The role of venous circulation disorders in the origin and course of cerebrovascular diseases has been underestimated for a long time. This is explained by the previously existing difficulties of intravital assessment of cerebral venous hemodynamics when using traditional methods of recording venous blood flow in the vessels of the brain, as well as insufficient attention from researchers to this section of angiology.
The emergence of modern neuroimaging methods, in particular MRI diagnostics, has greatly facilitated the identification of such diseases.
Let's consider several examples of pathological processes detected by MRI diagnostics using MR venography.
THROMBOSIS OF THE VEINS AND SINES OF THE BRAIN
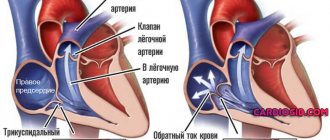
The cause of the development of thrombosis of the veins and sinuses of the dura mater can be septic lesions, trauma, compression of the sinus by a tumor, and systemic lesions of the connective tissue.
In addition, sinus thrombosis can develop due to thrombophlebitis of the extremities or inflammatory foci in the body (in the postpartum period, after an abortion, with infectious diseases, as well as diseases of the ears and paranasal sinuses).
Taking into account the patient’s age, the degree of development of collateral circulation, as well as the localization of the pathological process, the clinical manifestations of venous thrombosis are quite variable and nonspecific.
It is very difficult to identify typical clinical manifestations of sinus thrombosis, but the most common initial symptoms are the following: 1. headache 2. papilledema (a sign of intracranial hypertension) 3. focal neurological deficit 4. disturbances of consciousness (appear in case of damage to the brain substance in the form of progressive edema, developing infarction or hemorrhage).
In case of damage to the sinuses, general cerebral symptoms depend on the size and rate of increase of thrombosis.
Focal symptoms develop when brain matter is involved in the process, i.e. with the development of cortical venous infarction. Cortical motor deficits, cortical symptoms, and seizures appear according to the location of the affected sinus.
When a clinical picture of thrombosis of the veins and sinuses of the brain occurs, MRI in most cases reveals signs of extensive areas of ischemia and hemorrhage. However, in some cases, standard neuroimaging methods fail to detect changes in the brain parenchyma.
The method of choice in such cases is magnetic resonance imaging (MRI) of the brain using MR venography.
Thrombosis of the right transverse sinus - hypointense areas on T2 (intracellular deoxyhemoglobin).
To confirm venous sinus thrombosis and determine the exact location and extent of the thrombus, MR venography is necessary.
MR venography – lack of visualization of blood flow in the right transverse sinus and jugular vein.
MRI of the brain: on the right (green arrow) the T2-weighted image shows the normal phenomenon of “empty flow” from the right sigmoid sinus and jugular vein. On the left (orange arrow) there is an abnormally high signal, most likely resulting from thrombosis. To confirm sinus thrombosis and definitively determine the location and extent of thrombosis, MR venography is necessary.
MR venography: thrombosis of the left transverse sinus. There is loss of MR signal from the left transverse sinus. The presence of sinus visualization on “raw” data or brain MRI confirms sinus thrombosis and excludes its hypoplasia.
MR venography: thrombosis of the right transverse sinus. There is loss of MR signal from the right transverse sinus. The presence of sinus visualization on “raw” data or MRI of the brain confirms sinus thrombosis and excludes its hypo- and aplasia.
Thrombosis of the right transverse sinus. Absence of the phenomenon of “empty flow” from the right transverse sinus on MRI of the brain. Absence of visualization of the right transverse sinus on MR venography.
As mentioned above, in cases of a clinical picture of cerebral venous thrombosis along the veins and sinuses, an MRI of the brain in some cases reveals an area of ischemia and hemorrhage.
MRI of the brain: a combination of vasogenic (orange arrow), cytotoxic edema and hemorrhage (green arrow) is noted. This MR picture, as well as the location of the pathological zone in the projection of the temporal lobe, makes us think about hemorrhagic venous cerebrovascular accident due to thrombosis of the vein of Labbe. Confirmation requires MR venography or contrast-enhanced MRI.
