Cardiosclerosis is a pathological replacement of the working muscle tissue of the heart with rigid connective tissue that does not bear a functional load. An inelastic replacement is unable to contract and conduct impulses.
In cardiology, the disease is regarded as one of the manifestations of myocardial damage caused by a deficiency or cessation of blood supply, otherwise known as coronary heart disease (CHD). Cardiosclerosis is classified into four types:
- myocardial cardiosclerosis – a complication of inflammation of the muscular lining of the heart (myocarditis);
- post-infarction cardiosclerosis – consequences of necrosis (death) of a portion of the myocardium;
- primary cardiosclerosis is the result of congenital pathologies of the inner layer of the membrane of the myocardial walls and connective tissue;
- atherosclerotic cardiosclerosis.
According to ICD-10, the disease was assigned code I25.1.
About the disease
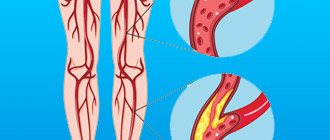
The cause of this disease is atherosclerosis - a chronic process in the vascular wall of medium- and large-caliber arterioles, which is based on the accumulation of cholesterol, the growth of scar tissue and the narrowing of the lumen of the vessel.
In the international classification of diseases (ICD 10), cardiosclerosis is coded in the group of coronary heart disease (CHD):
- I25 - chronic ischemic heart disease:
- 0 - atherosclerotic cardiovascular disease.
At the appointment, I diagnose this condition in patients with a long course of coronary heart disease and its consequences (angina pectoris, myocardial infarction, rhythm disturbances, circulatory failure).
Symptoms
Atherosclerotic cardiosclerosis progresses slowly. Primary symptoms are not specific. Changes in the myocardium are manifested by slight shortness of breath, chronic drowsiness and fatigue, accelerated fatigue, tingling in the subclavian region (left).
Patients note increased heart rate, pale skin, and short-term numbness in the fingers of the left hand. As the sclerotic areas increase, sharp chest pain occurs (angina pectoris syndrome). Periodically, the heart “stabs”, and pain is felt not only in the heart area, but also on the left side of the body (under the shoulder blade, under the collarbone, in the arm).
No ads 3
Developing:
- dyspnea (shortness of breath);
- heart rate disturbance (tachycardia, bradycardia);
- painful sensations in the epigastric region, accompanied by nausea;
- dry chest cough;
- insomnia (insomnia).
At a later stage, the symptoms of coronary heart disease are added to the listed signs. Swelling of the face and lower limbs. Dizziness, periodic clouding of consciousness, fear of death, manic anxiety, and fainting occur. Angina attacks last up to 15 minutes.
One of the signs of hypercholesterolemia is fatty growths under the skin of the eyelids - xanthomas.
Causes
Today it has been established that atherosclerotic cardiosclerosis is a disease caused by a combination of many factors. Some of them can be influenced by one or another therapeutic measures. A favorable basis for cholesterol deposition is the presence of damage to the internal lining of the vessel (intima).
Risks of developing atherosclerotic cardiosclerosis:
- Unmodifiable (unchangeable):
- genetic predisposition (hereditary dyslipidemia);
- age (men over 40, women over 50);
- male (estrogens produced during the menstrual cycle protect blood vessels from becoming saturated with cholesterol).
- Modifiable (changeable):
- dyslipidemia caused by poor nutrition;
- arterial hypertension;
- smoking, alcohol;
- overweight, metabolic syndrome;
- carbohydrate metabolism disorders (hyperglycemia, diabetes mellitus);
- tachycardia;
- sedentary lifestyle;
- chronic stress;
- hyperhomocysteinemia (an excess of this amino acid causes damage to the intima of the vessel, to which it is easier for cholesterol to attach).
