A healthy person does not feel the work of his heart in any way. And if heart rhythm disturbances occur, he may feel palpitations, interruptions or “loss of pulse.” The normal heart rate of an adult is from 60 to 90 beats per minute.
Tachycardia is an increase in heart rate to values exceeding 90 beats per minute. Often in such situations, patients complain of increased beating, “fluttering” or “jumping out” of the heart, they say that “the heart is pounding.” Of course, such a condition is a deviation from the norm.
What it is?
The human heart beats at a rate of 60-90 beats per minute.
These values are considered normal, and an increase in heart rate above 90 is usually called tachycardia. Contrary to popular belief, tachycardia is not always bad! The heartbeat may increase as a result of the body’s adaptation to changed environmental conditions. For example, exercise in the gym, being a physical activity, activates the sympathetic nervous system, which leads to an increase in heart rate and blood pressure. Another example is tachycardia in a patient with bleeding. Due to blood loss and a decrease in hemoglobin levels, hypoxia develops, the myocardium receives an insufficient amount of oxygen, and this causes an increase in heart rate.
Prevention
To prevent attacks of nocturnal tachycardia from occurring, the best way out is to reduce the load from both physical labor and emotions, adhere to an active lifestyle that can enhance the reserve capabilities of the human body and bring the pulse back to normal.
You need to take control of the number of hours spent motionless (at the computer), remove all “nicotine poisoning sessions” from the regime, and avoid drinking 8 cups of coffee a day, especially before going to bed.
It is better to avoid heavy meals before bedtime and reduce the amount of quickly digestible carbohydrates. The body should receive almost the entire daily dose of calories in the first half of the day. Before going to bed, you should not engage in physical activity; it is better to take a walk or take a relaxing shower.
Causes of rapid heartbeat
The reasons for this phenomenon may be different. Tachycardia can be physiological – the body’s reaction to irritating factors, and pathological – a manifestation of the disease.
In the first case, it occurs against the background of emotional excitement (stress) or as a result of increased physical activity (sports). People are taken by surprise and frightened by an increased heart rate, but the doctor’s task is to explain that a person’s heart rate does not remain constant throughout the entire time! We change and react to events around us: we get out of bed in the morning, go to work or to meet a friend, we are happy, we are upset - and all this is reflected in the heart rate through the activation of the autonomic nervous system.
Young boys and girls periodically turn to the therapist with complaints of high pulse. Their attacks are accompanied by autonomic reactions: sweating, pallor, increased blood pressure, sharp pain in the chest, panic attack with fear of death. Despite the pronounced clinical picture, after a comprehensive examination no pathology is detected. Such patients are given a mythical diagnosis of “VSD” and are recommended to take “Anaprilin” during an attack. The cause of this condition is disturbances in the functioning of the autonomic nervous system. Sessions with a psychotherapist help in this situation better than IVs in a hospital. Why? The answer is in the video link below.
Pathological causes of rapid heartbeat (tachycardia) are congenital or acquired diseases of the heart or other organs. These include: rheumatism, myocarditis, heart attack, developmental anomalies, thyrotoxicosis, anemia, neurosis and others. Patients with a rapid pulse may be aware of the presence of one of these problems. In such a situation, it is necessary to consult with a cardiologist about possible ways to eliminate tachycardia in your particular case. After all, a person with a diseased thyroid gland will not be able to get rid of a rapid pulse without adjusting the level of hormones, since changes in their concentration in the blood directly affect the heart rhythm.
After sleep and in the morning
“Sleep is the kingdom of the vagus” is a law of physiology. Activation of the vagus nerve through a complex neurohumoral mechanism causes a decrease in pulse and respiration, and a decrease in blood pressure. In the early morning hours, vagal activity decreases and the sympathetic nervous system comes into play. Stress hormones (adrenaline, cortisol) enter the blood, which leads to an increase in heart rate.
In addition, a sudden rise from bed can also cause tachycardia: after a long stay in a horizontal position, the baroreceptors do not have time to adapt to the vertical position of the body. The overall vascular resistance and pressure decrease, the return of blood to the heart decreases, which, according to the feedback mechanism, predisposes to the occurrence of tachycardia.
Nocturnal tachycardia
At night, the heart rate should normally slow down, but it doesn’t always happen as it should. The use of psychostimulants, drinking drinks that stimulate the central nervous system (wine, strong tea, coffee), watching a horror movie, neurosis, smoking, insomnia - all this can cause a rapid heartbeat. This is why sleep hygiene is so important; it is not recommended to drink coffee and tea after 16:00. In addition, you need to learn how to cope with stress so that negative emotions do not cause your heart rate to increase.
