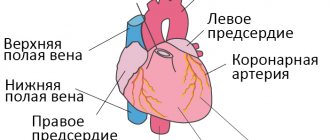
Heart failure (HF) is a pathological condition caused by the failure of the heart as a pump that provides adequate blood circulation. Manifestation and consequence of pathological conditions affecting the myocardium or complicating the work of the heart: coronary heart disease, heart defects, arterial hypertension, diffuse lung diseases, myocarditis, myocardial dystrophy (including thyrotoxic, sports, etc.), myocardiopathy (including alcoholic) and etc.
Acute heart failure can be either acute itself, or it can be an acute manifestation of chronic heart failure.
Why does vascular insufficiency occur?
The causes of the pathological condition are often hidden in the aging of the body.
Every year the vessels weaken, their walls lose their tone and natural elasticity. People with hypertension are at greatest risk. A constant increase in pressure leads to the fact that the blood vessels narrow, the rate of contraction of the heart muscle increases, and its hypertrophy develops. Therefore, in order to avoid acute vascular insufficiency, doctors at the Euromedprestige clinic recommend promptly identifying the symptoms of hypertension and undergoing appropriate treatment. In elderly patients, pathology may appear against the background of concomitant diseases:
- heart defects;
- IHD;
- myocardial infections.
An attack can be triggered by pneumonia, purulent appendicitis, or sepsis. Sometimes collapse occurs against the background of a rapid decrease in pressure resulting from chemical or mushroom poisoning. Severe blood loss, large area burns, and electric shock are also provoking factors in the development of the pathological condition.
Causes of CCVN
{banner_banstat2}
The causes of cerebral pathogenesis are divided into main and additional.
Main factors:
- developing atherosclerosis of cerebral vessels;
- diabetes mellitus, gout;
- hiertonia.
Additional factors:
- alcohol abuse;
- smoking;
- predominance of fatty foods in the diet;
- sedentary lifestyle;
- hereditary causes;
- inflammatory infections;
- neck osteochondrosis;
- diseases of the cardiac system;
- overweight;
- increased blood clotting;
- previous injuries;
- poisoning with various chemicals;
- emotional stress (stress, anxiety).
Types of disease
According to the distribution of the pathological process, the following types of cardiovascular failure are distinguished:
- Regional – occurs when there is a circulatory disorder in the peripheral vessels.
- Systemic – appears when there is a disturbance in the general blood flow.
Based on the rate of increase in symptoms, the pathology can be acute or chronic. In the first case, its symptoms appear rapidly due to a sharp drop in pressure. The chronic type of condition takes a long time to develop, and its “provoker” is usually a persistent decrease in blood pressure less than 100/60. Chronic failure can be primary (caused by disorders of the autonomic system) and secondary (due to various diseases).
Symptomatic manifestations
{banner_banstat1}
Cerebrovascular disease is a pathological change in the blood vessels of the brain that provokes a violation of the circulation of cerebral blood flow. The pathology is preceded by atherosclerosis and hypertension, and its consequence is a stroke with disability or death.
The etiology of the disease is expressed in the slow narrowing of small arteries in the brain, the development of focal ischemia of the white medulla. Symptoms of cerebrovascular disease are as follows:
- constant headaches;
- tinnitus;
- attacks of dizziness;
- decreased field of vision, spots before the eyes;
- mental dysfunctions (impaired thinking, memory, decreased attention, insomnia, trembling fingers, slow speech);
- change in behavior (lethargy, apathy, causeless irritability and resentment);
- pathological lesions of most of the brain, expressed in impaired coordination of movement, paralysis, speech and memory disorders, signs of parkinsonism, dementia.
Cerebrovascular disease is divided into acute and chronic forms.
Acute types of CVD:
- acute encephalopathy of the hypertensive type;
- transistor ischemic crisis;
- hemorrhagic or ischemic stroke.
The chronic form of cerebrovascular pathology is discircular encephalopathy, which is divided into the following types:
- cerebral vascular thrombosis - vascular obstruction due to blockage of the lumen by blood clots or atherosclerotic plaques;
- cerebral embolism - blockage of small vessels by emboli that have broken off from large vessels;
- brain bleeding caused by a ruptured vessel (hemorrhagic stroke);
- discircular encephalopathy with subsequent transition to the acute form of CVD.