The basis for the development of atherosclerotic cardiosclerosis is:
- Combined disorder of protein and fat metabolism. Previously, the main role was given to hyperdipidemia - an increased concentration of fats in the patient's serum due to their excess consumption. To date, it has been proven that an imbalance between “good” (high density - HDL) and “bad” (low and very low density - LDL, VLDL) lipoproteins plays a significant role in the deposition of cholesterol plaques.
- Hormonal imbalance. Insulin resistance, diabetes mellitus, and hypothyroidism contribute to the accumulation of cholesterol in the inner layer of cells (endothelium) of arterioles.
- Hemodynamic load. Constant high blood resistance in hypertension contributes to the rapid development of pathological processes in the vascular bed.
- Nervous factor. Constant stress, conflicts, lack of sleep, and unfavorable psycho-emotional background lead to impaired control over the metabolism of proteins and lipids and disorders of vascular tone.
- The immediate condition of the walls of blood vessels. An atherosclerotic plaque does not form on the intact intima of the coronary arteries. Therefore, the presence of age-related changes, an infectious process, and thrombosis facilitates the formation of cholesterol deposits.
The main danger of this disease is that cholesterol plaques, as they increase in size, lose their stability, ulcers form on their surface, and thrombotic masses accumulate. Ultimately, the affected vessel is completely blocked, and myocardial ischemia develops. Only after this do symptoms appear, with which the patient consults a doctor.
If the affected vessels are small in caliber, over time the blood-supplied areas of the heart muscle grow with connective tissue fibers that replace cardiomyocytes, gradually reducing the contractility of the myocardium. In case of blockage of a larger coronary vessel, a clinical picture of acute coronary syndrome develops with necrosis of heart tissue and replacement of the non-functioning area with a fibrous scar.
Causes of hypercholesterolemia and atherosclerosis
Atherosclerosis develops under the influence of correlation factors: hypercholesterolemia and the presence of microdamage to the endothelium. The normal level of total cholesterol in the blood for adults is 3.2-5.2 mmol/l. Analysis results > 7.7 mmol/l are considered pathologically overestimated.
An increase in LDL and VLDL in the blood is caused by:
- unhealthy eating habits (excessive fatty and sweet foods in the diet);
- low physical activity (hypodynamia);
- long-term psycho-emotional instability (stressful state);
- chronic diseases of the gallbladder and liver;
- malabsorption is a violation of the resorption (absorption) of nutrients in the intestine.
Hypercholesterolemia accompanies diabetes mellitus and other metabolic disorders. Microcracks in the endothelium appear as a result of the aggressive influence of nicotine, alcohol, and certain medications. Intimal damage is caused by:
- diseases associated with blood disorders (including metastatic cancer and diabetes mellitus);
- high pressure on the walls of blood vessels - arterial hypertension.
Fragility of arteries and cracks can be a consequence of hypovitaminosis.
The inner layer of the coronary and all other arteries is protected by flat blood cells - platelets. They are also responsible for blood clotting. When a microcrack appears in the intima, platelets (in large quantities) try to “seal” the damage.
Due to the identical charge of LDL molecules and platelets, excess fats are attracted to the crack, which is the beginning of the formation of cholesterol deposits. At first, a spot forms, then it increases in volume and area, turning into a plaque - an obstacle to blood flow. Then the plaque calcifies and transforms into a hard growth - the cause of NK and atherosclerotic coronary artery sclerosis.
Typical symptoms
Atherosclerotic cardiosclerosis does not have significant symptoms as long as the compensatory capabilities of the blood flow maintain oxygen delivery at the proper level to the area supplied by the affected vessel. A bright clinic is present in the case of critical narrowing of the lumen of the arteriole.
In some areas of the myocardium, over a long period of cholesterol accumulation, new bypass blood supply pathways are formed, or the plaque itself grows with its apex towards the outer wall of the vessel, while the lumen remains unchanged.
With this disease, general clinical signs of atherosclerosis will be present:
- xanthelasmas (subcutaneous accumulations of cholesterol, often around the eyes);
- xanthomas (wart-like deposits of cholesterol on the elbow and palmar bends, along the tendons);
- premature aging, skin aging;
- early gray hair;
- increased hair growth in the ears;
- chronic pancreatitis.