The cause of nocturnal tachycardia may be sleep apnea (short-term cessation of breathing). It is observed in persons with abdominal obesity, hypertension and snoring. The occurrence of apnea can provoke various rhythm disturbances: from blockades with asystole pauses to atrial fibrillation and ventricular tachycardia.
Fast heart rate at rest
A situation that should make you make an appointment with a doctor is a constant heart rate of more than 90 per minute at rest. Such tachycardia is almost always a symptom of a disease, and not necessarily of the cardiovascular system.
Chronic inflammatory disease, anemia or iron deficiency, thyroid disease, physical lack of training are the most common causes, the elimination of which will lead to normalization of the pulse.
Tachycardia can develop against the background of an acute infectious process: chills, an increase in body temperature by 1 degree increases heart rate by an average of 10 beats per minute. The use of adrenergic agonists (for example, for bronchial asthma or glaucoma), digoxin overdose, hypoxia (chronic and acute) also affect heart rate.
Rhythm under control
The doctor selects an antiarrhythmic treatment strategy. The main option for normalizing cardiac arrhythmias are antiarrhythmic drugs. Drug therapy is prescribed on a strictly individual basis. It depends on the form of tachycardia, existing chronic diseases and disorders, as well as on the causes that caused this condition! There are different groups of antiarrhythmic drugs depending on the main mechanism of action. Due to individual characteristics in the prescription of therapy, it is strictly forbidden to self-medicate. In difficult cases, urgent medical intervention is necessary to stop the attack.
Additionally, the cardiologist evaluates risk factors that may worsen the patient's condition. This may be family history, old age, arterial hypertension, some chronic diseases, lifestyle, etc. Simple rules for an adequate work and rest regime have a positive effect. This includes proper and restful sleep, good nutrition, limiting stressful situations, and the right approach to physical activity. If you have tachycardia, you should not smoke or drink alcohol. Alcohol and nicotine can independently affect the heart rhythm, and also become provocateurs of more serious pathologies. If palpitations occur, it is very important to always follow all doctor’s orders and regularly come for routine examinations. The specialist will evaluate the effectiveness of the prescribed therapy and clarify your well-being. Do not stop prescribed medications yourself. Only a cardiologist will help you choose the right tactics and take control of your heart rhythm.
The cardiologist at the EXPERT Clinic prescribes individual drug therapy only after a thorough assessment of the patient’s condition. A careful comprehensive approach and correct diagnosis guarantee effective treatment! Frequent heartbeat will no longer bother you.
Main symptoms
Tachycardia manifests itself in different ways; clinical symptoms depend on age and concomitant diseases. Rapid heartbeat may be accompanied by a feeling of discomfort in the chest, a drop in blood pressure, and weakness. There may be a feeling of shortness of breath, dizziness, darkening of the eyes, fainting. A patient with angina pectoris experiences chest pain as a result of an imbalance between the heart's increased oxygen demand and decreased O2 delivery. In people with heart disease, an attack of tachycardia is accompanied by a sharp increase in shortness of breath.
Features of the floors
There are no particular differences between the manifestations of tachycardia in men and women, except for autonomic reactions and emotional overtones.
The heart beats and bubbles in the throat, gives rise to fever, severe sweating, trembling in the body - this is how the signs of tachycardia in women are vividly described. They are more likely than men to have chronic non-paroxysmal sinus tachycardia - a disease when heart rate does not correspond to the level of physical activity or emotional stress. A possible mechanism for its development is considered to be an anomaly of the sinus node or increased automaticity of the heart.
Postural orthostatic tachycardia is also predominantly characteristic of women. It is accompanied by an inadequate increase in heart rate when the body position changes from horizontal to vertical.
Treatment
It is a common situation when cardiac pathology is the basis of the nightly “pranks” of the pulse. In this case, treatment aimed at getting rid of cardiac pathology will help. The main goal of therapy is to reduce the number of attacks and their severity. Indeed, in the presence of myocardial pathology, a violation of the rhythm of contractions gradually turns into a factor aggravating heart disease.
When the cause of night attacks is high blood pressure, the doctor prescribes antihypertensive drugs and determines the dose individual for the patient. As a rule, the evening dosage of the medication is increased. If the issue is sleep apnea, then everything is more complicated. Therapeutic measures in relation to it have a weak effect.