Symptoms of vascular insufficiency
Characteristic manifestations of acute vascular insufficiency are shock, fainting or collapse. The difference between them consists mainly in the absence or presence of a disorder of consciousness, however, each condition also has its own characteristic symptoms:
- Fainting is characterized by the suddenness of its appearance, a sharp deterioration in general health, and autonomic disorders. Usually a person feels increasing weakness, discomfort, nausea, and then loses consciousness for a while. As the pathological condition develops, pale skin, ringing sounds in the ears, and a feeling as if the earth is disappearing from under one’s feet are observed.
- Collapse is associated with a decrease in the volume of circulating blood and a deterioration in vascular tone. Symptoms of vascular insufficiency in such a situation manifest themselves in the form of weakened vision and a feeling of thirst. The person remains conscious, but his skin turns pale, his face takes on a sallow color, and his fingers, lips and the tip of his nose become bluish. The pathology is characterized by indifference to everything around, a feeling of melancholy and shallow breathing.
- Shock is a complex pathological process caused by a sharp decrease in blood flow against the background of extreme influences (electric shock, burns, severe injuries, etc.). The clinical picture of shock is almost similar to collapse, but it goes through several stages, and at the last (terminal) the actions of doctors may not produce results.
Degrees of pathology
{banner_banstat0}
CCVD is a gradual disorder of brain activity that causes severe symptoms of brain cell damage due to insufficient blood circulation in the brain. The pathology mainly affects older people over 50 years of age.
There are 3 degrees (stages) of the clinical course of the disease:
- Initial stage (1st degree). Symptoms: headaches, dysfunction of the vestibular apparatus (unsteady gait), insomnia, memory impairment, fatigue and decreased performance. Changes in the structure of the fundus occur (retinal angiopathy), increased blood pressure, and cardiac arrhythmia.
- In the middle stages (grade 2) of vascular dementia, a decrease in mental and intellectual abilities, sclerosis of cerebral vessels, and changes in the structure of the brain fluid are observed.
- At the last stage (3rd degree) of chronic CVN, patients are assigned a disability due to pronounced signs of mental impairment.
Often the disease is accompanied by attacks of stroke, myocardial infarction and cardiac arrhythmia.
Diagnosis and assistance
When treating pathologies of the cardiovascular system, doctors conduct a thorough diagnosis of the patient and provide qualified assistance according to the identified problems.
Diagnostics
The main diagnostic measures in the development of a pathological condition are aimed at examining the patient, assessing his symptoms and determining the form of deficiency. To give an accurate conclusion, a specialist studies the person’s history and determines what factors could lead to the pathology. After assistance is provided, the patient is sent to a hospital, where examinations of the circulatory and cardiac systems are prescribed:
- ECG;
- phlebography;
- auscultation (listening) of arterial vessels;
- sphygmography, etc.
Our clinic has all the necessary equipment for diagnostics, which allows us to accurately determine the etiology of the pathological process.
First aid
Help for acute vascular insufficiency should be provided without delay. If you faint, do the following:
- the person is laid horizontally;
- loosen the collar of clothing for air access;
- splash your face with water;
- give ammonia to smell;
- call an ambulance.
Upon arrival, the doctor injects the patient with caffeine or adrenaline and then admits him to a medical facility. If shock develops, it is necessary to urgently take the person to the hospital. The faster his resuscitation is performed, the lower the risk of death. If necessary, stop the bleeding and carry out other procedures, focusing on the reasons that led to the attack.
Chronic cerebrovascular insufficiency
Etiology and pathogenesis
Chronic cerebrovascular insufficiency (CVI) is the most common variant of vascular-cerebral pathology (in foreign literature there is an illogical term “cerebrovascular diseases”, which can be used in cases where the brain is primarily affected and the innervation of the vascular system is secondarily disrupted with clinical disorders, for example, the neurogenic stage of hypertension, vegetative-vascular dystonia, etc.). The most common etiological factors of vascular damage are atherosclerosis, hypertension and their combination, diabetes mellitus, vegetative-vascular dystonia, vasculitis in systemic connective tissue diseases (lupus erythematosus, etc.), syphilis, tuberculosis, blood diseases with an increase in its viscosity (erythremia , macroglobulinemia, etc.).
The following stages of chronic cerebrovascular insufficiency are distinguished: initial manifestations of cerebral circulatory failure and dyscirculatory encephalopathy.