STENOSIS, AREAS OF PATHOLOGICAL EXTENSION AND HYPOPLASIA OF VENOUS STRUCTURES OF THE BRAIN
MRA picture of pronounced asymmetry of the venous network with a predominance and mild dilatation of the veins of the right hemisphere (transverse, sigmoid sinuses and jugular vein on the right); hypoplasia of the left transverse and sigmoid sinus. Single areas (2) of local dilatation of veins in the parasagittal parts of the left hemisphere, the great vein of the brain. Asymmetrical, dilated and clearly convoluted venous structure of the extracranial sections on the right.
MRA signs of slight dilatation of the superior sagittal sinus, local decrease in blood flow and narrowing of the lumen of the distal straight sinus; asymmetry of the lumen of the transverse, sigmoid sinuses and internal jugular veins.
VASCULAR MALFORMATIONS
Will an ultrasound of the neck vessels show a blood flow deficiency?
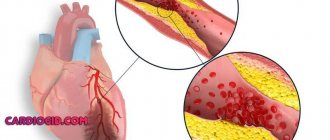
Blood flow deficiency is a very common pathology in the practice of neurologists and vestibulologists. A lot of people with headaches, constant dizziness and periodic fainting suffer from this disease. It occurs when, for one reason or another, the walls of the vessel narrow at the place where the right and left vertebral arteries inside the skull merge into one and together supply blood to the three main centers of the brain - the center of the vestibular apparatus, the center of vision, the center of hearing. Therefore, a lack of blood flow usually manifests itself as dizziness and tinnitus. Ultrasound can show the speed of blood flow in the vessels of the neck at different positions of the head. It is often important for neurologists to obtain data on the quality of blood flow in the carotid arteries. These vessels mainly supply blood to the cerebral cortex and subcortical structures. Thinking, memory, character, emotions and thought processes depend on how much oxygen the carotid arteries bring to the brain. If an ultrasound of the vessels of the neck shows a deficiency of blood flow in these arteries, the doctor must take urgent measures, since such a pathology can lead to loss of capacity. Basically, doctors encounter a deficiency of blood flow in the internal carotid arteries in post-stroke patients with one or more strokes in the past, in people who have suffered a heart attack, severe skull injury or several moderate concussions. Here, regular ultrasound of the neck vessels and MRI of the brain play an important role in assessing progress after therapy. Based on MRI and ultrasound data, the doctor can tell what and how the patient’s health has changed after treatment, and decide on a new form of therapy if the prescribed treatment is not enough and another course of other drugs is needed. In post-stroke patients, an ultrasound of the neck vessels will show how difficult the period after the stroke is, as well as how quickly or slowly the recovery is going.
| Service | price, rub. | Promotion Price |
| “Healthy Legs” program (duplex scanning of the veins of the lower extremities with assessment of valves and perforating veins and duplex scanning of the arteries of the lower extremities) | 3200 rub. | 3000 rub. |
| Ultrasound triplex scanning of N/C veins with assessment of valves and perforating veins | 2500 rub. | |
| Ultrasound triplex scanning of veins of the upper extremities | 2000 rub. | |
| Ultrasound triplex scanning of the arteries of the lower extremities with measurement of the brachial-ankle index (BAI) | 2000 rub. | |
| Ultrasound triplex scanning of the arteries of the upper extremities | 2000 rub. | |
| Ultrasound duplex scanning of the arteries of the aorto-iliac segment | 1900 rub. | |
| Ultrasound duplex scanning of the abdominal aorta and visceral arteries | 1900 rub. | |
| Ultrasound duplex scanning of the inferior vena cava | 1700 rub. | |
| Ultrasound duplex scanning of the iliac vein | 1700 rub. | |
| Ultrasound duplex scanning of the renal arteries | 1700 rub. | |
| Intracranial duplex of cerebral vessels | 2500 rub. | |
| Ultrasound of neck veins | 2500 rub. | |
| Ultrasound of the brachiocerebral arteries (BCA) | 2500 rub. | |
| Heart ultrasound or echocardiography for adults | 2400 rub. | |
| Comprehensive neck diagnostics (MRI of the cervical spine, MRI of neck vessels, ultrasound examination of neck vessels, ultrasound of the thyroid gland and soft tissues of the neck, consultation with a neurologist) | 13200 rub. | 9500 rub. |
Klippel-Trenaunay syndrome
This malformation of the deep veins is considered congenital; it usually affects the lower limbs in boys. The cause is compression of the deep veins by embryonic cords and muscles. The problem can also be caused by underdeveloped and narrowed veins. Already at birth, vascular spots are visible, and when the baby begins to walk, other symptoms will appear. The diseased leg is noticeably larger than the healthy one
, she has an unhealthy venous pattern. Due to the difference in legs, the pelvis is deformed. The skin of the limb may become ulcerated, sweaty and peeling.