Manifestations of atherosclerotic cardiosclerosis in the heart are caused by a decrease in the mass of functioning muscle cells. All symptoms will indicate chronic heart failure:
- shortness of breath during exercise;
- orthopnea (dissatisfaction with breathing in a horizontal position);
- decreased tolerance to physical activity;
- general malaise, increased fatigue, drowsiness;
- swelling in the legs;
- cardiopalmus;
- attacks of dizziness, low mood;
- night cough.
Since atherosclerosis also affects large-caliber arterioles, the patient may additionally experience symptoms of angina pectoris: pain in the chest in response to physical and emotional stress, which can be relieved by taking Nitroglycerin and rest.
Gradual involvement of the conduction system in the pathological process can provoke heart rhythm disturbances:
- sinus or ventricular tachycardia;
- atrial fibrillation;
- atrioventricular block;
- Hiss bundle branch block.
Complications
Atherosclerotic cardiosclerosis leads to disruption of the rhythm of heart contractions. Due to the fact that the conducted impulse “stumbles” over a healed area of the myocardium, the heart rate is lost. Types of failures:
- bradycardia – slowing of the rhythm. HR (heart rate) less than 60 beats/min.;
- tachycardia – heart rate more than 140 beats/min. without physical activity;
- extrasystole - uneven contraction of the heart (the most characteristic pathology for cardiosclerosis);
- atrial fibrillation is a chaotic contraction (in the atria the rhythm slows down, while the ventricles contract up to 140-150 times/min.).
Reference! The normal heart rate at rest for an adult ranges from 60 to 90 beats/min.
Unstable myocardial function leads to the development of:
- CHF (chronic heart failure);
- acute necrosis of a portion of the myocardium (infarction);
- congestion in the lungs and pulmonary edema;
- cardiomyopathy;
- sudden cardiac arrest (coronary death).
The main clinical syndrome of pathological changes in cardiosclerosis is angina pectoris (an imbalance in the myocardial oxygen demand and the supply of blood to the heart muscle).
How to make a diagnosis
The diagnosis of “atherosclerotic cardiosclerosis” can only be established on the basis of a detailed examination of the patient for myocardial damage, blockage of coronary vessels and dyslipidemic changes in the blood serum.
The examination plan for a patient with suspected atherosclerotic coronary artery sclerosis includes:
- Laboratory blood test:
- cholesterol level, lipoprotein fractions;
- blood sugar, glycosylated hemoglobin (HBA1c);
- glucose tolerance test;
- biochemical study - creatinine, urea, ALT, AST;
- coagulogram, international normalized ratio (INR);
- hemoglobin, hematocrit;
- natriuretic peptide.
- Electrocardiography:
- standard at rest (12 leads);
- with dosed physical activity (bicycle ergometry, treadmill test);
- 24-hour Holter monitoring.
- EchoCG (ultrasound examination will accurately show the degree of myocardial hypertrophy, ejection fraction, size of the heart chambers, condition of the valve system). Recently, stress echocardiography has been introduced into practice - the study is performed in combination with physical activity on a treadmill or bicycle ergometer.
- Myocardial scintigraphy (OFCET, PET). The essence of the method is the intravenous administration of a radionulide marker (technetium99). The quality of the blood supply to the heart muscle is examined (the better it is, the more the radiopharmaceutical accumulates in the tissue; well-nourished areas have a bright glow). This scan in combination with stress tests has the greatest diagnostic information value.
- CT scan:
- CT visualization of the coronary arteries without the introduction of contrast - calcification index (cholesterol plaques, during their growth, go through the stage of calcium deposition in them, which can be seen on the scan);
- CT coronary angiography is a study of the coronary arteries using intravenous contrast.
