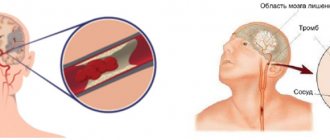
A group of clinical syndromes that develop due to a decrease or cessation of cerebral circulation refers to acute cerebral circulatory disorders or stroke. The cause is: heart disease, atherosclerosis, non-atherosclerotic vascular lesions. If stroke causes persistent neurological disorders, they are classified as a stroke. If the symptoms disappear within 24 hours, the syndrome is classified as TIA - transient ischemic attack. Strokes are classified as ischemic or hemorrhagic. Ischemic stroke occurs when there is a critical decrease in the blood supply to an area of the brain and the development of necrosis of brain tissue. A hemorrhagic stroke is bleeding into the brain tissue or membrane due to rupture of blood vessels in the brain. When large arteries of the brain are damaged, extensive infarctions develop; when small vessels are damaged, lacunar infarctions develop with a small focus of damage to brain tissue.
The Neurology Clinic of the Yusupov Hospital treats patients with strokes and other cerebrovascular diseases. The neurology department treats a wide range of neurological diseases: epilepsy, Alzheimer's disease, Parkinson's disease, various types of dementia, multiple sclerosis and other diseases. The neurological department is equipped with modern equipment and diagnostic equipment, which allows for a quick diagnosis of the disease and timely initiation of treatment.
Causes
As a rule, hemorrhagic stroke develops against the background of stage 2 or 3 hypertension. Often there are also endocrine disorders in the background (pituitary adenoma, pathology of the thyroid gland, pheochromocytoma), which lead to a critical course of arterial hypertension. About a fifth of all strokes are caused by rupture of aneurysms, dissection of the arterial wall, and arteriovenous malformations. Also, the causes of the disease can be systemic diseases of the connective tissue, leading to fragility and increased fragility of blood vessels. Blood diseases such as hemophilia, hematopoietic aplasia, thrombocytopenia, etc. also often serve as a direct cause of the disease. Very rarely, vitamin deficiencies, congenital angiomas, uremia and other conditions lead to hemorrhagic stroke.
In this case, all hemorrhagic strokes are usually divided into strokes due to rupture of a vessel and strokes of the type of diapedetic soaking of the brain substance with blood.
Strokes
This term refers to rupture of an artery followed by hemorrhage. This is a very dangerous condition in which the cerebral cortex is damaged by a growing hematoma with subsequent loss of function. According to ICD 10, there are three codes corresponding to stroke:
- I 60 - indicates hemorrhage into the space that is located between the membranes of the brain, called subarachnoid. According to further gradation, it includes five varieties (0-4) depending on the vessel whose rupture caused the stroke. The next digit is written after the period;
- I 61 – damage to parenchymal tissue. This means that the vessel has ruptured inside the hemispheres or brain stem, damaging the white or gray matter. Further classification also includes five types depending on the location of the lesion;
- I 62 – stroke, the localization of which could not be identified. The doctor is sure that the patient has a hemorrhage, but it is impossible to determine the location and area of the lesion for a number of reasons. Includes three subclasses.
The consequences of stroke of the hemorrhagic type are described in the headings of ICD 10 - these are residual effects after hemorrhage, which often lead to disability. These are very dangerous conditions, during which there is a high mortality rate; about a third of patients die in the first 5 years of life.
Symptoms
Symptoms of hemorrhagic stroke are varied and are divided into two large groups: general cerebral and focal. Also, the symptoms strongly depend on the location of the hemorrhage, its size, the somatic condition of the patient and many other factors.
General cerebral symptoms of hemorrhagic stroke include the following:
- Impaired consciousness (stunning, stupor, coma). The larger the focus, the lower the level of consciousness. However, with damage to the brain stem, even a small focus of hemorrhage leads to severe depression of consciousness.
- Dizziness.
- Nausea, vomiting.
- Headache.
- General weakness.
- Breathing disorders.
- Hemodynamic disorders.
Predominantly focal symptoms include the following:
- Paresis or plegia in the limbs, hemiparesis is more common.
- Paresis of facial muscles.
- Speech disorders develop mainly with damage to the left temporal lobe.
- Visual impairment (including the development of anisocoria).
- Hearing impairment.