Diagnosis of Klippel-Trenaunay syndrome involves duplex scanning, venography, etc. Treatment of the disease is surgical, it is usually carried out when the child reaches 3-5 years of age. During the operation, the cause of the compression is eliminated or the damaged vein is replaced with an autograft.
Will an ultrasound of the neck vessels show vascular compression?
Dynamic vascular compression is the bending of a vessel from the outside at a certain position of the head or body, which leads to a temporary deficiency of blood flow. Dynamic compression of the vertebral and subclavian arteries is a common cause of regular or spontaneous fainting, as well as headaches and sudden attacks of dizziness (fainting). This pathology is closely related to osteochondrosis of the cervical spine. When the vertebrae are displaced relative to each other to some extent and their displacement presses on the outside of the vessel, this narrowing of the vessel actually leads to stenosis, but not due to an atherosclerotic plaque, but due to compression. Such compression can be either permanent or temporary. Vascular ultrasound can easily diagnose temporary compression through rotary functional tests. During an ultrasound of the vessels of the neck, the blood supply is checked in dynamics:
- with head turns;
- with a tilt of the head;
- in a lying and sitting position.
The most common location of vascular compression is the area of the vertebral arteries of the neck. They run in the bony canal of the spine and are therefore often compressed when the cervical vertebrae are misaligned relative to each other. Sometimes a person develops an abnormal bone spur that grows towards the vessel and also puts pressure on it. Such conditions can lead to sudden loss of consciousness both from childhood and in adulthood, when this situation has increased due to osteochondrosis. Diagnosis of compression of neck vessels requires an integrated approach. Typically, the neurologist prescribes the patient to undergo an ultrasound of the neck vessels and an MRI of the cervical spine. It is the ultrasound of the cervical vessels that can show hidden temporary compression of the vessel, and the MRI of the cervical spine visualizes the causes of the clamps if they are related to the condition of the intervertebral discs and vertebrae.
Methods of treatment and prevention of mammary ectasia
The choice of treatment method for ectasia depends on the cause of the pathology. If the expansion of the milk ducts is associated with infectious inflammation of the gland, then antibacterial and antiviral medications are prescribed. If the pathology occurs due to excess prolactin or menopausal changes, then hormonal therapy is performed.
If pharmacological treatment is ineffective, then surgery is resorted to. Remove the affected areas or the entire duct completely. The indication for surgical intervention is the presence of a tumor and papillomas in the canal.
To prevent the development of pathology, women over 40 years of age need to undergo regular mammography examinations. It must be remembered that any injury to the mammary gland is very dangerous, so you need to protect your breasts from blows, bruises and concussions. It is important for patients to monitor the state of the body’s hormonal levels.
Breast ectasia is easily curable in the early stages. But in advanced cases, pathology can provoke the development of mastopathy and tumors. Therefore, if you experience chest pain and discharge from the nipples, you should urgently visit a mammologist.
Congenital anomalies of vascular development on ultrasound
Hypoplasia, that is, a small diameter of the vertebral arteries, is a fairly common finding in the practice of ultrasound diagnosticians. The most typical form of its manifestation is hypoplasia of one of the vertebral arteries with a decrease in blood flow in its basin. Often there is a high entrance of one or two arteries into the spinal canal, while part of the path of the vertebral artery is not protected by the bone canal and can be compressed when turning the neck. Less common are the absence of any of the vertebral arteries and hypoplasia of the carotid arteries. An ultrasound of the neck vessels will clearly show the presence of hypoplasia, but we will not always be able to say whether this is a congenital anomaly or an acquired narrowing of the vessel due to osteochondrosis. This pathology requires conservative vascular treatment in order to increase the general blood flow of the body so that compensation occurs at the expense of other arteries. The effectiveness of the treatment is usually monitored using a series of control ultrasounds of the neck vessels.