In all cases, doctors advise sleeping on your side. But sleeping people usually do not control the position of their own body in their sleep. For this reason, the only effective method is the use of special devices for ventilation. Such gadgets pressurize oxygen through a mask into the lungs of those sleeping.
To prevent your tongue from closing your windpipe at night, you can lose excess weight and cure ENT pathology. One hundred percent option: the doctor selects a gadget that fixes the position of the lower jaw while you sleep. Straining, changing body position, and taking a hot-cold shower will help quickly (but not for long) make tachycardia disappear.
Psychotherapy
The trigger for an increase in heart rate at night can be a mental injury, after which the patient wakes up for a long time, attacked by panic attacks. A qualified psychotherapist will help eliminate this problem. Beta-blockers and sedatives are indicated as medications.
General recommendations for nocturnal tachycardia - normalize sleep, increase the overall tone of the body
Clinical case
In my practice, there was a case of sinus tachycardia in a pregnant woman.
The woman constantly felt a rapid heartbeat, which was an adaptive reaction of the body: pressure decreased, heart rate increased; but the patient was also diagnosed with anemia. After correcting the hemoglobin level with iron supplements, her health improved and the feeling of palpitations disappeared. Although at first the woman was sincerely surprised when she was not prescribed drugs to slow down her pulse! Depending on the location of the source of excitation, tachycardias are divided into supraventricular and ventricular.
The first arise in the structures of the heart up to the level of branching of the trunk of the His bundle: in the atria, AV node, in additional conduction pathways. The source of origin of the latter is the His bundle, Purkinje fibers, and ventricular myocardium.
Based on the nature of the course, paroxysmal and non-paroxysmal types of pathology are distinguished.
According to the mechanism of occurrence - reciprocal, ectopic, with trigger activity, and so on.
Differential diagnosis of arrhythmias is a difficult and responsible task. In particular, when it comes to tachycardia with wide QRS complexes on the ECG. This may be a ventricular arrhythmia or tachycardia involving the accessory tract (accessory tract).
Ventricular tachycardia has a poor prognosis and occurs as a result of damage to the heart muscle. In contrast, arrhythmia involving the AP appears in a person without gross structural pathology of the heart.
To clarify the type of tachycardia, an ECG with an intrathoracic lead should be recorded or a transesophageal electrophysiological study should be performed. However, in real clinical practice, such an opportunity is rarely provided, and in these situations the doctor is guided by the following rule: assess the condition as the most dangerous to human health and life and begin appropriate treatment.
Expert recommendations
The doctor will conduct diagnostics, tests, interview the patient and prescribe an individual treatment regimen. First aid and self-help methods will help relieve an attack, but after it you still need to be examined. If the cause is not a serious pathology, then the doctor will prescribe:
- regular physical activity;
- clean water consumption rate;
- reducing consumption of fatty, sweet, fried foods;
- taking multivitamins.
In rare cases, maintenance medications and dietary supplements are prescribed to normalize the heart rhythm. To stabilize the condition, increase the body's resistance and endurance, physiotherapeutic methods are prescribed from hydrotherapy and balneotherapy to magnetic therapy.
Diagnostics: when and with what to see a doctor?
Any first-time attack of tachycardia that negatively affects your well-being is a reason to consult a doctor! And the more pronounced the clinical manifestations, the sooner you need to consult. If a person loses consciousness during a paroxysm, it is necessary to immediately call an ambulance and perform electrical cardioversion (impact of a pulsed current discharge on the heart).
Doctor's advice: check-up list for suspected tachycardia
To establish a correct diagnosis, the following studies and tests are necessary:
- electrocardiogram - at rest and at the time of rapid heartbeat;
- Ultrasound of the heart - data on the structural structure and valve apparatus;
- daily ECG monitoring;
- transesophageal EPI (TEPE);
- general blood test - will provide information about the presence of anemia and/or inflammation;
- blood test for thyroid hormones and TSH;
- consultation with an ENT doctor (if you have a history of frequent sore throats) and a dentist (caries) to identify and treat foci of chronic infection.
This is the minimum research that will help establish the cause of tachycardia, its nature and type, or allow you to choose a further diagnostic direction. Often, the doctor needs to seek help from fellow arrhythmologists who are able, using modern instrumental methods, to determine the area with pathological impulses. After its localization becomes known, the issue of minimally invasive destruction of the lesion can be decided.
If rapid heartbeat is the result of chronic tonsillitis, then by eliminating the cause (by performing surgical removal of the tonsils), you can forget about the heart problem. Such patients complain of pain in the heart area. Why chest discomfort occurs with a sore throat and how to act correctly - read here.
