection and radiation exposure. Quite often the following factors provoke the appearance of neutropenia:
- poor environmental conditions;
- use of certain medications (“Sulfanilamide”, “Analgin” and “Levomycetin”);
- inflammatory process in the body.
A reduced percentage of neutrophils is not an independent disease. This is only the result of the development of another disease, which can be identified after a thorough medical examination. If laboratory test results are unsatisfactory, you should visit a hematologist. After a thorough examination, the specialist prescribes complex therapy.
Negative effects of elevated neutrophil levels
Too much neutrophil activity can increase the release of agents toxic to cells (cytotoxic) and over-activate parts of the immune system. Under normal circumstances, this helps protect your body from infection or injury. However, prolonged and unregulated release of these compounds can cause damage to body tissue. (, )
Diseases of the cardiovascular system
Research shows that neutrophils increase inflammation in plaque in hardened arteries (atherosclerosis). ()
After a heart attack, neutrophils clear away dead cells and debris around the damaged area in the heart. After the neutrophils die, macrophages release growth factors that cause inflammation and tissue formation, which creates scarring in the heart (cardiac fibrosis). ()
A high neutrophil-to-lymphocyte ratio (NLR) is a predictor of cardiovascular disease. It is associated with an increased risk of developing irregular heartbeats (arrhythmias) and death in patients undergoing treatment for cardiovascular disease (percutaneous coronary intervention) [,].
A study of 4,625 people found that higher neutrophil counts were associated with an increased risk of developing cardiovascular disease. () Similar results were obtained in another study with 4,860 men. ()
Another study of 18,558 people found that high levels of neutrophils increased the risk of cardiovascular disease such as ischemic stroke and myocardial infarction. ()
Cancer
In general, neutrophils may play a role in the initiation of cancer , tumor formation , and the spread of metastases to other sites in the body. ()
Neutrophils promote inflammation by releasing reactive oxygen species (ROS). Research shows that they also suppress the antitumor immune response (by stimulating TGF-β to release iNOS or ARG1, which suppresses cytotoxic CD8+ T cells that fight cancer cells). ()
Neutrophils contribute to the development of cancer. (source)
The neutrophil to lymphocyte ratio ( NLR = neutrophil/lymphocyte) is a blood marker that scientists have used to try to predict the outcomes of various types of cancer (colon, lung, head, neck, ovarian, etc.). Numerous studies have shown that elevated NLR values are associated with poor prognosis in colon cancer, pancreatic cancer, gastric cancer, and lung cancer . (, , , )
In a review of more than 100 studies and 40,000 patients, an NLR value greater than 4 was associated with worse overall cancer survival rates. ()
Interpretation of the NLR depends on the clinical context. However, we can roughly imagine how this indicator can be assessed:
- Normal NLR level is in the range of 1-3
- An NLR of 6-9 suggests mild inflammatory stress (eg, in a patient with uncomplicated appendicitis)
- Severely ill patients often have an NLR of ~9 or higher (sometimes reaching values close to 100)
Neutrophils are normal
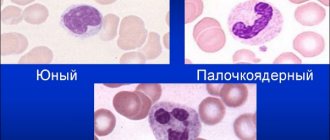
This indicator is designated neut in a blood test of type wbc; two subgroups of these cells are distinguished. Inside the body, there are 2 phases of granulocyte maturation; this process takes place in the bone marrow. Initially, the cells are called myelocytes, after which they turn into metamyelocytes. They are formed exclusively inside the bone marrow and do not enter the blood, so the WBC analysis should not detect them.
At the next stage, they look like a rod, which is where the name of the form comes from – rod-shaped. After maturation, the cells acquire a segmented nucleus; at this stage, segmented leukocytes are formed. The norm of neutrophils in the blood is determined by these two types of cells: wbc analysis indicates the percentage of the total number. From the total number of leukocytes, the ratio of each type is calculated: this is called the leukocyte formula.