- Invasive coronary angiography. The most accessible method for visualizing atherosclerotic lesions of the heart vessels. During the procedure, a conductor with a contrast agent is inserted through the femoral artery into the coronary artery and the location of the narrowing is determined using x-rays.
All cardiac imaging methods will help make a differential diagnosis between different types of cardiosclerosis (post-infarction, atherosclerotic, myocardial).
Forms of the disease
Atherosclerotic cardiosclerosis is classified according to the degree and extent of myocardial damage. There are two forms of the disease:
- Focal. Difficult to diagnose. Based on the area of damage to individual myocardial areas, it is divided into small-focal (sclerotic zone less than 2 mm) and large-focal (sclerotic zone more than 2 mm). It is practically asymptomatic until the scar lesions grow to large sizes.
- Diffuse. It is characterized by a generalized distribution of connective tissue in the myocardium. The heart muscle acquires a mixed (diffuse) structure. Scars and necrosis form in the altered areas. Extensive lesions are accompanied by severe symptoms characteristic of ischemic heart disease.
In the case when atherosclerosis develops simultaneously in the coronary arteries and the central vessel (aorta), the risk of diffuse cardiosclerosis increases. In addition, when the walls of the aorta (aneurysm) expand and stretch, due to an increase in the volume of cholesterol plaques, there is a danger of rupture of the vessel and instant death.
No ads 2
Clinical case
Since 2014, I have been seeing patient B., born in 1951, diagnosed with coronary artery disease.
Angina pectoris, functional class II. Atherosclerotic and post-infarction (2013) cardiosclerosis. Hypertension II degree. Heart failure IIA. The patient was overweight (BMI 30.4) and had been a smoker for 22 years. At the beginning of treatment, the patient complained of chest pain and shortness of breath that occurred when climbing to the 3rd floor, swelling of the legs in the evening, and general weakness. Blood pressure ranged from 150-160/90 mm. Hg Art., pulse - 89 beats/min.
Based on the results of additional studies, an increased amount of cholesterol, triglycerides in the blood was established, glucose was 5.8 mmol/l.
Over the course of 4 years of treatment, the patient managed to switch to a healthy diet, quit smoking, and lose weight by 22 kilograms. Regular physical activity helped increase exercise tolerance and stabilize blood pressure, and limiting salt and water made it possible to stop taking Furosemide and reduce the dosage of Enalapril.
At the moment, patient B.’s heart condition remains satisfactory. Episodes of taking Nitroglycerin no more than 1-2 times a week. It is possible to keep cholesterol levels below 4.9 mmol/l.
Diagnostics
The diagnosis of “atherosclerotic cardiosclerosis” is based on the results of laboratory and instrumental studies. The patient receives an appointment for tests and diagnostic procedures upon presentation of symptomatic complaints. Characteristic changes in the biochemical blood test indicate myocardial damage.
An increase in enzyme concentration is determined:
- aspartate aminotransferase (ALT);
- creatine phosphokinase (CPK);
- lactate dehydrogenase (LLH).
The lipidogram (the patient's lipid profile, which determines the quality of fat metabolism) shows a significant excess of the norm for total cholesterol, triglycerides, low and very low density lipoproteins. A general clinical blood test determines the hanging platelet count, the discrepancy between thrombocrit and platelet indices from normal values.
A number of pathological changes are recorded during a coagulogram (blood clotting test). Primary examination of the heart - ECG (electrocardiogram) reveals areas of the myocardium that have lost the ability to conduct impulses.
Depending on the nature and intensity of the violations, the following may be prescribed:
- transthoracic or transesophageal echocardiography - ultrasound of the heart with an external probe or a tubular probe through the esophagus;
- echocardiography with Doppler – examination of the aorta and coronary arteries;
- stress echocardiography – ultrasound of the heart in a calm state and after a dynamic load (physical exercise or administration of medications);
- coronography - x-ray of the coronary arteries of the heart with the introduction of a radiopaque substance.
If possible, magnetic resonance imaging or computed tomography of the cardiovascular system is performed.