If the study reveals changes in thyroid hormone levels, or pheochromocytoma is suspected, then an endocrinologist will treat such a patient. It is worth noting that in clinical practice the first symptom of thyrotoxicosis is paroxysm of atrial fibrillation. Therefore, all patients with new-onset atrial fibrillation need to determine the concentration of thyroid hormones in the blood.
Monitoring a person with tachycardia first of all involves monitoring by a specialist who treats the underlying disease. It is a competent approach to the pathology that causes arrhythmia that will help get rid of unpleasant symptoms and minimize the consumption of medications.
How to choose a cardiologist
If you want to go to a medical institution for consultation because of rapid heartbeat, then first of all it is important to choose a clinic that has proven itself well. Advantages of the EXPERT Clinic:
- multidisciplinary medical center, which allows you to get advice from various specialists if necessary
- experienced and attentive cardiologists
- modern examination equipment, as well as practicing specialists in ultrasound and functional diagnostics
- the ability to quickly take all tests and provide examination results
- the most attentive attitude towards patients, only an individual approach, a detailed study of the problem
- convenience and comfort in the clinic, responsive medical staff.
Do not delay visiting a cardiologist, because timely identification of the main problem of “rapid heartbeat” can sometimes save your life.
How to relieve an attack of tachycardia: first aid
Vagal tests can be used as an emergency aid. Their meaning is to irritate the receptors of the parasympathetic nervous system, as a result of which the vagus nerve is activated. Performing these techniques will help either interrupt the paroxysm or lower the heart rate and reduce symptoms.
- Valsalva maneuver. While sitting or standing, take a deep breath, then pinch your nose, close your mouth and try to exhale, while straining the anterior abdominal wall.
- The cough reflex is simple to perform: the patient needs to cough.
- The gag reflex is to press on the root of the tongue.
- Squatting with straining.
- Diving dog reflex: hold your breath, pinch your nose and lower your face into a container of cold water.
- Carotid sinus massage. Prohibited for patients with atherosclerotic lesions of the carotid arteries and/or a history of stroke. It is carried out as follows: the pulsation point on the neck is determined and several pressures are applied on it for 3-5 seconds.
- Danini-Aschner test - pressure on the eyeballs; currently not recommended for use.
In addition to vagal tests, medications are used for emergency care. Verapamil is widely used, but its use is possible only when it is reliably known that there are no additional pathways in the myocardium. If atrial fibrillation has developed, then Propafenone, the “pill in your pocket” technique, can help. This drug is taken only if it has been previously successfully used in a hospital under the control of an electrocardiogram.
In my practice, during transesophageal pacing, patients often developed an attack of reciprocal AV nodal tachycardia. The use of vagal maneuvers (Valsalva and carotid sinus massage) made it possible to stop paroxysm. The entire process is demonstrated on the screen of the ECG installation: against the background of a smooth sinus rhythm, an attack of tachycardia with narrow QRS complexes suddenly occurs. This is accompanied by typical patient complaints (dizziness, nausea, darkening of the eyes, etc.), a massage of the carotid sinus is performed, and the attack suddenly ends.
If wide complex tachycardia develops during TEE, you can try to stop it using several electrical stimuli. The cessation of paroxysm in this way indicates the supraventricular nature of the arrhythmia. If the source is located in the ventricles of the heart, then stimulation will not affect the course of the attack in any way.
If you want to get quick, accessible and short information about frequent heartbeats, watch the video on our channel dedicated to this topic. Ask questions to experts in the comments.
Signs and warning signs
Conditions when you need to pay attention to your health and immediately consult a doctor:
- the appearance of shortness of breath (I can’t breathe);
- noise in the ears, cranium;
- dizzy;
- it becomes dark in the eyes;
- there is weakness up to loss of consciousness;
- heartache.
You must immediately call an ambulance, and while waiting for it you must:
- free the patient’s neck and chest from tight clothing;
- provide air access to the patient (open the window);
- apply cold to your forehead, rinse your face with very cold water.
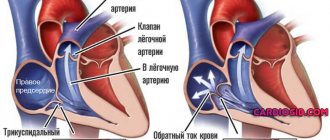
What are the symptoms of ventricular tachycardia?
What are the symptoms of ventricular tachycardia?
