Transient ischemic attack of the brain is a temporary acute disorder of the central nervous system. In medical practice, such a pathology may also be called a microstroke. The only difference is the duration of symptoms. In the case of transient ischemia, the signs disappear within an hour; they do not have irreversible consequences. Most often, this type of disorder is found in older people.
Diagnosis is carried out on the basis of the totality of all information obtained through medical research: computed tomography, magnetic resonance imaging, ultrasound and PET scans of brain regions. Additionally, laboratory procedures may be prescribed. It is advisable to undergo the examination in specialized neurological centers.
Treatment of transient ischemic attack of the brain can be conservative, symptomatic and surgical. It all depends on the patient’s age, the presence of concomitant diseases and general condition. Therapy is necessary to eliminate the risk of stroke. According to statistics, a patient’s risk of stroke after 2 days after an attack is 4%, after 30 days - 8%, within 5 years - 29%.
General information
The concept of transient ischemic attack (abbr. TIA ) is quite broad and represents a transient circulatory disorder of the brain.
Assigned code for transient ischemic attack according to ICD-10: G45.9. The pathology develops according to the ischemic type - it occurs as a result of a local decrease in blood circulation and leads to episodes of neurological disorders ( paresis and various sensitivity disorders). TIA is also accompanied by retinal ischemia, but there is no development of cerebral infarction . If irreversible ischemic damage to areas of the brain is detected, then they talk about stroke .
Ischemic attack, what is it? Previously, it was believed that an attack is a disease of rapidly developing symptoms with focal and diffuse damage to brain functions, which occurs without the influence of obvious extravascular factors and lasts less than 1 day. However, later the scientists changed the definition, since symptoms often persisted for 24 hours on an MRI of the brain under diffusion-weighted conditions and led to a heart attack. Therefore, it has now been established that on average the duration of transient attacks usually does not exceed 1 hour.
Today, it is quite important to promptly identify TIAs and assess the extent of lesions, but, unfortunately, patients do not pay attention to periodically transient symptoms and do not consult a doctor. And this is a very bad trend, because in 30-50% of cases, people who have suffered a transient ischemic attack or the so-called micro-stroke are diagnosed with a stroke within 5 years.
Neuroimaging and antiplatelet therapy
Neuroimaging results can have a significant impact on the choice of treatment options. Aggressive management of patients with DAPT increases the risk of intracranial hemorrhage (ICH). And this significantly limits the treatment of patients with TIA in contrast to patients with ACS. And although current clinical guidelines allow prescribing DAPT to all patients with TIA and minor IS, it is safer to start treatment with a loading dose of acetylsalicylic acid (300–325 mg), and include clopidogrel (as the second component of DAPT) in a loading dose of 300 mg in the treatment regimen after performing MRI (CT) [3, 4, 11]. It should be noted that the 2021 Russian clinical guidelines demonstrate a more cautious approach to DAPT, prescribing the prescription of two antiplatelet drugs only to patients who, along with the picture of acute cerebral ischemia, also have cardiac indications for more aggressive therapy [12]. If, according to the results of neuroimaging, biomarkers of a high risk of ICH are detected in a patient, the doctor may therefore limit the aggressiveness of treatment (Table 1).