Treatment and observation by a doctor
Atherosclerotic cardiosclerosis is a slowly progressive disease, the lack of treatment of which leads to failure of the heart muscle (areas of dead muscle cells are replaced by connective tissue).
Taking into account the characteristics of this condition, I highlight the main directions of treatment for the disease:
- whenever possible, compensation for the underlying disease;
- symptomatic correction (elimination of edema syndrome, restoration of rhythm, support of myocardial contractile function);
- lipid-lowering therapy;
- lifestyle modification;
- prevention of complications.
The treatment plan for atherosclerotic cardiosclerosis should include:
- A set of physical activity, quitting smoking and alcohol.
- Special diet: limiting the intake of sodium, water, unsaturated fats, gas-forming products, coffee, strong tea. Fractional 5-6 meals a day. Regular weighing.
- Lipid-lowering drugs (Atoris, Rosuvastatin).
- Diuretics (“Furosemide”, “Trifas”, “Veroshpiron”).
- ACE inhibitors (Enap, Lisinopril).
- Beta-blockers (“Bisoprolol”).
- Antiplatelet agents (Cardiomagnyl, Clopidogrel).
- If necessary: ytrates (“Nitroglycerin”);
- cardiac glycosides (Digoxin).
Treatment
Conservative treatment of atherosclerotic cardiosclerosis is aimed at eliminating the symptoms of ischemia, correcting blood composition, improving blood circulation, increasing the density and elasticity of arterial vessels.
In advanced stages of the disease, drug therapy is inappropriate. To restore hemodynamics, the patient undergoes surgery to correct the arteries. Regardless of the chosen treatment tactics, the medical diet “Table No. 10” is prescribed, intended to eliminate hypercholesterolemia.
Groups of medications
Prescribed drugs are divided into several pharmacological groups:
How to lower blood cholesterol levels?
- Statins. Slow down the production of endogenous cholesterol. As a result, the level of LDL decreases and the content of HDL in the blood compensatory increases.
- Fibrates (fibric acid derivatives). Normalize lipid metabolism and the balance of lipoproteins of different densities.
- Calcium channel blockers and angioprotectors. They tone the walls of the arteries, strengthen the endothelium, and enhance the contractility of blood vessels.
- Anticoagulants and antiplatelet agents. Reduce high blood clotting rates characteristic of coronary artery disease and its manifestations.
- Bile acid sequitrants. Stimulate hepatocytes to use excess low-density lipoproteins for bile synthesis.
- Cardiac glycosides are plant stabilizers of rhythmic myocardial contractions.
- Vitamin PP (nicotinic acid) is an active participant in lipid metabolism.
- Nitroglycerin preparations for the relief of angina attacks.
At the same time, hypertension, metabolic disorders and other chronic diseases are treated.
Diet therapy
Diagnosed atherosclerosis, as a trigger for cardiovascular pathologies, is poor eating behavior, nicotine addiction, and addiction to alcoholic beverages. First of all, cardiologist patients are advised to review their diet, quit smoking, and give up alcohol.
The diet for atherosclerotic cardiosclerosis excludes the consumption of foods rich in animal fats, baked goods, smoked products, sausages, fast food, and pickles. It is prohibited to eat foods prepared by frying (including over charcoal).
Dietary nutrition is organized on the basis of slow carbohydrates (dishes from legumes, grains and cereals), fiber and vitamins (vegetables, herbs, berries, fruits), foods rich in Omega acids (linseed oil, fish, seafood, nuts). The rules of the diet indicate adherence to the eating regimen (every 3-4 hours in small portions).
A short list of products for atherosclerotic disease
Beverage classification
| Refuse | Introduce into your diet on a regular basis |
| coffee | freshly squeezed fruit and vegetable juices |
| alcohol (any strength) | berry compotes and jelly |
| energy | decoctions of rosehip, linden |
| sweet cocktails and juices |
When compiling a daily menu, special attention should be paid to compliance with the daily calorie intake and the ratio of nutrients.