Due to the fact that during ventricular tachycardia, the contractions of the ventricles are not synchronized with the atria, a chaotic heartbeat occurs, which prevents sufficient filling of the heart chambers with blood, as a result of which the heart is not able to pump the required amount of blood to vital organs. This may lead to loss of consciousness. However, the clinical manifestations of ventricular tachycardia may vary. Sometimes short episodes of ventricular tachycardia may last seconds and not cause any noticeable symptoms. In other cases, a prolonged episode (usually more than 30 seconds) can lead to severe symptoms such as:
Palpitations Dizziness Shortness of breath Chest pain Loss of consciousness
Ventricular tachycardia sometimes poses a serious danger, leading to a more severe, life-threatening condition - ventricular fibrillation. This is a condition in which the ventricles of the heart seem to tremble and pump very little blood. Ventricular fibrillation is the most common cause of sudden cardiac death.
ATRIAL TACHYCARDIA
What types of atrial tachycardia can be distinguished? What are the electrocardiographic signs of atrial tachycardias?
Atrial tachycardias account for approximately 20% of all supraventricular tachycardias. According to the electrophysiological mechanisms of development, three types of atrial tachycardia are distinguished: automatic, triggered (post-depolarization) and reciprocal (re-entry). Reciprocal atrial tachycardias are more often paroxysmal, and automatic ones are chronic (constant or continuously recurrent). In addition, almost all researchers agree that in children, a violation of automaticity can be considered the predominant cause of the development of atrial tachycardia, and the arrhythmia itself is quite often persistent or chronic, lasting months and sometimes years, and can lead to the development of cardiomegaly.
Electrocardiographic diagnosis and clinical manifestations
Electrocardiographically, atrial tachycardias are characterized by the presence of a P wave, the shape of which usually differs from its morphology in sinus rhythm, located before the QRS complex of a supraventricular type (PR interval less than RP interval). The frequency of tachycardia in adults usually ranges from 140 to 180 beats per minute. With an increase in the frequency of the atrial rhythm, the PR interval may increase, and the P wave merges with the preceding T wave. Deterioration of atrioventricular conduction is sometimes accompanied by the development of second-degree AV block (Samoilov-Wenckebach period) without cessation of tachycardia, which distinguishes atrial tachycardia from most atrioventricular reciprocal tachycardia. Although, based on clinical and ECG data, it is difficult to distinguish automatic atrial tachycardia from arrhythmia developing by the re-entry mechanism, there are also a number of differential diagnostic signs. Automatic atrial tachycardia cannot be caused or stopped by pacing, which is precisely typical for reciprocal arrhythmias. Stimulation of the atria at a rate higher than the rate of automatic atrial tachycardia only temporarily suppresses the arrhythmia; after cessation of stimulation, it resumes.
The first P wave of automatic atrial tachycardia is similar to subsequent P waves. In reciprocal tachycardia, the shape of the atrial extrasystole complex, with which the attack usually begins, differs from subsequent P waves, the morphology of which depends on the location of the impulse circulation. In contrast to arrhythmias caused by the re-entry mechanism, the frequency of automatic atrial tachycardias often gradually increases. This phenomenon in electrophysiology is figuratively called “warms up”. In clinical practice, determining the electrophysiological mechanism of the development of atrial tachycardia is necessary, mainly, only when deciding on the use of cardiac pacing.
Vector analysis of the atrial ECG complex during tachycardia helps to establish its localization. A positive or biphasic P wave in lead aVL indicates the presence of an ectopic focus in the right atrium, while a positive P wave (“dome and dart”) in lead V1 and a negative one in leads V4-V6 indicate the origin of the arrhythmia from the left atrium.
Atrial tachycardia in some cases must be differentiated from sinus tachycardia. Differential diagnosis can be difficult, but it is important for choosing treatment tactics. Physical activity and vagal maneuvers significantly affect the frequency characteristics of sinus tachycardia and have little or no effect on them in atrial tachycardia. Long-term ECG recording in patients with chronic atrial tachycardia can reveal short periods of sinus rhythm (especially at night), which also helps in differential diagnosis.
Atrial tachycardias often develop in patients with organic heart disease. They are diagnosed with diseases such as coronary artery disease, myocardial infarction, arterial hypertension, heart valve lesions, dilated cardiomyopathy, cor pulmonale, etc. The role of digitalis intoxication, alcohol intake and hypokalemia in the appearance of atrial tachyarrhythmias is known. At the same time, a number of patients (primarily with automatic atrial tachycardia) are not diagnosed with cardiovascular diseases, which could be the cause of the arrhythmia.