- Segmented blood neutrophils: normal indicators and causes of deviations from the norm
Band neutrophils are normal
The indicators of these cells do not depend on the gender of the person; the main criterion for assessing the normal indicator is the patient’s age. This is one of the types of cells that are taken into account in the leukocyte formula. If band neutrophils are studied, the norm is significantly different in an infant and a child who is already a week old. It should be remembered that this is only a part of the total leukocyte cell content. Normal values are shown in the table:
| Age | Number (% band) |
| Baby | From 5 to 12 |
| 7 days from birth | From 1 to 5 |
| 14 days | From 1 to 4 |
| 1 month | From 1 to 5 |
| 1 year | From 1 to 5 |
| Preschooler | From 1 to 4 |
| 6-12 years | From 1 to 4 |
| Adult | From 1 to 4 |
Segmented neutrophils are normal
This is the second form of leukocyte cells that are taken into account in the analysis. This is the second element that is taken into account in the leukocyte formula. The transcript of the general analysis will indicate segmented neutrophils - the norm is:
| Age | Number (% segmented) |
| Baby | 50-70 |
| 7 days from birth | 35-55 |
| 14 days | 27-47% |
| 1 month | 17-30% |
| 1 year | 45-65% |
| Preschooler | 35-55% |
| 6-12 years | 40-60 |
| Adult | 40-60 |
Neutrophils are normal in children
After a general analysis, the doctor pays attention to the number of leukocytes. If they are decreased or increased, this indicates the possible development of some pathology. A deviation in the indicators of one of the types of leukocytes will indicate a specific type of disease. The main task of these cells is to fight fungal and viral diseases. Doctors have established the norm of neutrophils in the blood of children, which indicates the absence of pathologies.
- In the first days of life, the child should have 50-70% segmented and 5-15% band.
- The number of these cells by the end of the first week should be 35-55% and 1-5%.
- After two weeks, the indicator of rod cells will be 1-4%, and segmented cells - 27-47%.
- By the end of the month of life, the child will have 1-5% band, 17-30% segmented, and by the year 1-5% and 45-65%.
- 1-4% and 35-55% are the norm for children 4-6 years old.
- At the age of 6-12 years, the indicators are 1-4% band-nuclear, 40-60% segmented.
For diagnosis, indicators in the analysis are important not only the independent norm of neutrophils. The ratio between all segmented, young cells must be taken into account, which may indicate the presence of some neutrophilic shift. To determine the presence of a particular disease, the individual number of rod and segmented cells is not significant.
The norm of neutrophils in the blood of women
Certain fluctuations in the normal number of immune cells are observed only in the first years of a person’s life. In adulthood, this value always remains at the same level. If immune cells are low or high, this indicates the development of the disease. The norm of neutrophils in the blood of women should be as follows: 40-60% segmented cells and 1-4% band cells.
The norm of neutrophils in the blood of men
The gender of a person does not matter when determining the normal level of protective cells. The main parameter is age, for example, in a child under one year old there are noticeable jumps in the content of leukocytes. The norm of neutrophils in the blood of men is the same as that of women: 1-4% rod- and 40-60% segmented cells. A change in this indicator will be associated with inflammatory or infectious processes occurring in the body.
Functions of neutrophils
Like other blood cells, neutrophils are produced in the bone marrow. (, ) They make up the largest portion of the blood cells produced by the bone marrow. They are our “first defenders”, playing the role of the first line of defense against infectious organisms entering the body.