Surgical intervention
With intense negative dynamics of the disease, surgical methods are used in treatment. Depending on the progressive changes, one of the following types of surgery may be prescribed:
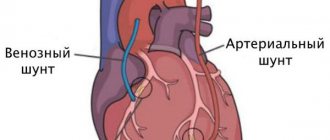
- coronary bypass surgery - creation of an artificial channel for blood flow bypassing the atherosclerotic section of the coronary artery;
- aneurysm resection – excision of the damaged area of the aorta of the heart followed by prosthetics;
- RFA (radiofrequency ablation) – endoscopic cauterization of a section of the myocardium that blocks cardiac impulses;
- angioplasty of coronary vessels with stenting - dilation of arteries by installing a wall.
In difficult cases, an electrical pacemaker (ECS) is implanted.
Prevention of deterioration of the condition
The clinical picture of coronary sclerosis worsens as cholesterol plaques and foci of fibrosis grow. All preventive measures are aimed at maximizing the preservation of myocardial contractility - preventing the progression of heart failure.
In addition to well-chosen drug therapy and control of risk factors, the patient may need:
- implantation of a cardioverter-defibrillator;
- placement of an artificial pacemaker;
- surgical methods of myocardial revascularization (stenting, coronary artery bypass grafting).
Publications in the media
Atherosclerosis of the coronary arteries with their hemodynamically significant stenosis leads to the emergence of various clinical variants of coronary heart disease (see Coronary heart disease) • In addition to atherosclerosis (more than 90% of cases of coronary artery disease), coronary artery disease can be caused by arteritis, collagenosis, thrombosis and embolism, anomalies in the development of coronary vessels and etc.
Frequency - see Coronary heart disease.
The etiology in most cases is unknown • The main role, apparently, belongs to various disorders of lipid metabolism (see Hyperlipidemia), detected in almost all patients with coronary artery disease • In some cases, atheromatosis is accompanied by diffuse distal sclerosis of the coronary arteries without local lipid infiltration of their wall (X- syndrome).
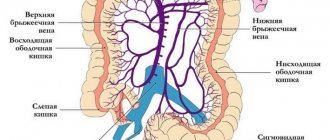
Pathophysiology • The heart requires 0.1–0.2 ml of oxygen per 1 g of weight per minute. Such intense gas exchange is possible due to the high perfusion pressure in the coronary arteries arising directly from the aortic ostium, the high inflow volume of 5% of the bcc, and the increased extraction of oxygen by the myocardium (more than 75% at rest and almost 100% at maximum load) • With stenosis of the coronary arteries of less than 70–75% of their lumen, disturbances in myocardial perfusion occur only during exercise, and at rest the decrease in perfusion does not exceed 5% of normal values • Even with complete occlusion of one of the main coronary arteries, the level of perfusion of the “compromised” myocardial zone is reduced by only 50 % due to collateral circulation • With hemodynamically significant stenoses of several coronary arteries, the dependence of impaired myocardial perfusion at rest on the degree of stenosis is almost linear, therefore multi-vessel damage is always associated with a worse prognosis • As a rule, even in the area of the previous infarction, a certain amount of viable myocardium remains (see . Heart disease is ischemic), therefore revascularization interventions improve the contractile function of the heart even in the area of infarction • When assessing the degree of damage to the coronary bed by atherosclerosis and choosing tactics, the following classification is used.
