Ultrasound of cerebral vessels is an absolutely painless technique that helps to identify possible pathological processes. It has been scientifically proven that ultrasonic waves do not have a negative effect on organs and tissues, therefore such manipulation can be carried out not only for diagnosis in adults, but also in children. The number of procedures and frequency of examinations are not limited - ultrasound can be performed as often as necessary. Brain examination using ultrasound is carried out both according to the doctor’s indications and at the request of the patient. Let's look at how an ultrasound is performed and how to properly prepare for it.
In what cases is ultrasound of the brain prescribed?
Of course, you can undergo the examination without any complaints. But there are a number of symptoms that indicate that the procedure should not be postponed.
Be sure to consult your doctor if any of the following concerns you:
- Constant feeling of drowsiness and weakness;
- Dizziness, darkening of the eyes with a sharp rise;
- Noise in ears;
- Regular headaches or headaches that occur in the morning;
- Flashing “flies” before the eyes;
- Difficulty in perceiving information (reading or listening);
- Problems paying attention or remembering;
- Blood pressure surges;
- Episodes of incoordination;
- Apathy or low mood;
- Unreasonable nausea and vomiting;
- Deterioration of vision or hearing.
For preventive purposes, ultrasound is also indicated for those people who have high cholesterol or blood sugar levels, as well as people suffering from obesity, the elderly and those who have previously suffered a heart attack or stroke.
Sometimes ultrasound of cerebral vessels is prescribed before an upcoming operation, for example, if tumors in the head area are to be removed.
Main arteries of the head
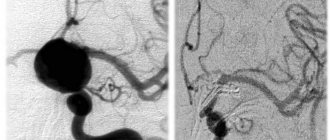
Angiography of the main arteries of the head
is an instrumental research method that allows you to literally “see” the vessels of the brain. To carry out the study, it is necessary to introduce a contrast agent into the corresponding vessel of the brain and the presence of an X-ray machine, with the help of which an image of the vessels filled with this contrast will be recorded. Angiography of cerebral vessels is not a routine diagnostic method; it has its own indications and contraindications, and, unfortunately, complications. Angiography in a broad sense is the acquisition of images of any blood vessels in the body using X-rays. Angiography of cerebral vessels is just one of the varieties of this extensive research method.
What is cerebral angiography?
The essence of this research method is as follows. The patient is injected into a specific cerebral artery (or the entire network of cerebral arteries) with an X-ray contrast agent, usually iodine-based (Optirey, Omnipaque, Ultravist and others). This is done so that an image of the vessel can be recorded using x-rays, since the vessels are poorly visualized with a regular image. The introduction of a radiopaque substance is possible by puncture of the corresponding artery through a catheter connected to the required vessel from the periphery (usually from the femoral artery). When the contrast agent appears in the vascular bed, a series of X-ray images are taken in two projections. The resulting images are evaluated by a doctor and conclusions are drawn about the presence or absence of a certain pathology of the cerebral vessels.
Indications for use
Angiography of the main arteries of the head is a specialized diagnostic method that should only be prescribed by a doctor. It is not performed at the request of the patient. The main indications are:
• suspicion of arterial aneurysm of cerebral vessels;
• suspicion of arteriovenous malformation;
• determining the degree of stenosis (narrowing) or occlusion (blockage) of cerebral vessels, that is, establishing the lumen of the corresponding vessels. In this case, the severity of atherosclerotic changes in the vessels and the need for subsequent surgical intervention are established;
• establishing the relationship between the cerebral vessels and the adjacent tumor to plan surgical access;
• control of the location of clips applied to the vessels of the brain.
I would like to note that simply complaints of dizziness, headache, tinnitus, and the like are not in themselves an indication for angiography. Patients with such symptoms should be examined by a neurologist, and based on the results of the examination, as well as other research methods, the need for angiography is determined. This necessity is determined by the doctor!
Contraindications
The main contraindications are:
• allergic reaction (intolerance) to iodine preparations and other radiopaque substances;
• pregnancy (due to ionizing radiation during the procedure). In this case, MR angiography may be performed;
• mental illnesses that do not allow one to comply with all the conditions for the procedure (for example, a person will not be able to remain motionless during the image);
• acute infectious and inflammatory diseases (as the risk of complications increases);
• violation of blood coagulation system parameters (both downward and upward);
• the general condition of the patient, regarded as serious (this may be stage III heart failure, end-stage renal and liver failure, coma, and so on). Essentially, this subgroup of contraindications is relative.
