Home / Cardiologist / Treatment of vascular insufficiency
Vascular insufficiency is a phenomenon that is associated with the pathology of the circulatory system due to deterioration in the tone and elasticity of blood vessels, as well as problems with the passage of blood through them and directly with the amount of blood itself. As a result of a decrease in blood flow speed, the transport of oxygen and nutrients across cell membranes is disrupted. Hypoxia develops and the functioning of cells and tissues is disrupted.
Pure vascular insufficiency is rare; most often, heart muscle insufficiency occurs simultaneously with symptoms of vascular insufficiency.
Types of vascular insufficiency
Based on localization, vascular insufficiency can be divided into: regional (affecting a specific part of the body) and systemic (affecting the vessels of the whole body).
According to the speed of formation and progression, acute and chronic vascular insufficiency are distinguished.
- Acute failure develops when there is a sharp drop in the level of pressure in the vessels, for example, with cardiogenic shock due to myocardial infarction. Characterized by the development of collapse due to a pronounced drop in blood pressure.
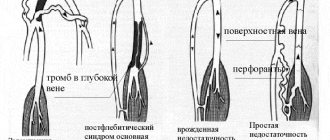
- Chronic failure develops over time when blood pressure drops below 100/60 mmHg. This concept includes a wide group of diseases: thrombophlebitis, vertebrobasilar insufficiency, coronary heart disease, mesenteric vascular insufficiency and other conditions accompanied by ischemia. Chronic vascular insufficiency can be primary (develops when the activity of the autonomic nervous system is disrupted) and secondary (due to various diseases).
Who is susceptible to arterial pathologies?
The risk group for arterial dysfunction includes persons of both sexes with:
- Hereditary predisposition (family history of arterial diseases);
- Disorders of metabolic processes in the body;
- Hypertension;
- Decompensated diabetes mellitus;
- Heart rhythm disorders;
- Tendency to stress and chronic fatigue syndrome;
- Increased levels of cholesterol and lipids in the blood;
- Obesity and pre-obesity;
- Addiction to fast food and other foods with a high concentration of saturated fats;
- Physical inactivity;
- Autoimmune disorders;
- Bad habits (smoking, alcohol abuse);
- Injuries associated with vascular deformation;
- Extensive intense frostbite of the extremities;
- Chronic infectious diseases that provoke thinning of the walls of blood vessels (syphilis, tuberculosis, etc.).
Elderly people are more susceptible to vascular pathologies, but in recent years there has been a tendency to increase the number of young patients with this problem.
Causes of vascular insufficiency
The acute variety occurs in various cardiac pathologies, massive blood loss, poisoning, severe infections, adrenal insufficiency, organic damage to the nervous system, extensive burns, traumatic brain and general injuries.
The root causes of the chronic form are autonomic and neurological factors, organic lesions of the brain stem and heart, in which there is hypotension with constant low blood pressure and, as a consequence, constant systemic hypoxia of organs and systems, the impossibility of adequate tissue perfusion with increasing consumption due to stress.
Symptoms of vascular insufficiency
Manifestations of vascular insufficiency depend on the type of insufficiency.
Acute vascular insufficiency
- Collapse – develops with a sharp decrease in blood pressure. It develops suddenly, when within a few seconds a person begins to feel severe weakness, noise in the head, dizziness, and the appearance of a “veil” before the eyes. The man loses consciousness. The patient's skin is pale, cold, breathing is rapid and shallow.
- Fainting – develops with a sudden disruption of cerebral circulation. The patient loses consciousness for several seconds or minutes, followed by darkening of the eyes, ringing in the ears, and severe weakness.
Chronic vascular insufficiency
Has signs of ischemia of organs and tissues, which has not clearly expressed signs:
- Cold extremities
- Blue discoloration of soft tissues in the periphery (fingertips, nose, earlobes)
- Trophic disorders (loss and fragility of hair, nails, loss of turgor and elasticity of the skin)
- Reduced pain and temperature sensitivity
- Weakness in the limbs, especially after exercise
- Muscle wasting
- Fast fatiguability
- Chronic cerebrovascular insufficiency is manifested by frequent headaches, dizziness, clouding of consciousness, decreased memory, attention, and ability to concentrate
- Chronic mesenteric ischemia is manifested by symptoms of dyspepsia (nausea, vomiting), abdominal and epigastric pain
Appointment with a surgeon (vascular surgeon) for patients with atherosclerosis of the arteries
Chronic arterial insufficiency of the lower extremities
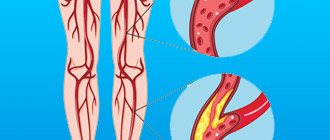
Chronic arterial insufficiency (CAI) of the lower extremities is a pathological condition accompanied by a decrease in blood flow to the muscles and other tissues of the lower extremity and the development of its ischemia with an increase in the work performed by it. Blood circulation in the lower extremities is weakened, which is why the most distant parts of the legs usually suffer. The tissues in these places do not receive the necessary amount of nutrients and oxygen, which are delivered by the arterial blood flow. This can lead to serious consequences, so you need to know what causes this disease, how to recognize it and cure it.