If MRI (CT) does not detect biomarkers of high risk of ICH, then DAPT for 2–3 weeks. significantly reduces the likelihood of all vascular events and IS. Loading doses (300–325 mg for acetylsalicylic acid and up to 300 mg for clopidogrel) have been used in clinical trials, which showed a 32% reduction in the likelihood of stroke within 90 days after TIA [13–16]. Studies [14, 17–19] have established that patients with TIA and minor IS without signs of amyloid cerebral angiopathy receive benefits from DAPT. The 2021 AHA/ASA clinical guidelines allow the use of DAPT for TIA and IS, allowing for the possibility of extending such therapy up to 3 months. [eleven]. Recent European guidelines demonstrate a more cautious approach to aggressive antithrombotic therapy, limiting the duration of DAPT to 10–21 days [17]. Thus, active antiplatelet therapy for patients with TIA is not only possible, but also highly advisable [10, 17, 18]. The trend in recent years towards an increase in the activity of antithrombotic therapy for TIA seems obvious. Antiplatelet drugs are prescribed as early as possible in combinations and doses that best prevent recurrent vascular events. The relatively new concept of “early secondary prevention” involves active or even aggressive management of patients in the first hours and days after the onset of symptoms of circulatory decompensation in the cerebral vascular system. Antiplatelet agents are prescribed regardless of the suspected stroke subtype. However, several days after cardiac examination, patients with atrial fibrillation should receive anticoagulants instead of antiplatelet agents. The principle approach to the active management of patients with TIA is not limited to antithrombotic therapy. Antihypertensive and lipid-lowering therapy for patients with signs of TIA differs from the strategy used for large-focal strokes.
Pathogenesis
Ischemia of brain tissue is a transient disorder of cerebral blood supply, which is also called a microstroke. In this case, neurological symptoms disappear spontaneously within an hour after the end of the attack, without causing irreversible organic damage to the structures of the brain.
Transient ischemic attacks usually develop in conditions of atherosclerotic occlusion of the main vessels bringing blood to the head. These include the carotid artery system - especially at the bifurcation sites, as well as the vertebral arteries. Most often, the pathogenesis is facilitated by compression and vasospasm caused by osteochondrosis .
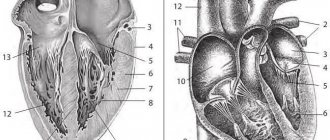
Mechanism of development of TIA
Ischemia of cerebral tissue includes 4 stages:
- Autoregulation - which occurs due to compensatory dilation of cerebral vessels as a response to reduced perfusion pressure of cerebral circulation, causes an increase in the volume of blood that fills the vessels of the brain.
- Oligemia - a further increase in the fall in perfusion pressure indicators causes a decrease in cerebral blood flow, when it cannot be compensated by autoregulatory mechanisms; at this stage, the processes of oxygen metabolism are not yet disrupted.
- Reversible ischemia is the development of an “ischemic penumbra” caused by an increasing decrease in perfusion pressure and a decrease in the level of oxygen metabolism, which leads to hypoxia and disruption of neuronal function.
- Irreversible ischemia is irreversible cell death or apoplexy depolarization of neurons.
Thus, a microstroke causes disturbances in cerebral hemodynamics, sudden and short-term dyscirculatory disorders in the structures of the brain, manifested by focal and general cerebral symptoms that persist throughout the day.
Blood pressure control and lipid-lowering therapy
Aggressive therapy for TIA, in addition to DAPT, involves prescribing lipid-lowering and antihypertensive therapy with achieving target blood pressure values (130/80 mm Hg) as soon as possible. This treatment strategy differs significantly from the procedure adopted in the current recommendations for providing care to patients with stroke, which do not mention statins, and arterial hypertension up to 180 mm Hg. Art. is considered acceptable in the first hours of the disease [12]. Arterial hypertension is the most important risk factor for IS and a frequent accompaniment of the acute period of vascular accident. The causes of arterial hypertension in the acute period of IS are associated with activation of neuroendocrine and neurogenic mechanisms of blood pressure regulation, ischemia of brain stem structures, hospital stress, and disruption of autoregulation of cerebral circulation [20]. The optimal values of systolic and diastolic blood pressure in the acute phase of IS have not been established, and clinicians do not have a consensus on this matter. Large studies that should resolve this issue have not yet been completed [20–22]. The only argument justifying a high level of blood pressure in the acute period of IS is the supposed possibility of better perfusion of brain tissue in the area of the ischemic focus at high systemic pressure in conditions of autoregulation failure [23, 24]. However, the results of recent studies do not support this idea [24]. The assumption about the beneficial effect of high systolic blood pressure on the damaged brain also seems unconvincing with regard to perivascular edema, since in patients with high blood pressure values and developing cerebral infarction, edema in the damaged area is more pronounced [24, 25]. The preservation of “therapeutic” arterial hypertension in patients with TIA seems even less justified. Transient focal cerebral ischemia is very often associated with hypertensive crisis, cerebral vasospasm and thromboembolism. In all cases of TIA, conditions for restoring cerebral blood flow will be better when blood pressure levels are close to normal. Lipid-lowering therapy with statins is not mentioned in guidelines for the management of patients in the acute period of stroke, but is actively used in patients with TIA [2, 3, 25]. The pleiotropic effects of statins, which reduce edema, stabilize atherosclerotic plaques and restore microcirculation, may be useful not only for preventing a recurrent vascular event. Studies in which biomarkers of inflammation and tissue destruction (high-sensitivity C-reactive protein and matrix metalloprotease 9) were used to verify the results of intensive lipid-lowering therapy in patients with atherothrombotic IS showed the effectiveness of atorvastatin at a daily dose of 60 mg [25].