In patients with atrial tachycardia, the prognosis is usually determined by the underlying disease. Mortality among them in the absence of other pathology other than heart rhythm disturbances is very low. However, if the arrhythmia occurs with high frequency and for a long time, then even in patients without organic heart damage, cardiomegaly develops, the ejection fraction decreases and congestive heart failure appears.
Treatment. Patients with asymptomatic, rare, short-lived paroxysms of atrial tachycardia do not require treatment. They need to be examined in order to identify the cause of the rhythm disturbance and eliminate it. Pharmacotherapy or non-drug treatment is necessary only for patients with severe attacks of arrhythmia, as well as in its chronic course, even in the absence of hemodynamic disturbances and good tolerance of the rhythm disturbance - due to the high risk of developing cardiomegaly and heart failure. Many cardiologists, when treating such patients, currently give preference not to antiarrhythmic drugs, but to interventional interventions, given their high effectiveness with a small number of complications.
Paroxysms of atrial tachycardia with unstable hemodynamics should be stopped by an EIT discharge of medium energies (50-100 J). Pharmacotherapy for atrial tachycardias has not been sufficiently developed, although, in principle, it is carried out as for other atrial tachyarrhythmias. When hemodynamics are stable, to reduce high heart rate, drugs that worsen atrioventricular conduction are used: calcium antagonists (verapamil, diltiazem), beta blockers, cardiac glycosides, or a combination thereof. The effectiveness of these drugs in terms of restoring and maintaining sinus rhythm is low. If the paroxysm remains, then restoration of sinus rhythm is carried out with the intravenous administration of antiarrhythmics of classes 1A, 1C and III (procainamide, propafenone, amiodarone, sotalol, etc.), and in case of reciprocal atrial tachycardia, pacing can be used for this purpose.
In order to prevent repeated attacks of arrhythmia, according to our experience and literature data, first of all, drugs of classes 1C and III (propafenone, flecainide, encainide, amiodarone, sotalol) should be used; class 1A antiarrhythmics such as quinidine, disopyramide, procainamide are less effective, ajmaline [1, 2, 3]. K. Koike et al. (13), having assessed for several years the effectiveness of 5 antiarrhythmic drugs of various classes, as well as digoxin and its combinations with propranolol, metoprolol, quinidine for automatic atrial tachycardia in children, they came to the conclusion that it is advisable to begin therapy for this cardiac arrhythmia with sotalol, since in 75% of cases it restored sinus rhythm or significantly reduced the frequency of ventricular contractions. If it is ineffective or there are contraindications, according to the authors, it is necessary to use class 3 antiarrhythmics (with the exception of ethmosin, which is ineffective with ALART) or amiodarone. Chronic atrial tachycardia in most cases is difficult to respond to mono- and combined antiarrhythmic therapy. EIT in this case is also ineffective. If antiarrhythmics do not work, in patients with chronic atrial tachycardia it is necessary to reduce the ventricular rate to prevent the development of congestive heart failure. For this purpose, verapamil, diltiazem, cardiac glycosides or even amiodarone are used (combinations of these are possible); in addition, the issue of non-drug treatment should be addressed.
Radiofrequency catheter destruction has been successfully used to treat atrial tachycardia, regardless of the electrophysiological mechanism of its development (automatic, triggered or reciprocal) and localization (right or left atrium). The main indication for radiofrequency catheter destruction is the ineffectiveness of pharmacotherapy or the patient's reluctance to take antiarrhythmic drugs for a long time. In the USA, according to some data, the effectiveness of such an intervention is 75%, and the number of complications is 0.8% [4]. Destruction of the atrioventricular connection with implantation of a pacemaker or its “modification” (partial destruction) is carried out if radiofrequency catheter destruction of the arrhythmia focus is ineffective or impossible. In patients with symptomatic recurrent supraventricular tachycardias that are controlled by pacing, in whom drug treatment and radiofrequency catheter destruction have been ineffective, implantation of an antitachycardial pacemaker is possible. Surgical interventions (isolation, resection or destruction of the arrhythmogenic zone) are now rarely performed in case of failure of radiofrequency catheter destruction or if another cardiac surgery is planned.
Sinoatrial reciprocal tachycardia
One of the forms of atrial tachycardia, which is somewhat different in its clinical course, electrophysiological and ECG diagnostics, as well as pharmacotherapy, is sinoatrial reentrant tachycardia (sinus nodal reentrant tachycardia). The development of sinoatrial reciprocal tachycardia is associated with the circulation of an excitation wave in the sinus node with the inclusion in some cases of a nearby section of the right atrium myocardium in the circulation circuit.