Classification of atherosclerosis of the coronary arteries (Petrosyan-Zingerman) • Anatomical type of blood supply to the heart •• Predominantly left (about 10%) •• Predominantly right (85–90%) •• Balanced (about 5%) • Localization of the lesion •• Trunk of the left coronary artery (CA) •• Anterior interventricular branch •• Circumflex branch •• Diagonal branch •• Right CA •• Blunt edge branch •• Other arteries • Extension of lesion •• Local stenosis •• Diffuse stenosis • Localization of stenoses •• Proximal segment of artery •• Middle segment of the artery •• Distal segment of the artery • Degree of luminal stenosis •• Without stenosis •• Moderate (less than 50%) •• Severe (less than 75%) •• Severe (from 75% to subtotal stenosis) •• Occlusion • Collateral blood flow • • Anastomoses between the anterior interventricular and circumflex branches •• Anastomoses between the circumflex branch and the right coronary artery •• Anastomoses of the circle of Viessen-Tebezia •• Other anastomoses.
Clinical picture and diagnosis.
• Complaints and objective examination - see Coronary heart disease.
• Instrumental methods •• ECG, chest x-ray, echocardiography, radioisotope study, stress tests - see Ischemic heart disease •• Intravascular ultrasound of the coronary arteries ••• Indications: •••• stenting of narrow coronary arteries; •••• restenosis after stent implantation; •••• unsatisfactory results of percutaneous transluminal coronary angioplasty; •••• questionable stenoses, especially of the trunk of the left coronary artery; •••• stenosis and implantation of stents in the mouths of arteries; •••• the need to assess the extent of stenosis and vessel diameter before endovascular interventions; •••• additional indications are under development ••• Methodology •••• Determine the cross-sectional areas of the coronary artery, the degree of stenosis, the transverse area of the residual lumen in the area of maximum stenosis, the length and eccentricity index of the plaque •••• If three-dimensional reconstruction is possible determine the volume of the plaque and its structure throughout •••• A study in color Doppler mapping mode is carried out when there are difficulties in interpreting the area of the lumen of the vessel that arise in the area of lipid plaques with a thin cap, and during coronary artery stenting, when measurements of the coronary artery lumen in the area of implantation can be significant influence further tactics •• Ultrasound of coronary bypass grafts ••• Indications •••• Transthoracic ultrasound of pedicle coronary bypass grafts is performed for all patients in the immediate period after coronary bypass surgery •••• Intravascular ultrasound of coronary bypass grafts is performed for endovascular correction of coronary bypass graft stenoses in the postoperative period •••• Additional indications are under development ••• Technique •••• Transthoracic ultrasound of pedicled mammarocoronary bypass grafts, pedicled coronary artery bypass grafts from the gastroepiploic artery, as well as intravascular ultrasound of coronary bypass grafts are feasible in almost all patients ••• • Transesophageal and transthoracic ultrasound of autovenous coronary artery bypass grafts appear to be futile •••• Transesophageal and transthoracic ultrasound of autoarterial coronary artery bypass grafts is under development •• Ultrasound of arteries and veins used as coronary artery bypass grafts ••• Performed in all patients before coronary artery bypass grafting ••• Determine the presence of the corresponding arteries, their diameter, length, their possible stenosis in case of damage by atherosclerosis or other pathological processes, anomalies in the development of arteries, volumetric blood flow in them ••• When using saphenous veins of the lower extremities as coronary bypasses, diagnose varicose veins ••• When using internal mammary arteries as shunts, ultrasound of the subclavian arteries is also performed ••• When ultrasound of the radial and ulnar arteries is performed, the Allen compression test is performed to determine the anatomical type of blood supply to the hand •• X-ray contrast selective coronary angiography ••• Indications: performed on all patients, initially admitted with a diagnosis of myocardial infarction, who have suffered acute coronary events, with clinical symptoms in patients with chronic forms of coronary artery disease, as well as with positive results of stress testing ••• Methodology •••• Typically, radiopaque selective coronary angiography is performed from a transfemoral approach, but with severe atherosclerosis of the femoral arteries, it can be performed from other approaches •••• In most cardiological centers, catheterization of the coronary arteries is carried out using the Judkins controlled catheter technique •••• The study reveals the indicators indicated in the heading Classification of atherosclerosis of the coronary arteries •••• When planning endovascular treatment, except assessment of the localization and degree of stenosis of the coronary artery, the presence, severity of calcification and angioarchitecture of the coronary arteries (in particular, tortuosity of the artery, lateral branches, etc.) are important in the area of possible transcatheter correction •••• When planning coronary bypass surgery, information about the structural and morphological features is obtained coronary artery distal to the stenosis, where a coronary bypass can be applied, as well as the functioning of collateral circulation in the area of impaired myocardial vascularization.