Preparation for angiography
To obtain accurate results and reduce the risk of complications from the procedure, it is recommended:
• take general and biochemical blood tests, including determining the indicators of the coagulation system (the period of limitation of tests should not exceed 5 days). The blood type and Rh factor are also determined in case of possible complications;
• do an ECG and FG (FG, if one has not been performed within the last year);
• do not drink alcoholic beverages for 14 days;
• during the last week, do not take medications that affect blood clotting;
• perform an allergy test with a contrast agent. To do this, 0.1 ml of the corresponding drug is administered intravenously to the patient over 1-2 days and the reaction is assessed (the appearance of itching, rash, difficulty breathing, etc.). If a reaction occurs, the procedure is contraindicated!
• the day before, take antihistamines (anti-allergic) drugs and tranquilizers (if necessary and only as prescribed by a doctor!);
• do not eat for 8 hours and do not drink water 4 hours before the test;
• swim and shave (if necessary) the site of puncture or catheterization of the vessel;
• before the examination itself, remove all metal objects (hairpins, jewelry).
Research technique
At the very beginning, the patient signs consent to conduct this type of study. The patient is placed with an intravenous peripheral catheter to have immediate access to the circulatory system. Then premedication is carried out (approximately 20-30 minutes before the procedure): antihistamines, tranquilizers, painkillers are administered to minimize discomfort during the procedure and the risk of complications.
The patient is placed on the table and connected to devices (cardiomonitor, pulse oximeter). After treating the skin with local anesthetic and anesthesia, the corresponding vessel is punctured. A small skin incision is made and a puncture of the femoral artery is made, followed by immersion of the catheter and passing it through the vessels to the study site. Advancement of the catheter along the arterial bed is not accompanied by pain, since the inner wall of the vessels is devoid of pain receptors. The catheter's progress is monitored using x-rays. When the catheter is brought to the mouth of the required vessel, a contrast agent in a volume of 8-10 ml, preheated to body temperature, is injected through it. The administration of contrast may be accompanied by the appearance of a metallic taste in the mouth, a feeling of heat, and a rush of blood to the face. These sensations go away on their own within a few minutes. After the administration of contrast, X-ray images are taken in several projections almost every second several times (which allows you to see the arteries, the capillary phase, and veins). Then the catheter is removed, and a sterile pressure bandage is applied to the puncture site of the vessel. The patient should be monitored by medical personnel for at least 6-10 hours.
Complications
According to statistics, complications during this diagnostic method occur in 0.4-3% of cases, that is, not so often. Their occurrence may be associated both with the procedure itself (for example, bleeding from the puncture site of a vessel) and with the use of a contrast agent. It should be borne in mind that compliance with all conditions when preparing and performing angiography is the prevention of possible complications.
So, possible complications of cerebral angiography are:
• vomit;
• an allergic reaction to an iodine-containing drug: itching, swelling and redness at the injection site, followed by the appearance of shortness of breath (reflex breathing disorder), a drop in blood pressure, and heart rhythm disturbances. In severe cases, anaphylactic shock may develop, which is a life-threatening condition;
• spasm of cerebral vessels and, as a consequence, acute cerebrovascular accident (up to stroke);
• convulsive seizures;
• penetration of the contrast agent into the soft tissue in the area of the puncture of the vessel (outside the vascular bed). If the volume of the drug spilled into the tissue is up to 10 ml, then the consequences are minimal, but if more, then inflammation of the skin and subcutaneous fat develops;
Types of ultrasound of cerebral vessels
Various techniques can be used to study cerebral vessels:
Doppler ultrasound
- used to assess blood flow in vessels, allowing to identify its nature and speed.
Duplex ultrasound.
This technique is a variation of the technique described above. Duplex examination allows you to visualize blood vessels, assess their condition, identify blood clots, plaques, aneurysms and other pathological processes. During this technique, the direction and speed of blood flow are also determined.
Triplex ultrasound.
With its help, an image of the arteries is obtained, colored in different shades, depending on the direction and speed of blood movement. The ophthalmologist can also set other parameters for staining - this opportunity is provided by a computer program. Ultrasound of cerebral vessels using triplex scanning allows you to obtain maximum information about the state of the circulatory system.