A stroke should be suspected if the patient has any type of speech impairment, weakness in the arm and leg on one side, the development of epileptic seizures without provoking factors (for example, such factors include alcohol consumption), impaired consciousness up to coma. In any suspicious cases, it is better to play it safe and call an ambulance. Behavior and assessment of the situation when a stroke is suspected should be considered in a separate article.
Blockages and spasms of blood vessels without heart attack
In clinical practice, there are often cases where disruption of blood flow does not cause necrotic changes. According to ICD 10, such conditions are included in two large groups:
- I 65 – includes damage to the carotid, vertebral and basilar arteries emerging from it;
- I 66 – this code indicates spasm or embolism of the cerebral and cerebellar arteries.
Nerve cells are very sensitive and quickly die due to oxygen starvation and lack of nutrients. But the brain is structured in a unique way; it contains the so-called “Circle of Willis” - these are “spare” connections between arteries, thanks to which blood can flow through bypass vessels. That is why sometimes obstruction does not lead to cerebral infarction.
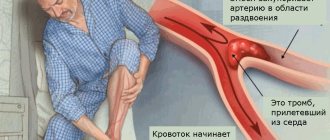
Let us note the main reasons that can create an obstruction in the artery:
- Spasm is a narrowing of a vessel due to contraction of its muscles, resulting in a decrease in its capacity. Usually the cause is neurogenic;
- Narrowing - differs from the previous version by violating the anatomical integrity of the vascular wall in a certain area. Such changes are irreversible;
- Thrombosis is the formation of a blood clot on the artery wall, which gradually increases in size and creates an obstruction;
- Embolus - circulates along with the blood, enters a vessel of a smaller caliber and causes its blockage. Usually this is a detached blood clot or atherosclerotic plaque.
The listed reasons often lead to cerebral infarctions or the development of severe conditions after stroke, having a certain code according to ICD 10.
Diagnostics
Currently, diagnosing hemorrhagic stroke is not very difficult in most cases. If a stroke is suspected, neuroimaging techniques (MSCT or MRI) are indicated, which identify foci of hemorrhage. In the absence of foci of hemorrhage, but the classic clinical picture of a stroke (paresis, speech disorders, etc.), intensive therapy, resuscitation if necessary, and repeated neuroimaging studies after 12-24 hours are indicated.
If it is impossible to conduct MSCT or MRI, the diagnosis is based on complaints, anamnesis (if it is impossible to collect from the patient, they resort to the help of relatives), and data from a neurological examination. In some cases, they resort to lumbar puncture (historically, this method was used everywhere). Blood may be detected in the cerebrospinal fluid, in this case we are talking about a breakthrough of blood into the ventricular system, protein-cell dissociation with a large amount of protein, leukocytes, and single red blood cells.
In the neurological status, they look at the localization of pyramidal signs, the presence of pathological reflexes, assess the level of consciousness, and higher cortical functions. It is also important to evaluate muscle tone, movement disorders, the presence of meningeal symptoms, etc.
Treatment
First of all, when starting therapy for hemorrhagic stroke, it is necessary to establish indications for neurosurgical intervention. With ongoing bleeding, ruptured aneurysms, subarachnoid hemorrhage, cerebral herniation syndrome, progressive hydrocephalus, or large accumulations of blood, patients are advised to undergo urgent surgical intervention. If there are no indications for surgery, then therapy for hemorrhagic stroke includes the following steps:
- Intensive care and resuscitation.
- Active drug treatment.
- Exercise therapy, physiotherapy, speech therapy and general nursing.
- Rehabilitation activities.
Patients with respiratory and hemodynamic disorders are admitted to the intensive care unit, especially if the stroke was accompanied by myocardial infarction, with epileptic seizures, with swallowing disorders (certain swallowing tests are used), with impaired consciousness. In other cases, treatment is used in intensive care wards.
Drug treatment for hemorrhagic stroke is aimed at maintaining respiratory activity (for example, atropine is used to reduce mucus secretion), cardiac activity, and maintaining water-salt metabolism. Basic therapy is also aimed at preventing the development of cerebral edema (diuretics of different pharmacological groups, glycerin are used), combating hyperthermia, preventing pneumonia and renal failure.
Pathogenetic therapy includes the administration of angioprotectors, stopping bleeding, antioxidant, and neuroprotective therapy. Among the angioprotectors with proven effectiveness, ACE inhibitors are used; when prescribing them, contraindications for lowering blood pressure should be taken into account (on the first day, blood pressure should not decrease by more than 15-20 mmHg compared to the initial values). To stop bleeding, aminocaproic acid, dicinone, proteolytic enzyme inhibitors (contrical, gordox) are used, supplement therapy with vitamin K, it is possible to use platelet mass, blood plasma for blood diseases that were the cause of a stroke.