The clinical picture of CAN can be caused by both isolated and combined occlusions (closure of the lumen) of the abdominal aorta, its bifurcation, iliac and femoral arteries, as well as arteries of the leg and feet.
The pathogenesis of arterial diseases is multifaceted, and the list of their types and the nature of clinical manifestations is very wide. It is advisable to briefly list the main groups of diseases caused by damage to the arterial bed. The most important in terms of prevalence are atherosclerosis and vascular complications of diabetes mellitus, causing limb ischemia.
Together with a vascular surgeon, consultations are held for patients with pathology of the arteries of the lower extremities, brachiocephalic arteries, varicose veins of the lower extremities, after examination and evaluation of the examination results, the patient is prescribed conservative therapy, recommendations for care, additional examination methods, if indicated, a referral for outpatient examination is given and hospitalization in the department of surgery, vascular surgery or purulent surgery.
Causes of insufficient blood flow in arterial insufficiency of the lower extremities
Atherosclerosis of the lower extremities. This is a condition when atherosclerotic deposits that form on the walls of blood vessels block the lumen of the arteries.
Diabetic vascular damage.
Thrombosis. In this case, the blockage of the artery occurs due to a blood clot that has formed there. Also, a blood clot could move into a vessel of the lower limb from another place, this is called an embolism.
Endarteritis. In this case, the walls of the artery become inflamed, which leads to spasm of the vessel.
Symptoms of arterial insufficiency of the lower extremities
Symptoms of chronic ischemia of the lower extremities
- Subjective symptoms: at first there are no symptoms, over time - rapid fatigue of the limbs, increased sensitivity to cold, paresthesia. Most often, patients consult a doctor about intermittent claudication; there is pain that occurs quite regularly after a certain muscle load (walking a certain distance). Pain (sometimes described by patients as a numb, stiffening sensation) in the muscles below the site of arterial stenosis/occlusion, radiates, causes the patient to stop, and spontaneously disappears after a few tens of seconds or a few minutes of rest. Most often, the pain is localized in the lower leg muscles. Foot lameness (deep pain in the midfoot [short foot muscles]) occurs rarely, but is more common in thromboangiitis obliterans (Buerger's disease) and in diabetes mellitus. Patients with obstruction of the aorta or iliac arteries may develop Leriche syndrome - intermittent claudication, absence of pulse in the inguinal folds, erectile dysfunction.
- Objective symptoms: the skin of the feet is pale or cyanotic (especially in an upright position), cold, in the later stages - with trophic changes (depigmentation, hair loss, ulcers and necrosis); muscle atrophy, weak, absent or asymmetrical pulse in the arteries below the stenosis/occlusion, sometimes a vascular murmur above the large arteries of the extremities. In the lower extremities, the pulse is assessed in the arteries: dorsal artery of the foot (on the back of the foot between the I and II metatarsal bones, in 8% of healthy people it is not determined), posterior tibial (along the medial malleolus), popliteal (in the popliteal fossa), femoral (in the groin , just below the inguinal ligament).
Stages of diseases of arterial insufficiency of the lower extremities
Asymptomatic course
Intermittent claudication (by name of the dominant clinical manifestation)
Critical limb ischemia.
- The asymptomatic course of diseases of the arteries of the lower extremities is a preclinical stage of chronic arterial damage that does not cause clear clinical manifestations of chronic arterial insufficiency. This stage is characterized by damage (most often atherosclerotic) of arteries without hemodynamically significant stenoses or with minor changes in regional hemodynamics that do not cause clear clinical manifestations of chronic ischemia limbs.
- Intermittent claudication is a syndrome of transient chronic ischemia of the limb, which manifests itself as malaise, discomfort or pain in the muscles of the lower limb (usually in the calf, less often in the gluteal region, thigh, foot), which occurs during physical activity. At this stage, morphological changes in the arteries are significant and are sufficient to cause distinct hemodynamic changes, the essence of which boils down to the suppression of the parameters of volumetric blood flow velocity and perfusion pressure in the arteries distal to the focus of the obliterating lesion. Both from the point of view of pathogenesis and in the light of the clinical course, HP characterizes the stage of subcompensation of LEAD - the main symptoms appear during physical activity.