Parkes-Weber-Rubashov syndrome
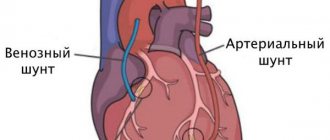
Veins can also dilate as a result of pathological arteriovenous connections and fistulas. The latter can be either congenital (this is Parkes-Weber-Rubashov syndrome) or acquired.
Fistulas in arteries and veins can be located in any organ or tissue, but most often they are detected in the extremities. The result of the disease is an increase in the cavities of the heart and the development of chronic heart failure
.
Symptoms of the pathology include dilated veins at the surface and a feeling of trembling upon palpation. Treatment of Parkes-Weber-Rubashov syndrome takes place in several stages, it all depends on the specific case. Angiosurgeons excise vessels, sometimes pathological vessels are stitched directly through the skin. Compression therapy is also necessary. In severe cases, limb amputation is indicated.
Will an ultrasound of the neck vessels show a tumor?
With an ultrasound of the vessels of the neck, doctors sometimes detect compression of the vessels by tumors.
First of all, it may be metastases of the lymph nodes of the neck. The peculiarity of metastatic tissue is that it is rigid, so it can compress the vessel or grow into its wall and form a tumor thrombus. All this is well visualized by a comprehensive ultrasound examination of the vessels of the neck and ultrasound of the soft tissues of the neck. Initial appointment with a NEUROLOGIST
ONLY 1800 rubles!
(more about prices below)
Symptoms of enlarged milk ducts
Signs of ectasia are usually pronounced. The shape of the nipples changes, they become flat, and sometimes even inverted. White discharge appears from the mammary glands. The area around the nipple swells and the skin becomes rough. The patient is bothered by pain, burning and itching.
Pathology can be detected using mammography and ultrasound of the mammary glands. They also do ductography - an X-ray of the mammary glands with the ducts filled with a contrast agent.
How does ultrasound show tortuosity and deformation of blood vessels?
Ultrasound of the vessels of the neck and head quite accurately shows changes in the shape and location of the arteries and the effect of these changes on blood flow. Most often in the practice of doctors, tortuosity of blood vessels occurs. Vascular tortuosity is an adaptation of the body to increased or unstable pressure and to various changes in the spine, which can sag in its height. This pathology is primarily associated with age-related characteristics or high blood pressure. In most hypertensive patients, ultrasound of the neck vessels will show either T-shaped or S-shaped tortuosity. Not all vascular tortuosity poses a threat to the health of patients. It is important for the neurologist to exclude loops and kinks in the arteries. The bending of the arteries at an acute angle is a kind of stenosis, which does not allow blood to pass through and requires surgical intervention. The results of the ultrasound scan will answer the question of whether this tortuosity is obstructing blood flow, since this determines the form and urgency of treatment. If the tortuosity severely deforms the vessel, when it bends at an acute angle or twists in a loop, the neurologist should refer the patient for a consultation with a vascular surgeon to decide on the need for surgical intervention.
Maffucci syndrome
This is a congenital disease associated with chondrodysplasia, varicose veins and hemangiomas. The expansion of veins in this pathology is uniform; hemangiomas are located on the fingers; if you squeeze them, they do not fall off; in addition, the patient will complain of pain during such manipulations. Another sign of the disease is bone curvature
.
The pathology is characterized by a long course. Treatment of Maffucci syndrome is only surgical; it is associated with the removal of angiomatous formations.
Chronic limb ischemia Dislocation of the thumb
Nonspecific Tokayasu aortoarteritis on ultrasound of neck vessels
Tokayasu nonspecific aortoarteritis manifests itself at a young age and leads to lifelong hormone therapy. This is a systemic inflammation of blood vessels, leading to thrombosis. Diagnosis of this disease is difficult because it can develop in any part of the human vascular system. Here, it is important for doctors to use ultrasound to identify inflammatory changes in the arteries as early as possible. To do this, a comprehensive examination is carried out - ultrasound of the vessels of the whole body, which will include:
- Ultrasound of the vessels of the neck and head;
- Ultrasound of vessels of the lower and upper extremities;
- Ultrasound of the abdominal aorta;
- Ultrasound of pelvic vessels;
- Ultrasound of renal vessels.
Author: Shogenov Ramish Kurbanovich
Neurologist with 10 years of experience