Classification
A transient ischemic attack can vary in duration and severity, so TIA attacks can be:
- light – their duration usually does not exceed 10 minutes;
- moderately severe - lasts from 10 minutes to several hours and does not cause organic symptoms after complete restoration of functions;
- severe - can last up to 24 hours and result in mild organic symptoms after complete restoration of function.
The clinical picture of TIA differs depending on which part of the blood supply the occlusion in - in the vertebrobasilar or carotid system.
Transient ischemic attack in the vertebrobasilar region
According to Vereshchagin N.V. (1980) TIA occurring in the vertebrobasilar region is the most common type of transient ischemia, accounting for approximately 70% of all cases. Clinical manifestations consist of a number of symptoms and syndromes:
- systemic cases of dizziness with attacks of headache in the back of the head and other brainstem symptoms;
- various disorders of the visual analyzer: nystagmus , diplopia , hemianopsia ( bilateral blindness occurring in half the visual field), photopsia (appearance of moving images in the visual field);
- nausea and vomiting that may be uncontrollable;
- alternating syndromes and different manifestations of Wallenberg and Zakharchenko syndrome;
- drop attacks (a sudden fall of a person without loss of consciousness);
- disorientation attacks;
- temporary memory loss and other signs of transient global amnestic syndrome;
- syndrome of blood flow insufficiency in the arteries of the vertebrobasilar region, most often occurring in the form of dyscirculatory fainting - Unterharnscheidt syncope .
Cause of transient ischemic attack in the vertebrobasilar region
Transient ischemic attack in the carotid system
Occlusion of the arteries of the carotid system leads to:
- to transient hemi- and monoparesis ;
- hemitype hypoesthesia
- various speech disorders, most often manifested as partial motor aphasia ;
- development of optic-pyramidal syndrome .
Arteries of the carotid basin
Cerebral circulatory disorders in cervical osteochondrosis
Cervical osteochondrosis is a modern disease that affects 60-80% of the middle-aged population of industrialized countries. It leads to stenosis - compression of blood vessels along the spinal cord as a result of the formation of hernias , osteophytes , as well as the proliferation and thickening of other vertebral tissues. Initially, a person experiences only stiffness and pain in the affected part of the spine, but later radicular syndrome . It manifests itself in the form of headache, paresthesia, speech and smell disorders.
The most dangerous thing with cervical osteochondrosis is compression - squeezing the vertebral artery of the carotid system. It causes the development of vertebral artery syndrome , which is expressed as a constant or paroxysmal burning headache, most of all affecting the back of the head, temples and neck. It can lead to ischemia of cerebral tissues and the development of various cerebral and focal symptoms, as in a microstroke .
Carotid artery lesions
The appearance of typical symptoms is observed after a 2-5 minute period. When the circulation of the circulatory system in the area of the carotid artery is dysfunctional, the patient feels weak, suddenly loses vision, and completely or partially stops speaking.
Motor dysfunction of the limbs on one side is often observed, and the patient also loses sensation.
The pulse drops rapidly and a noise is heard in the carotid artery. The disease may be indicated by focal symptoms of damage to the brain structures of the head: the face becomes asymmetrical, the pressure fluctuates, the retina changes.