Antioxidant and neuroprotective therapy includes a lot of drugs and is represented by hundreds of trade names. Based on treatment standards, the most commonly used drugs are Ceraxon (according to the instructions), Mexidol, Cytoflavin, Cavinton, Actovegin and other drugs.
If necessary, from the second week, antidepressants can be added to therapy to compensate for vital functions. With the development of symptomatic epilepsy, anticonvulsants are added to therapy. In domestic practice, the drug glycine, which has a multicomponent anti-ischemic effect, is almost always used.
When the condition has stabilized, patients are prescribed first passive and then active physical therapy, which accelerates the disappearance of the motor defect. In the absence of contraindications, physiotherapy is used on the affected limbs.
If there are speech disorders, courses of logotherapy are prescribed. Speech therapists test patients and determine the most optimal type of therapy, depending on the nature of speech disorders.
It is important to pay attention to the overall care of the patient. Prevention of bedsores, breathing exercises to prevent lung complications, and psychological support for loved ones are necessary.
Consequences
As for the consequences of a hemorrhagic stroke, as I usually say, the following rule applies. Those functions lost at the onset of the disease that improved during the first month will generally be restored further. The level of the defect restored during rehabilitation measures in the first year, as a rule, remains practically unchanged.
The consequences of hemorrhagic stroke themselves are varied. Among them, the most common conditions are the following:
- Motor aphasia. A person cannot say a word, although, in general, he has an idea of what is being said.
- Sensory aphasia. A person does not perceive the words that others address to him.
- Dysarthria. This violation concerns the quality of spoken speech.
- Paresis of the limbs. They present as weakness in the muscles of the arms or legs, most often on one side of the body.
- Impaired coordination of movements.
- Pelvic disorders: urinary and fecal incontinence, or, conversely, constipation and urinary retention.
- Memory impairment. As a rule, after a stroke, the level of cognitive functions decreases significantly.
- Depression. Human disability, deep speech and motor, and especially pelvic disorders lead to severe depressive episodes. In many cases, psychiatric consultation and drug treatment for depression are desirable.
Also, to some extent, bedsores should be included as indirect consequences of hemorrhagic stroke. Which can occur during a supine position, congestion of the lungs (with the probable development of pneumonia), general exhaustion of the body, drug-induced damage to internal organs. It should be remembered that the better the general care and concern for the patient, the better the prognosis of the disease.
Forecast
In contrast to ischemic brain damage, the prognosis for hemorrhagic cerebral stroke is much more serious. In approximately 60-80% of cases, the prognosis is unfavorable for life, and the outcome of a vascular accident is the death of the patient. Fatal outcomes are especially common in hemorrhagic stroke localized in the brain stem, blood breakthrough into the ventricular system of the brain. When aggravated by decompensated somatic pathology and extensive hemorrhage, death occurs in almost one hundred percent of cases. The prognosis for work ability is also unfavorable. Although, in general, the prognosis for functional restoration is better than for ischemic stroke. With speech disorders, severe paresis of the limbs due to hemorrhagic stroke, patients become disabled in most cases. Only in small areas of hemorrhage that do not affect important speech and motor areas does the patient return to work after long-term rehabilitation. I would especially like to touch upon the issue of patients in a coma. The prognosis for a hemorrhagic stroke in a comatose patient is very difficult to predict. Coma is not at all an indicator that a person will die. Attention should be paid to the state of hemodynamics, electrolyte metabolism, renal and pulmonary functions. If blood saturation reaches 95-96%, creatinine clearance is normal, and the patient’s blood pressure and heart rate are adequate without hardware support, then the prognosis is generally satisfactory. The prognosis worsens when artificial ventilation is required, air oxygenation with humidified oxygen is required, and the acid-base balance is unstable.
Remaining classification
We have listed the main gradation of cerebrovascular disorders, which are often encountered in clinical practice. Let us note the remaining pathologies, concomitant diseases and conditions after stroke, which correspond to their code according to ICD 10:
- I 64 – set when it is not possible to distinguish hemorrhage from ischemia;
- I 67 – cerebrovascular pathologies not related to strokes and heart attacks;
- I 68 – cerebrovascular accident in other diseases;
- I 69 – complications of stroke.