Each method has its own advantages and disadvantages. Which diagnostic technology will be chosen is determined by the specialist, depending on what parameters are important to him for diagnosis.
Chronic cerebral ischemia - symptoms and treatment
The diagnosis of chronic cerebral ischemia is often a diagnosis of exclusion (that is, a diagnosis made after excluding all other causes) [6]. Diagnosis is especially difficult in the early stages, when the symptoms of the disease are quite nonspecific and can be disguised as depression and neurotic disorders. Therefore, diagnostics are always comprehensive, including a detailed anamnesis, various laboratory and clinical diagnostic methods, consultation with doctors of other specialties and neuropsychological diagnostics.
A detailed medical history includes a conversation with relatives or the patient’s immediate circle to determine risk factors, the presence of concomitant diseases, and the nature of disease progression.
Examination of neurological status : during an examination of the patient, a neurologist checks muscle strength, sensitivity in different areas of the skin, reflexes (using a neurological hammer), accuracy of movements, stability when standing and walking. Based on the examination, the doctor determines the areas of brain damage (topical diagnosis).
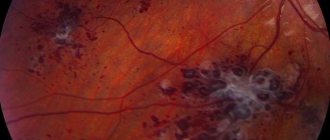
Neuroimaging methods: CT, MRI of the brain, MR angiography (cerebral arteries and veins), if necessary, radiopaque cerebral angiography. Neuroimaging allows you to exclude other diseases (tumor, hydrocephalus) and confirm the vascular nature of the disorders. MRI of the brain is preferable, which reveals changes characteristic of chronic cerebral ischemia:
- leukoaraiosis - a change in the white matter around the ventricles of the brain (in Figure 1, white glow around the ventricles);
- lekoencephalopathy - damage to the white matter of the brain (in Figures 1 and 3, light areas in the subcortical substance);
- small heart attacks, ischemic strokes ( Figure 3);
- multiple microbleeds (Figure 2 - dark areas);
- atrophy of the cerebral cortex.
There is a relationship between the type and severity of morphological changes in the medulla and the stage of the disease [4][6].
A neuropsychological examination allows us to identify the severity and nature of cognitive and emotional disorders, and determine intact functions that can be relied upon in subsequent neurocorrectional work.
The examination is carried out by a neuropsychologist using special tasks: tests of attention, memory, speech, thinking, and motor coordination. Ultrasound of the vessels of the neck and brain allows us to identify signs of hypertensive angiopathy: thickening and uneven internal surface of the vessels, deformation, bends, tortuosity, decreased blood flow speed, as well as signs of atherosclerosis: the number of atherosclerotic plaques, the percentage of vascular stenosis, the degree of danger of the plaque (whether the plaque or its fragment comes off and clogs the vessel).
ECG, Holter monitoring and 24-hour blood pressure monitoring are necessary to determine the severity of cardiovascular disease as the main causative factor of chronic cerebral ischemia [4].
Consultation with doctors of other specialties (general practitioner, endocrinologist, gastroenterologist, nephrologist, nutritionist) is necessary for timely detection and treatment of concomitant diseases.
A general clinical blood test, a study of lipid and carbohydrate metabolism, indicators of kidney function (creatinine, urea) and liver (bilirubin, transaminases) are necessary to identify and correct metabolic disorders.
Possible contraindications
There are no contraindications to ultrasound examination of cerebral vessels. The exception is severe damage to the skin in the area being examined. In this case, the procedure can be postponed until complete healing.
Another nuance may be an allergic reaction to silicone, which is part of the contact gel. If you have already had cases of allergic reactions to silicone, be sure to notify the doctor who ordered the test and the doctor who will conduct it. A specialist may recommend taking antihistamines to reduce allergies, or purchasing another gel without silicone.
Advantages and disadvantages
The main advantage of the diagnostic procedure is its high information content and 100% safety. Since the manipulation does not imply invasiveness, it has no contraindications. The study has other benefits:
- It doesn't hurt at all;
- Ultrasound does not cause discomfort;
- The ability to study both the physical state of blood vessels and their functionality.
One of the disadvantages is the low accessibility of blood vessels in certain areas of the brain for diagnostics using ultrasound.