This arrhythmia, as a rule, is paroxysmal in nature, and the heart rate varies from 100 to 220 beats per minute, but in general it is less than with other supraventricular tachycardias, and in most cases does not exceed 150 beats per minute. Attacks of tachycardia in this case are most often short (from 5-20 complexes to several minutes), prolonged attacks are observed very rarely. It is difficult to talk about the true prevalence of sinoatrial reentrant tachycardia. The frequency of detection of sinoatrial re-entry, according to most researchers, ranges from 2 to 10% among all supraventricular tachycardias. There is much less data indicating its wider distribution. Thus, SART was diagnosed in 11 of 65 patients (16.9%) with supraventricular tachycardias who underwent intracardiac electrophysiological study [5].
Since the mechanism of development of sinoatrial reciprocal tachycardia is associated with the re-entry of the excitation wave, it is successfully caused and stopped by extrastimulation of the atria (sometimes even the ventricles) and increased stimulation of the atria. Unlike most atrial tachycardias, the P wave located before the QRS complex is identical or very similar to that recorded during sinus rhythm. The PR interval is shorter than the RP interval. The sudden onset and, in most cases, the sudden cessation of an attack, as well as the possibility of stopping it with vagal techniques (sinus tachycardia and PRT do not stop with them) can serve as important differential diagnostic signs of sinoatrial reciprocal tachycardia.
Since the frequency of attacks with sinoatrial reentrant tachycardia is usually small, and the attacks themselves are short-lived, it may be asymptomatic and do not require treatment. Curative and prophylactic antiarrhythmic therapy for symptomatic sinoatrial reciprocal tachycardia is similar to that carried out for atrioventricular junctional reciprocal tachycardia. Relief begins with vagal maneuvers (Valsalva maneuver, carotid sinus massage), and if there is resistance to them, antiarrhythmics are administered intravenously: ATP 10-20 mg (adenosine 6-12 mg, very quickly) or calcium antagonists (verapamil 5-10 mg or diltiazem 0.25-0.35 mg/kg for 2 minutes). Possible IV use of digoxin, beta blockers and amiodarone. If the patient's condition is unstable (severe anginal pain, significant decrease in blood pressure, cardiac asthma or pulmonary edema), emergency electrical cardioversion is performed (first shock with a power of 50-100 J). Paroxysms of tachycardia can be successfully stopped by cardiac pacing. To prevent attacks of sinoatrial reciprocal tachycardia, verapamil, diltiazem, beta-blockers, digoxin, as well as class III antiarrhythmic drugs - amiodarone and sotalol are primarily used. There are reports of the effective use of radiofrequency catheter destruction of the source of arrhythmia.
Multifocal (chaotic) atrial tachycardia
Multifocal atrial tachycardia is diagnosed in 0.13-0.4% of hospitalized adult patients. It most often affects older people (the average age is more than 70 years). This rhythm disturbance is recorded in approximately equal proportions in men and women. More than 60% of patients with multifocal atrial tachycardia are diagnosed with pulmonary disease. Chronic obstructive pulmonary diseases are the most common. Less commonly, arrhythmia acts as a complication of acute pneumonia, pulmonary embolism, and lung tumors. Medicines such as aminophylline and isoproterenol, used in the treatment of chronic obstructive pulmonary diseases, can play a role in the occurrence of arrhythmia, and also cause its more severe course. In addition to pulmonary pathology, such patients often have cardiovascular diseases (coronary artery disease, hypertension, less commonly valvular heart disease, etc.), accompanied by congestive heart failure. It is important to note that in many cases (according to some data, up to 70%), disorders of carbohydrate metabolism accompany multifocal atrial tachycardia. Mortality among adult patients with multifocal atrial tachycardia is high and ranges from 29-62%. The cause of death is usually severe illness, which affects most patients with multifocal atrial tachycardia, and not the rhythm disorder itself.
Electrocardiographic criteria for diagnosing multifocal atrial tachycardia are:
- the presence of three or more P waves of different morphology in one ECG lead;
- the presence of an isoline between the P waves;
- irregular PR, PP and RR intervals.
The shape of the P waves depends on the location of the ectopic focus of the arrhythmia and changes in intraatrial conduction.
Most often, multifocal atrial tachycardia must be differentiated from atrial fibrillation. In contrast to the latter, with multifocal atrial tachycardia, P waves of changing shape and the isoline between them are clearly visible.
