Treatment of vascular disease of the legs is a set of medical measures aimed at eliminating the unpleasant symptoms of the disease and improving the patient’s quality of life. Among the methods of treatment of vascular diseases of the extremities, a distinction is made between conservative and surgical.
A group of diseases associated with damage to the vessels of the extremities and disruption of their functions are vascular diseases of the legs. Under the influence of certain factors, occlusions (complete blockage) or stenoses (narrowing) occur in a certain area of the peripheral arteries. As a result, the tissues of the limbs experience an acute lack of oxygen, which they no longer receive in the required volume. The patient feels fatigue, pain when walking, chills in the limbs, at first not attaching any importance to this. Then lameness occurs, pain haunts the person even at rest. In the advanced stage, poorly healing wounds and ulcers appear on the skin of the sore leg, and necrosis begins.
How OASNK is developing
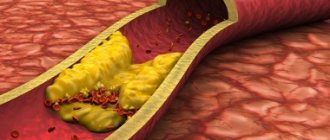
The inner wall of healthy vessels is smooth and even. This allows blood to flow within the lumen of the vessel without any difficulty. With atherosclerosis, the inner wall of the artery becomes uneven and thickened due to cholesterol deposits (cholesterol plaques). This pathological process is called atherosclerosis. With further development of the disease, narrowing or complete blockage of the arteries occurs, which leads to a significant decrease in blood flow to the legs. The consequence of this is the appearance of pain in the calf muscles when walking (intermittent claudication), numbness, and chilliness in the feet. As the disease progresses, pain in the legs becomes constant. Ultimately, trophic ulcers and necrosis appear in the foot area. If no therapeutic measures are taken, the next stage of the disease may be gangrene (death) of the limb.
Reasons for appearance
Varicose veins are based on a characteristic persistent and irreversible change in the walls of blood vessels belonging to the superficial venous peripheral network. This is facilitated by venous hypertension (4, English). This increase in pressure is triggered and maintained by many predisposing factors.
At first, venous hypertension is reversible and does not lead to structural changes in blood vessels, but already at this stage pathological processes are launched, which over time or with the addition of other provoking factors lead to deformation of the veins - such irreversible changes are called varicose veins.
Even before the characteristic visible deformation of the veins, pathological processes develop with an increasing effect; consider the sequence (5, English):
- Venous hypertension is accompanied by difficulty in the outflow of blood and a slowdown in its flow. Red blood cells are grouped in the center of the lumen of the vessel, and leukocytes and platelets are pushed to its periphery.
- Redistribution of leukocytes along the inner lining of the veins. The production of endothelial factors is stimulated, which promotes the adhesion (sticking) of leukocytes and their activation. The process of thrombus formation begins, which aggravates the damage to the surface of the venous walls.
- Phlebosclerotic process in the area of venous valves. Normally, when filled with blood, the valves close tightly to each other and block the lumen of the vein. This is necessary to prevent reverse blood flow during cardiac systole. Sclerosis leads to deformation of the valves, and they are no longer able to fully perform their function.
At the earliest stages, all these changes do not yet lead to clinically significant hemodynamic disturbances. And patient complaints are so far limited to cosmetic defects. Over time, visible deformation of the affected area of the vessel begins. The vein acquires pathological bends and lengthens somewhat, local expansions and saccular bulges in the form of varicose nodes appear on it. This is accompanied by worsening valve insufficiency - the valves located in the area of varicose deformation cease to touch each other when filled.
The pathological reverse flow of blood that occurs at this stage is called vertical reflux. This hemodynamic disturbance is one of the key pathogenetic aspects of varicose veins, as it contributes to the formation of chronic venous insufficiency with blood stagnation. It is this that leads to the appearance of the main symptoms of varicose veins. But when small and very small venous vessels in the thickness of the dermis are affected, clinically significant stagnation of blood does not occur.
Risk factors for OASNK
Atherosclerosis of the vessels of the lower extremities is characterized by the same risk factors as other arterial diseases, for example: coronary heart disease and cerebrovascular insufficiency.
- High blood pressure (hypertension),
- High blood cholesterol levels,
- Smoking,
- Sedentary lifestyle,
- Obesity,
- Burdened heredity.
A few words about smoking. Complete abstinence from any form of tobacco is necessary. Smoking even 1 cigarette per day of the lightest type is an unfavorable risk factor that causes the progression of obliterating atherosclerosis of the lower extremities and the development of its severe complications. The nicotine contained in tobacco causes the arteries to spasm, thereby preventing blood from moving through the vessels and increasing the risk of blood clots in them.