Preparing for the study
If you want to get the most accurate results, you need to properly prepare for the upcoming test. Let's consider the most important stages of preparation:
- Since we are talking about checking blood vessels, it is important three days before the upcoming procedure to give up alcohol, energy drinks and additives that can affect the functionality of blood vessels and the speed of blood flow;
- Try to completely relax and breathe freely at the time of diagnosis;
- Do not engage in sports or physical activity for at least 2 hours before the ultrasound.
- If you are constantly taking any medications, be sure to discuss this with your doctor. If it turns out that the pills affect blood pressure and blood vessels, the doctor may stop them for a day, or postpone taking the drug to a later time;
- 3 hours before ultrasound diagnostics you need to refrain from smoking;
- Before the procedure, long hair must be collected so that nothing interferes with the examination process.
If the examination is being carried out on a child, you should prepare him mentally. Explain to your child that this procedure is completely painless and does not cause discomfort, persuade him to lie still - movements during the diagnostic process can distort the results of the study.
How to do an ultrasound of the brain
The person lies down on the couch, his head resting on a low pillow. The desired area of the skin is lubricated with silicone gel. In order to determine the nature and speed of blood flow, several sensors are attached to the temples.
If it is necessary to study the condition of the veins and arteries of the brain, the specialist suggests conducting Doppler sonography, during which changes in the displayed sound waves from moving blood cells are recorded. To carry out the procedure, the sensor can be localized in the forehead, back of the head or temples.
In total, the manipulation lasts no more than 40 minutes. Next, the patient receives the test results in hand and goes to the attending physician to decipher the results.
Cerebrovascular disorders
Temporary disorders of cerebral circulation occur for various reasons. Due to osteochondrosis, the openings in the cervical vertebrae narrow, the vessels passing through them are compressed, and the blood supply to the brain becomes difficult - headaches, migraines, etc. appear. With increased blood pressure, severe anxiety or tension, headaches, dizziness, a feeling of heaviness in the head also appear, sometimes vomiting and short-term loss of consciousness.
Author: Olga Gurova, Candidate of Biological Sciences, Senior Researcher, Associate Professor of the Department of Human Anatomy of the RUDN University
Decoding the results
A neurologist interprets the results of an ultrasound examination of cerebral vessels. In order to establish an accurate diagnosis, the specialist takes into account the characteristics of the cerebral vessels and the patient’s medical history, because some changes may be an anatomical feature unrelated to pathology.
If everything is normal, the results should look like this:
- the lumen of the vessels is completely free, various neoplasms are absent;
- turbulent blood flow is not present in the branching of vessels;
- the thickness of the vascular wall is less than 0.9 mm (sometimes 0.9-1.1 mm is also a normal option);
- absence of foreign inclusions, cysts and various neoplasms.
Please note that a diagnosis cannot be made based on ultrasound alone. The disease is determined by a combination of pathological factors, which are indicated by various studies.
What happens when blood pressure rises?
At first, vascular tone is slowly disrupted. Over time, if elevated blood pressure (BP) persists, minor cerebral hemorrhages and strokes may occur.
As a result of a constant increase in blood pressure during hypertension, plasma (part of the blood without formed elements) is released, which ultimately leads to the destruction of the walls of blood vessels.
How does this happen? A specific protein (hyaline-like substance, similar in structure to cartilage) is deposited on the walls of blood vessels, which leads to the development of hyalinosis. The vessels become like glass tubes, lose their elasticity and ability to hold blood pressure. In addition, the permeability of the vascular wall increases, and blood can freely pass through it, soaking the nerve fibers (diapedetic bleeding). The result of such transformations can be the formation of microaneurysms and rupture of the vessel with hemorrhage and blood entering the white medulla. The resulting swelling and hematomas lead to further hemorrhages (hemorrhagic stroke).
Atherosclerosis that accompanies hypertension, or exists without it (which is rare), contributes to cerebral ischemia - insufficient supply of nutrients and oxygen to the tissues (except for atherosclerotic plaques that narrow the lumen of the arteries, the blood itself can be thick and viscous).
Acute circulatory disorders are strokes (hemorrhagic and ischemic). But it all starts with transient cerebrovascular accidents against the background of hypertension and atherosclerosis, as well as obesity, diabetes mellitus, and respiratory diseases that often accompany them.