There is a feeling of heaviness in the sternum area, the heart is working intermittently, there is not enough air to breathe, convulsions appear, and you want to cry.
Causes
The main causes of transient ischemic attack are arterial hypertension, thromboembolism and atherosclerotic lesions of large vessels that bring blood to the brain, for example, the vertebral and carotid arteries. In addition, disturbances in the nervous regulation of the state of blood vessels and metabolic processes in the brain, the presence of morphological changes such as stenosis, as well as changes in the physicochemical and biochemical properties of the blood play a significant role in the pathogenesis. These include an increase in viscosity, adhesion and aggregation of blood cells.
People most at risk for developing TIA are:
- senile and elderly people;
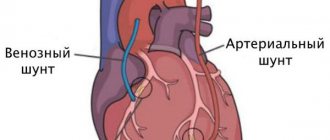
- suffering from arterial hypertension or heart disease, including atrial fibrillation, left ventricular aneurysm, cardiomyopathy, bacterial endocarditis , previous myocardial infarction or the presence of an artificial heart valve;
- patients with diabetes mellitus ;
- when the vertebral artery is compressed by osteophytes formed as a result of cervical osteochondrosis or ankylosing spondylitis (Bechterew's disease) ;
- exposed to stress and occupying responsible positions;
- excessively heavy loads and difficult working conditions;
- with a long history of smoking;
- with reactive changes in myocardial and endothelial tissue caused by Fabry disease ;
- having deposits of globosides in the tissues and organs of the cardiovascular system.
Symptoms of transient ischemic attack
Symptoms of an ischemic attack of the brain can vary significantly depending on which part of the brain is affected, but there are a number of clinical disorders that are general cerebral symptoms, these include:
- dizziness;
- headache;
- short-term loss of consciousness.
Focal symptoms of cerebral circulatory disorders manifest themselves as:
- temporary loss of speech and speech disorders - aphasia;
- loss of the ability to read and/or write;
- weakness in one half of the body - hemiparesis , causing loss of balance and impaired coordination of movements;
- strabismus or immobility of the eyeballs, loss of vision or its sharp deterioration;
- involuntary urination;
- numbness - hypoesthesia , sensitivity and tingling - paresthesia .
Complications and consequences of ischemic attack of the brain
A transient attack is characterized by incoming symptoms as a result of impaired cerebral circulation. They should pass within 24 hours and not provoke serious consequences. Symptoms that persist after a severe microstroke include:
- slurred speech;
- amnesia;
- paralysis;
- deterioration of visual acuity.
For rehabilitation after a mini-stroke and the most successful prognosis - prevention of ischemic stroke, the help of many specialists is needed:
- neurologist – monitors the condition of cerebral vessels, the functioning of neurons and the level of metabolic processes in the brain;
- cardiologist - will select the best treatment regimen to normalize blood pressure and heart rate;
- endocrinologist - will help adjust blood sugar levels and neutralize the negative effects of diabetes ;
- speech therapist - a specialist who will help solve speech problems;
- psychologist – necessary for the correction of mental disorders.
Diagnosis of TIA
After the occurrence of any symptom, the person must be hospitalized in the neurological department. Specialists from European clinics are able to urgently perform a head MRI and CT scan on a patient to monitor changes in the brain, diagnose ischemia or differentiate nosological forms.
MR or CT angiography allows visualization of damage to the blood vessels of the brain - procedures for contrast examination of the arteries after the injection of contrast into the vein. Simultaneously with assessing the patency of the arterial network, the state of the cardiovascular system is assessed:
- Holter monitoring;
- Echocardiography;
- Electrocardiography.
Laboratory diagnostic methods:
- Determination of anticardiolipin antibodies, lupus anticoagulant, antithrombin III, protein S and C, D-dimer, von Willebrand factor;
- Study of coagulogram;
- Biochemical analysis.
After the first neurological signs of a cerebral ischemic attack appear, consultation with several specialists is required - an ophthalmologist, a cardiologist, a therapist.