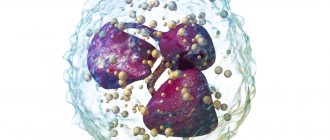
Neutrophils appear first at the site of infection and inflammation . (, ) They attack foreign organisms by “eating them” through a process called phagocytosis , or by engulfing them in a process called endocytosis . Once the foreign organism is inside the neutrophil, it is “attacked” by enzymes that lead to the destruction of the enemy. Neutrophils also help regulate the overall immune response. ()
In response to infection or inflammation, circulating neutrophils release surface molecules that facilitate their interaction with activated endothelium. During inflammation and infection, neutrophils release mediators that promote the subsequent immune response by modulating the adaptive function of immune cells. (source)
The rapid response of neutrophils to infection makes them the first group of immune cells to participate in the immune response during infection or injury. They produce antimicrobial substances and proteases (enzymes) that help degrade and kill microbes. ()
Neutrophils can also produce cytokines (CXCL2, CCL3, IL-6, TNF-alpha) to support the body's inflammatory response to infection. (, )
After they finish defending our body against pathogens, some neutrophils activate macrophages (large white blood cells) to help remove destroyed microbes and neutrophils from the body. The limited lifespan of the neutrophil helps prevent further tissue damage and excess inflammation. ()
NEU formation and typing
Neutrophil formation begins in the red bone marrow. The particles then penetrate the plasma, where they are divided into segments for further maturation. NEU typification is determined by their maturation:
- Rods. This name was given by its external feature – the shape of the sticks. They are immature (young) blood cells and do not have a segmented nucleus. When their number goes beyond normal limits, the leukocyte formula has a “shift to the left,” otherwise cell rejuvenation. In most cases, such an analysis result requires checking the patient for the presence of oncology. And also an increased content of stabs is a clinical sign of a diabetic crisis.
- Segmented. Fully mature blood cells, with a pronounced nucleus at the base. Exceeding their number shifts the leukogram formula to the right (cellular aging). This may be a sign of depletion of bone marrow reserves, chronic renal failure (CRF). A non-pathological shift to the right is a recent blood transfusion (blood transfusion).
The average lifespan of a mature neutrophil in tissues is three (sometimes four) days. To timely replenish the antimicrobial “army,” the red brain is forced to produce them in large quantities. After eradication (destruction) of pathogenic microorganisms, NEU die and, together with other organic decay products, form purulent masses.
This type of programmed cell death is called netosis. There are certain types of bacterial microorganisms that NEUT cannot resist, and then the infectious-inflammatory process becomes chronic and protracted.
The overall high concentration of granulocytes of this type is designated as neutrophilia or neutrophilic leukocytosis (absolute or relative). A decrease in their number in the blood is called neutropenia. The neutrophil response to bacterial and infectious invasions is primary in acute inflammation. In relation to chronic pathological processes, NEU do not show much activity.
Neutrophil norm (reference values)
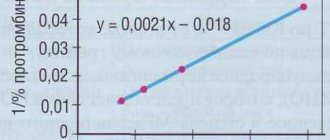
The absolute neutrophil count (ANC) can be calculated using the formula:
ACN = NEU x WBC / 100
Where:
NEU - total number of neutrophils
WBC - leukocytes (109 cells/l)
Neutrophil reference values may vary between laboratories. The approximate norms of neutrophils in adults are as follows:
- segmented neutrophils: 40-70% or 1.7-7.2 x 10⁹ cells/l (1700-7200 cells/µl)
- band neutrophils: 1-6% or 0.1-0.6 x 10⁹ cells/l (100-600 cells/µl)
Norm of neutrophils during pregnancy
The number of neutrophils increases during pregnancy. During pregnancy, an acceptable value is considered to be an increase in neutrophils to 10x10⁹ cells/l or up to 80%.
Norm of neutrophils in children
Reference values for neutrophils for children differ from adult values. The presence of a small amount of immature forms is allowed in children's blood.
At birth, the number of neutrophils is increased. Then gradually the level of neutrophils decreases and in adolescence approaches the norms of an adult.
Results
Neutrophils are a type of white blood cells (leukocytes) responsible for eliminating bacterial microorganisms and cancer cells. They are divided into band (young) and segmented (mature leukocytes). An increase in NEU (NEUT) levels in the blood indicates their mobilization to combat purulent-inflammatory processes, malignant neoplasms, and hemolytic diseases.
A decrease in the level of neutrophil leukocytes indicates chronic pathologies, viral infections, and irradiation of the body. The results of the study are recorded as a percentage of the total number of leukocytes, and in absolute units multiplied by 10^9 (that is, a billion cells per liter of blood). Microscopy and neutrophil counting are performed as part of a general clinical blood test.