- Critical limb ischemia is a syndrome of decompensation of chronic arterial insufficiency of the limb due to diseases of the arteries of the lower extremities, the main clinical signs of which are pain at rest, not relieved by narcotic analgesics and (or) the presence of an ulcerative-necrotic process of the foot. The basis of the pathogenesis of critical limb ischemia is progressive damage to the arterial bed such a degree of severity at which compensatory mechanisms (hemodynamic and metabolic) are unable to prevent insufficient blood supply to tissues.
Classification according to FONTAIN (1954)
Stage I full compensation.
It manifests itself only with significant physical exertion by the occurrence of parasthesia, fatigue, chilliness of the feet, sensations of coldness, and sometimes increased sweating.
Stage II circulatory failure during functional load.
To the clinical manifestations of stage I ischemia is added intermittent claudication - the occurrence of pain in the calf muscles, forcing the patient to limit the pace of walking or stop for rest.
Stage III – circulatory failure at rest.
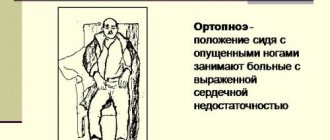
Manifests itself as constant and/or/ night pain. The patient is forced to lower his leg down from the bed.
Stage IV – ulcerative-necrotic changes in the limb.
Diagnosis of arterial insufficiency of the lower extremities
Diagnostics is based on several groups of methods. For example, a physical examination includes different modalities. For example, this is thermometry, that is, a decrease in skin temperature. The movements occurring in the joints are also assessed. Determining sensitivity is considered important. The physical examination also includes a study of peripheral pulsations and a study of the “capillary” pulse.
Among the instrumental diagnostic methods, the following should be noted:
- Arterial blood pressure - after measuring blood pressure in the arms and legs using an ultrasound Doppler (a device for determining blood flow), the obtained figures are compared and a general conclusion is made about the presence of arterial blood flow disorders in the lower extremities
- Duplex (triplex) scanning of arteries - ultrasound vascular examination allows you to detect narrowing or blockage of the artery and measure the diameter of the vessel. Provides information about the condition of the saphenous vein of the leg, in order to decide on the use of the saphenous vein as a bypass (shunt) to bypass the blocked section of the artery.
- Computed angiography CT angiography is a study performed on a spiral computed tomograph with the simultaneous injection of contrast into the saphenous vein of the arm, providing information about the presence and extent of narrowing, blockage, and dilatation of the arteries. Invasive examination - the examination is carried out by injecting contrast into the arteries under X-ray control.
- Angiography. An angiogram is the most valuable study in patients with atherosclerosis of the arteries of the lower extremities, for whom, according to preliminary examination and examination, surgical treatment is indicated and planned. Contrast is injected into the artery and a special x-ray is used to show the exact location of the blockage or narrowing of the artery and the condition of the arteries above and below the affected area. Angiography is necessary when there is a question about endovascular intervention or surgical treatment of atherosclerosis of the arteries of the lower extremities.
The prognosis for the natural course of occlusive processes in the arteries of the lower extremities is unfavorable. According to N. Heine (1972), several years after the first signs of ischemia of the lower extremities appear, 2-3 patients either die or are subject to surgical treatment—limb amputation. In patients with critical limb ischemia, a year after diagnosis of the disease, 25% die from cardiovascular complications, another quarter of patients undergo high limb amputations. Approximately 50% have second limb involvement.
Treatment depends on the degree of ischemia and how extensive the areas of arterial damage are. The first thing the patient needs to do is give up bad habits, such as smoking. Smoking greatly aggravates this disease, contributing to its rapid development. In addition, if ischemia has just begun to develop, regular physical exercise may be helpful to improve blood supply to the limb. Such exercises are selected by a doctor.
For some patients, lifestyle changes are sufficient to stop the progression of atherosclerosis, but some patients require drug therapy or surgical treatment.
Factors that increase the risk of limb loss in patients with critical limb ischemia
- Factors leading to weakening of blood flow in the microvasculature:
- diabetes
- severe kidney damage
- marked decrease in cardiac output (severe chronic heart failure, shock)
- vasospastic conditions (Raynaud's disease, prolonged exposure to cold, etc.)l
- Tobacco smoking
- Factors that increase the need for blood flow in tissues at the level of the microvasculature
- infection (cellulitis, osteomyelitis, etc.)
- skin damage, trauma.
Conservative treatment of arterial atherosclerosis
Conservative treatment of chronic arterial ischemia of the extremities includes drug treatment and physiotherapeutic treatment. However, according to most authors, conservative treatment is ineffective and very often surgical treatment has to be used.