Initial manifestations of cerebrovascular insufficiency (CBF)
develop when the cerebral blood flow rate decreases from 55 ml/100 g/min (normal) to 45-30 ml/100 g/min. Clinical symptoms (complaints) are short-term dizziness and feelings of instability when walking or sudden changes in body position, a transient feeling of heaviness in the head, increased fatigue, decreased speed of thinking and memory, and sleep disorders. From time to time headaches and noise in the head appear. Such symptoms first occur after physical or emotional stress, alcohol consumption, hunger, or changes in meteorological factors.
When examining the neurological status, signs of focal damage to the nervous system are not detected. Neuropsychological examination reveals a slowdown in thinking when solving intellectual problems, and mild impairment of cognitive functions.
Encephalopathy
is a multifocal brain lesion due to a decrease in blood flow to the brain ranging from 35 to 20 ml/100 g/min. Typically, discirculatory encephalopathy (DE) develops against the background of general vascular pathology. The following forms are distinguished: atherosclerotic, hypertensive, venous and mixed.
Based on the severity of neurological disorders, 3 stages of dyscirculatory encephalopathy are distinguished.
Stage I is characterized by a decrease in attention, memory (primarily for current events - memorization of new information is impaired), increased fatigue, and decreased ability to work. new information), increased fatigue, decreased ability to work. It is difficult for the patient to concentrate and switch from one activity to another. There is a dull headache, which intensifies with prolonged mental stress and excitement. Sleep is disturbed. Periodically, dizziness and staggering occur when walking. Emotional lability and decreased mood are observed.
When examining the neurological status, revival of reflexes of oral automatism, anisoreflexia of deep reflexes in the arms and legs are revealed against the background of their moderate increase without a decrease in muscle strength, moderate impairments of attention and memory. Working capacity has been preserved.
In stage II , personal changes appear in the form of viscosity of thinking, getting stuck on trifles, selfishness, touchiness, irritability, narrowing the range of interests and needs; Memory disorders increase, the ability to generalize and abstract, and associative thinking decreases. It is difficult to fall asleep, sleep is short and intermittent. Patients often complain of a dull headache, darkening of the eyes with a sudden change in the position of the body and head, dizziness, and instability.
In the neurological status, along with pseudobulbar signs and anisoreflexia, akinetic-rigid syndrome and vestibulo-cerebellar disorders are detected. Working capacity and social adaptation decrease.
Stage III is characterized by worsening symptoms and signs of the previous stage. Signs of pseudobulbar paresis, pyramidal insufficiency with decreased muscle strength, extrapyramidal and cerebellar dysfunction are increasing. Criticism towards one's own state decreases, weakness of spirit (tearfulness) is noted. Control of the sphincters of the pelvic organs is impaired. Cognitive disorders become severe to the point of dementia, and the development of apato-abulic syndrome and epileptic seizures is possible. There is severe drowsiness after eating (pollakihypnia; from the Greek pollakis - often, hupnos - sleep). Headache, dizziness and memory disorders are often combined (Windscheid's triad). The patients are incapacitated and have signs of severe disability (group I).
Diagnostics
chronic cerebrovascular insufficiency is based on clinical data and additional studies of the vascular system and brain. In the fundus, vascular atherosclerosis and pallor of the optic disc are detected. The tortuous and compacted temporal arteries, compacted common, external and internal carotid arteries at the level of the neck are palpated. Rheoencephalography with functional tests (with nitroglycerin, hyperventilation for 3 minutes, turning and tilting the head, etc.), Doppler ultrasound with its variants (extracranial, transcranial, duplex scanning, ultrasound angiography, etc.), magnetic resonance imaging of the brain is performed. and the vessels supplying it (extra- and intracranial), carotid, vertebral or panangiography, X-ray examination of the aorta and large vessels. Useful information can be obtained from a biomicroscopic examination of the vessels of the conjunctiva, a biochemical study of lipid metabolism, as well as from an electroencephalogram and electrocardiogram. Often atherosclerosis of cerebral vessels is combined with atherosclerosis of the coronary arteries and vessels of the lower extremities.
Differential diagnosis
carried out in order to exclude brain pathologies of other origins and diseases of internal organs in which the function of the nervous system is secondarily affected (diabetes mellitus, damage to the liver, kidneys, lungs, gastrointestinal tract, etc.).