In the management of patients with multifocal atrial tachycardia, an important place is occupied by the treatment of the underlying disease and the correction of factors predisposing to its development: combating infection during exacerbation of chronic pulmonary disease, treatment of heart failure, normalization of acid-base balance and electrolyte disturbances, streamlining the use of beta-adrenergic receptor agonists and methylxanthine derivatives. These measures sometimes make it possible to normalize the rhythm even without the use of antiarrhythmic drugs.
Antiarrhythmic therapy of multifocal atrial tachycardia is associated with great difficulties. Some studies have shown the ineffectiveness of quinidine, procainamide, lidocaine and phenytoin. Cardiac glycosides are also ineffective and often cause intoxication due to the presence of hypoxia and a number of severe metabolic disorders in patients. Electropulse therapy does not restore sinus rhythm and is therefore ineffective.
An analysis of works on antiarrhythmic treatment of multifocal atrial tachycardia shows that the most effective in slowing down, converting the rhythm and preventing relapses of arrhythmia are probably verapamil, beta-blockers (however, they are contraindicated in patients with bronchospastic syndrome) and amiodarone [6, 7, 11]. There is a small number of studies examining the effect of class 1C artriarrhythmics on multifocal atrial tachycardia. Thus, in particular, we describe a case of tachycardia relief due to intravenous administration of flecainide to a 57-year-old patient in whom verapamil, metaprolol, sotalol, disopyramide and some other antiarrhythmic drugs were ineffective [8]; the possibility of successful parenteral and oral use of propafenone for this type of arrhythmia in pediatric practice has been shown [9]. Interesting data were obtained regarding the high stopping effectiveness of magnesium sulfate (in some cases in combination with potassium preparations): in 7 out of 8 patients with multifocal atrial tachycardia (87.7%), sinus rhythm was restored when administered intravenously for 5 hours from 7 to 12 g MgSO4. It should be noted that a decrease in the level of magnesium and potassium in the blood plasma was observed only in 3 patients [10].
Thus, it is advisable to start pharmacotherapy of multifocal atrial tachycardia with beta-blockers (if there are no contraindications to them) or verapamil; if they are ineffective, use amiodarone and class 1C antiarrhythmics, and to relieve arrhythmia, intravenous administration of magnesium sulfate is also possible.
Literature
1. Pongiglione G., Strasburger JF, Deal BJ et al. Use of amiodarone for short-term and adjuvant therapy in young patients // Am. J. Cardiol. 1991; 68: 603-608. 2. Zeigler V., Gillette PC, Ross AB et al. Flecainide for supraventricular and ventricular arrhythmias in children and young adults // Am. J. Cardiol. 1988; 62:818-820. 3. Colloridi V., Perri C., Ventriglia F., Critelli G. Oral sotalol in pediatric atrial ectopic tachycardia // Am. Heart J 1992; 123: 254-256. 4. Scheinman MM Patterns of catheter ablation practice in the United States // Pacing Clin. Electrophysiol. 1994; 17: 873-877. 5. Gomes JA, Hariman RJ, Kang PS et al. Sustained symptomatic sinus node reentrant tachycardia: incidence, clinical significance, electrophysiologic observations and the effects of antiarhythmic agents // J. Am. Coll. Cardiol. 1985; 5: 45-57. 6. Scher DL, Arsura EL Multifocal atrial tachycardia: mechanisms, clinical correlates and treatment // Am. Heart J 1989; 118: 574-580. 7. Arsura E., Lefkin AS, Scher DL et al. A randomized, double-blind, placebo-controlled study of verapamil and metoprolol in treatment of multifocal atrial tachycardia // Am. J. Medicine. 1988; 85:519-524. 8. Creamer JE, Nathan AW, Camm AJ Successful treatment of atrial tachycardias with flecainide acetate // Br. Heart J 1985; 53: 164-166. 9. Reimer A., Paul T., Kallfelz H.-C. Efficacy and safety of intravenous and oral propafenone in pediatric cardiac dysrhythmia // Am. J. Cardiol. 1991; 68:741-744. 10. Iseri LT, Fairshter RD, Hardemann JL, Brodsky MA Magnesium and potassium theraphy in multifocal atrial tachycardia // Am. Heart J 1985; 110: 789-794. 11. Olgin JE, Zipes DP Specific arrhythmias: diagnosis and treatment. In Braunwald E. (eds). Heart disease. A textbook of cardiovascular medicine. Philadelphia: WB Saunders company. 2001. P. 837.