Prevention
The best way to prevent intermittent claudication and other symptoms of vascular disease in the legs is to maintain a healthy lifestyle. It means:
- Quit smoking if you smoke!
- If you have diabetes, monitor your blood glucose levels.
- Regular exercise for 30 minutes, at least 3 times a week, after consultation with your doctor.
- Reduce cholesterol and blood pressure.
- Eat foods low in saturated fat.
- Maintain a normal weight.
Symptoms of OASNK
- Pain in the leg at rest, depriving the patient of sleep;
- Pain or a feeling of fatigue in the leg muscles when walking (usually in the calf muscles) - this symptom is one of the early signs of atherosclerosis of the leg vessels;
- Unusual feeling of chilliness and numbness in the foot, aggravated by physical activity (walking, climbing stairs;
- The presence of a non-healing wound or trophic ulcer, usually located in the foot or lower third of the leg;
- Darkening of the skin, often in the form of dark brown or black necrosis of the toes (gangrene);
- Difference in skin temperature between extremities (the affected leg is cooler than the healthy leg).
Stages of development of atherosclerosis of the lower extremities
The manifestation of one or another symptom depends on the stage of atherosclerosis of the arteries of the lower extremities. In this connection, the following stages are distinguished (in our country, classification according to A.V. Pokrovsky, 1976):
- Stage I – pain in the lower extremities manifests itself during heavy physical activity, walking over a distance of more than 1 km.
- Stage II A – pain in the limb occurs when walking at a normal pace for more than 200 m.
- Stage II B - pain in the limb occurs when walking at a normal pace of less than 100-200 m,
- Stage III – pain in the limb occurs at rest or when walking less than 25 m.
- Stage IV – the pain is constant, there are ulcerative-necrotic changes in the tissue.
Most often, the level of damage is accompanied by complaints of characteristic localization.
With atherosclerosis of the aorta and iliac arteries, the so-called Leriche syndrome, in which pain is localized in the gluteal muscles, thigh muscles, there is no pulsation in the femoral arteries, or it is sharply weakened. Men also experience impotence.
With obliterating atherosclerosis of the femoral and popliteal arteries, pain is localized in the muscles of the legs and feet.
The influence of pregnancy on the formation of varicose veins
During pregnancy, it is important to stop the progression of varicose veins for the health of the mother and the unborn child.
Consultation with a phlebologist is required. Pregnancy creates the prerequisites for the appearance of initial varicose veins and its further development (6, 7 English):
- Hormonal imbalance between estrogens and gestagens. Already from the first days, the level of progesterone in the blood progressively increases, which prevents the onset of the next menstruation. But this hormone affects not only the condition of the endometrium and the entire uterus. Under the influence of progesterone, the tone of the smooth muscle layer in the walls of internal organs and blood vessels, including the veins of the lower extremities, decreases - this contributes to the deterioration of blood evacuation from the peripheral parts of the extremities with the development of venous hypertension.
- The growing uterus causes compression of nearby organs and vessels of the small pelvis. Already from the second trimester of gestation, most women experience difficulty in the outflow of blood through the inferior vena cava system. The resulting increase in pressure in the veins of the legs contributes to the decompensation of existing venous pathology and active remodeling of the vascular walls. There is often concomitant lymphostasis, which aggravates the situation.
- Physical inactivity at the end of the second and third trimesters of pregnancy. With insufficient physical activity, the efficiency of the muscle pump of the legs decreases, and there is a risk of early, initial varicose veins.
During pregnancy, symptoms of both cosmetic and classic varicose veins can develop. Women often do not attach much importance to them, considering them a natural manifestation of pregnancy. Therefore, a consultation with a phlebologist is included in the list of mandatory examinations.
Diagnostic methods for OASNK
If atherosclerosis of the arteries of the lower extremities is suspected, further examination is necessary to confirm (or exclude) the diagnosis of OASNK, establish the stage of the disease and determine treatment tactics. For this purpose, the following series of diagnostic measures are carried out:
- Examination by a vascular surgeon to determine the pulsation of the main arteries of the extremities, neck and abdominal cavity, as well as listening to noises in the projection of large vessels;
- Ultrasound duplex scanning
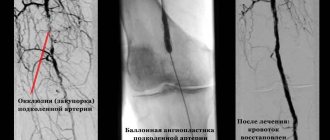
- X-ray contrast angiography;
- Computed tomography in angio mode;
- Magnetic resonance imaging in angio mode.