Treatment and prevention
When the first signs of chronic cerebrovascular insufficiency appear, periodic courses of treatment should begin to prevent progression of the disease. At the same time, primary prevention of atherosclerosis and vascular diseases of the nervous system should be organized by general practitioners (local therapists, family doctors, in large enterprises - workshop therapists), who explain the rules of a healthy lifestyle, including diet, self-regulation of work, rest and sleep patterns , adequacy of physical activity, skills and methods of relieving psycho-emotional stress, etc. Drug therapy for initial manifestations of insufficiency of cerebral blood supply is prescribed together with a therapist, taking into account the entire somatic status. Prescribed courses of vasoactive drugs (Cavinton, vinpocetine, cinnarizine, etc.), antisclerotic agents that improve blood rheology, and antiplatelet agents (acetylsalicylic acid and its derivatives, Wessel Due F, chimes, etc.), nootropic and neuroprotective drugs, including those containing amino acid complexes (actovegin, cortexin, glycine, etc.), antihypoxants, tranquilizers, vitamins B, E, etc.
Patients often have a fairly pronounced pathology of the cardiovascular system (hypertension, atherosclerosis), with coronary insufficiency, diabetes mellitus, obesity, I tereotoxicosis, etc., which requires the selection of additional combinations of drugs. In this regard, the doctor must remember and explain to patients: it is better to carry out the planned treatment with one drug for the full course of taking it, then after a short break (7-10 days) start taking another drug - and so on consistently for an unlimited time. If on the same day there is a need to take other drugs to correct the impaired function of internal organs, then taking the drugs should be separated by at least 30 minutes. It is strictly inadvisable to swallow 2 or more medications at the same time, since their interaction in the stomach is unpredictable, and this often leads to a decrease in the therapeutic effectiveness of each of the drugs taken and allergic reactions to medications.
If signs of cerebrovascular insufficiency appear, you should refrain from overheating (in the sun, in a sauna), climbing mountains more than 1000 m above sea level, consuming tobacco, alcohol (more than 30 ml of alcohol), strong tea and coffee (more than 2 portions per day), physical overload, prolonged exposure to TV, personal computer (no more than 45 minutes).
Measures to prevent cerebrovascular insufficiency should be carried out from adolescence (primary prevention) and be aimed at correcting risk factors: obesity (overeating, large meals in the evening), physical inactivity, smoking, abuse of alcohol and other drugs, stress, etc., and also to prevent exacerbations of the disease, repeated acute cerebrovascular accidents (secondary prevention).
Prevention of vascular insufficiency
Preventive measures to prevent vascular insufficiency consist of preventing diseases that can cause the pathological condition. It is necessary to adhere to a healthy diet, control blood pressure, and if you have hypertension, take medications prescribed by your doctor. It is advisable to give up bad habits and foods rich in cholesterol. Regular walks and exercise are recommended.
If symptoms of heart or vascular diseases appear, you should immediately contact a specialist to diagnose and treat them. The Euromedprestige clinic is ready to conduct a comprehensive examination and help you avoid the development of pathology.
Treatment of CVD
{banner_banstat4}
The main goal of therapy is the regeneration and normalization of blood circulation in the brain, aimed at expanding the lumen of blood vessels.
Cerebrovascular disease is treated comprehensively, using various methods of therapy.
Drug treatment is carried out in the following areas:
- vasodilators (Mefakor, Papaverine) and anticoagulants (Apirin, Curantil, Cardiomagnyl, etc.);
- nootropic drugs for restoring memory and cognitive activity of the brain (Cinnarizine, Stugeron, Nootropil, Piracetam, Cavinton, etc.)
- antihypertensive drugs;
- drugs for weight normalization.
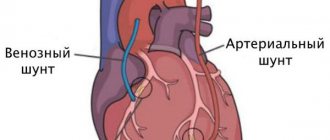
Surgical operations:
- in case of vascular obstruction, angioplasty is used - a catheter with a balloon is inserted;
- removal of blood clots (endarterectomy);
- insertion of stents into the walls of arteries that protect against narrowing (stenting).
Physiotherapeutic procedures:
- physiotherapy;
- massage;
- electrophoresis;
- ultrasound.
Non-medical treatment - speech therapy sessions, psychological consultations.
Determination of disability in patients with disulatory encephalopathy:
- At the initial stage (grade 1) of CSVD, patients remain able to work.
- The middle stage (2nd degree) implies assignment to patients of disability group II-III. Disability may be temporary due to concomitant ailments or during an exacerbation of chronic circulatory failure.
- Severe stage (grade 3) CCVP causes complete loss of ability to work. Patients are assigned disability groups I-II.