Surgical treatment of arterial atherosclerosis
Surgical treatment for atherosclerosis of the arteries of the lower extremities is used in cases where conservative treatment is not effective and (or) there are signs of disease progression that limit the patient’s lifestyle. There are several options here.
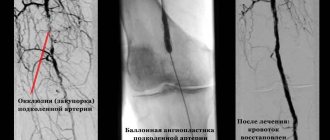
- Balloon angioplasty, stenting . These methods help expand the lumen of the vessel .
- Endarterectomy. This is the removal of atherosclerotic deposits from the lumen of the artery.
- Bypass surgery, prosthetics . They restore blood flow to the arteries located below the blocked area. Bypass options:
- Aortofemoral or aortobifemoral allografting
- Femoropopliteal allo- or autovenous bypass
- Femoral-tibial autovenous shunting.
- Limb amputation
Indications for surgery have now been significantly expanded. The absolute indications are pain at rest and the ulcerative-necrotic stage of ischemia of the lower extremities.
ONLY THE DISEASE CAN OVERCOME
SURGERY TO RESTORE VASCULAR FUNCTIONS!
Restoring blood flow (revascularization) is considered the only way to save a limb from high amputation when the supply arteries are damaged by atherosclerosis or diabetes. Currently, there are two complementary methods of revascularization - open bypass surgery and closed intervention through a puncture of the skin - balloon angioplasty of the arteries of the lower extremities.
Mortality after operations on the great vessels reaches 13%. The frequency of amputations for obliterating diseases of the arteries of the extremities is 47.6%, after reconstructive operations – from 10% to 30% according to various authors. Early obstruction of an artificial vessel occurs quite often - in 18.4% of cases, and all kinds of complications after operations can reach 69%. Shunts on the lower limb after 5 years function at 3 degrees. ischemia in 17% of cases, with 4 tbsp. ischemia - 0%. The largest number of late complications (60.2%) of reconstructive operations on the lower extremities requiring repeated operations occur in the first 3 years.
If treatment is not started in time, gangrene may begin. This brings a lot of suffering to a person. To avoid such a turn of events, it is best to prevent the development of the disease, which will help with a correct, healthy lifestyle. It is better to give up bad habits now than to painfully pay for their consequences later.
Remember that the further the disease has progressed, the more difficult it is to achieve a complete recovery!
Diagnosis of vascular insufficiency
To the extent that the symptoms of vascular insufficiency are not always pronounced, to clarify the diagnosis of the pathology and then select the optimal treatment regimen, the patient will need to undergo several types of examinations. Among them:
- Orthostatic test. Control of pressure in a state of activity, passivity, when changing body position.
- Plethysmography. Necessary for determining vascular tone.
- ECG diagnostics. It is carried out to identify pathologies of the heart muscle in hemodynamics.
- Ultrasound diagnostics of the heart. Allows you to determine the need for treatment of existing heart diseases.
A comprehensive diagnosis will reveal the cause-and-effect relationship between symptoms and characteristics of the disease, which in turn will allow the doctor to choose the right treatment regimen and effective prevention methods in the future.
Treatment of vascular insufficiency
The key treatment for vascular insufficiency over the past few years has been the administration of angiotensin converting enzyme inhibitors. This group of drugs dilates arteries, reduces peripheral vascular resistance, helps restore the function of their inner lining, and facilitates the work of the heart. If symptoms of vascular insufficiency develop against the background of the diagnosis of another pathology, the main treatment should be aimed at eliminating the root cause.
The best prevention of vascular insufficiency is the prevention of diseases that can cause it. It is recommended to monitor the condition of blood vessels, consume less cholesterol, and undergo regular examinations of the circulatory system and heart. In some cases, hypotensive patients are prescribed a prophylactic course of blood pressure-maintaining medications.
In our Medical City Alexandrov, the appointment is conducted by an experienced cardiologist, a high-class specialist who will conduct a comprehensive diagnosis of the disease and prescribe the necessary treatment.
By contacting us, you can be sure of a quality result!
To make an appointment with a specialist and find out all the details, please call: 8 (49244) 9-32-49
Prevention
For patients prone to arterial diseases, it is important to monitor their health and adhere to the following preventive measures:
- Control of blood sugar and cholesterol;
- Compensation for diabetes mellitus (if any);
- Timely treatment of related diseases of a provoking nature;
- Normalization and stabilization of optimal body weight;
- Quitting smoking and drinking alcohol;
- Optimization of sleep and wakefulness, improvement of motor activity;
- Rationalization of nutrition and adherence to an anti-sclerotic diet (especially for older people);
- Minimizing stress effects on the body;
- Regular scheduled examinations by specialized specialists.
With minimal suspicion of arterial disease, it is important to immediately consult a doctor for differential diagnosis and adequate therapy.