Through the above studies, local damage or multifocal (multi-level, multi-story) atherosclerosis of the main arteries, atherosclerosis of the aorta and arteries of the lower extremities is revealed. Areas of complete closure of the lumen (occlusion) of the artery and thrombosis may be detected.
Deep vein thrombosis (DVT) - what is it?
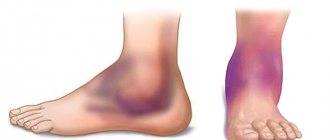
Deep vein thrombosis is a disease in which blood clots (thrombi) form in the lumen of the deep veins. The lower extremities are most often affected.
The mechanism of development of deep vein thrombosis
As the disease progresses, the health of the deep vessels is at risk. If treatment is not prescribed in time, there can be serious consequences.
Treatment of atherosclerosis of the vessels of the lower extremities
A vascular surgeon treats atherosclerosis of the aorta and arteries of the lower extremities.
Treatment of obliterating atherosclerosis of the vessels of the lower extremities depends on the stage of the disease and its prevalence. In the initial stages, it may be sufficient to eliminate risk factors for the disease:
- Weight correction for overweight or obese patients;
- Monitoring and correction of blood sugar levels in patients with diabetes mellitus;
- Control of blood pressure and maintain it at the recommended level (no more than 140/90 mmHg);
- Quitting bad habits (primarily smoking);
- Regular physical activity (training walking, exercise on an exercise bike, visiting the pool, etc.). Therapeutic walking for atherosclerosis of the lower extremities is of great importance for the development of collaterals. A gradual daily increase in physical activity is necessary;
- Following a diet low in cholesterol and animal fats;
- Reducing blood cholesterol levels to doctor-recommended levels.
Drug treatment of obliterating atherosclerosis of the arteries of the lower extremities
Most often, to prevent the sticking of platelets (blood cells involved in the formation of a blood clot), the doctor prescribes drugs containing aspirin or drugs containing clopidogrel.
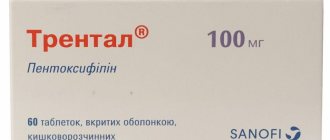
Medicines that improve collateral (roundabout) blood circulation - pentoxifylline containing drugs.
Statins are also used - these are drugs aimed at lowering blood cholesterol levels, thereby slowing down the growth of atherosclerotic plaque.
Medicines that improve peripheral circulation by dilating blood vessels - drugs based on prostanoids.
Surgical treatment of obliterating atherosclerosis
Surgical treatment for atherosclerosis of the arteries of the lower extremities is used in cases where conservative treatment is ineffective, there are signs of disease progression, as well as in advanced stages of the disease:
- Balloon angioplasty;
- Prosthetics;
- Stenting;
- Bypass;
- Endarterectomy.
- Lumbar sympathectomy is an operation to destroy sympathetic nerve fibers and remove the lumbar sympathetic ganglia, which are capable of contracting the muscular wall of the arteries. The operation is performed to increase blood flow to the tissues and reduce pain. This operation is also performed to reduce excessive sweating of the feet.
Gentle foot care
In addition to the recommendations listed, take care of your feet. In people with vascular disease of the legs, especially in combination with diabetes, wounds on the legs and feet do not heal well. Weakened blood circulation leads to slower treatment and an increased risk of infectious complications.
Follow these tips:
- Wash your feet daily, dry them thoroughly and moisturize them to prevent cracks, as they lead to infection. Avoid moisturizing between your toes as this encourages the development of fungus.
- Wear comfortable shoes and thick, dry socks.
- Treat any fungal infection on your feet thoroughly
- Be careful when cutting your toenails
- Avoid walking barefoot
- If you experience pain or sore skin, consult a doctor
Deep vein thrombosis - treatment at home
Today, along with traditional methods of treating the disease, traditional medicine is practiced if deep vein thrombosis is determined. Treatment with folk remedies is used as a complement to the main treatment.
The first thing to do is thin the blood. If you have deep vein thrombosis, treatment with traditional methods includes consuming the following products:
- onion and garlic;
- sunflower seeds;
- cocoa;
- beets;
- Apple vinegar;
- tomatoes or tomato juice;
- Hercules;
- oatmeal;
- cranberries;
- oatmeal;
- lemon;
- cherries;
- viburnum.
Blood thinning should be approached with caution so as not to provoke bleeding. It is not recommended to consume fatty and meat products if you have deep vein thrombosis. Photos and results of improper treatment are available on the Internet.
Every day you can eat one spoon of a mixture made from crushed garlic, two tablespoons of unrefined vegetable oil and one tablespoon of honey.