TREATMENT
Drug therapy - see Coronary heart disease.
Surgery.
• Indications: in general, the indications are determined by the anatomical type of coronary atherosclerosis, left ventricular function and, to a much lesser extent, the clinical picture of the disease.
• General indications for endovascular treatment •• One- or two-vessel coronary artery disease with stenosis or occlusion of type A or B according to the classification given below •• The introduction of new methods of endovascular treatment (stenting, laser revascularization) allows interventions in some cases with type stenosis WITH.
• Angiographic characteristics of stenoses by type •• Type A (minimal complex) ••• Local (less than 10 mm) ••• Concentric ••• Easily passable ••• Non-curved segment (<45°) ••• Incomplete occlusion ••• No major branches in the area of stenosis ••• No thrombosis ••• Smooth contour ••• Little or no calcification •• Type B (medium complex) ••• Tubular (10–20 mm) ••• Eccentric ••• Slight tortuosity proximal segment ••• Slightly curved segment (45–90°) ••• Total occlusion less than 3 months ••• Stenosis at the bifurcation, requiring the use of two guidewires ••• Thrombosis ••• Irregular contour ••• Moderate or severe calcification •• Type C (severe complex) ••• Diffuse (more than 20 mm) ••• Eccentric ••• Marked tortuosity of the proximal segment ••• Very curved segment (>90°) ••• Total occlusion, existing for more than 3 months, with developed collaterals ••• Impossibility of bypassing all major branches in the area of stenosis ••• Thrombosis ••• Irregular contour ••• Severe calcification.
• Contraindications to endovascular treatment •• Absolute: end-stage circulatory failure •• Relative ••• Type C stenoses ••• Poor short-term prognosis for life due to concomitant diseases (for example, malignant neoplasms with distant metastasis) ••• Diffuse distal sclerosis coronary arteries (X-syndrome).
• Specific complications of endovascular treatment •• Perioperative MI due to dissection, intimal volvulus, spasm or thrombosis of the coronary artery •• Restenosis due to progression of atherosclerosis, arteritis or hyperplastic reaction in the area of stent implantation •• False aneurysms at the access site •• Adverse reactions associated with use contrast media.
• General indications for coronary artery bypass grafting •• Hemodynamically significant stenosis of the trunk of the left coronary artery •• Variant of the trunk lesion (stenosis of the anterior interventricular branch, circumflex branch, right coronary artery) •• Two-vessel and single-vessel lesion with hemodynamically significant proximal stenosis of the anterior interventricular branch •• Two-vessel lesion without proximal stenosis of the anterior interventricular branch with a decrease in the contractile function of the left ventricle, severe ischemia, tolerant to conservative treatment, and also when stenotic vessels supply blood to a large volume of viable myocardium •• MI during the course or relapse of MI, refractory to intensive conservative therapy •• MI accompanied by left ventricular insufficiency in the presence of coronary artery stenosis, providing blood supply to viable myocardium beyond the developed necrosis •• Coronary artery bypass grafting as a primary reperfusion strategy in the early stages (no later than 6–12 hours) MI with ST segment elevation •• One- or two-vessel lesion that caused the onset life-threatening ventricular arrhythmias, especially if the patient has undergone resuscitation for arrhythmic cardiac arrest or there is sustained ventricular tachycardia •• Failure of percutaneous transluminal coronary angioplasty with persistent ischemia threatening coronary artery occlusion involving a significant volume of myocardium in the risk area •• Foreign body in the coronary artery in a position that threatens cessation of blood flow •• Ischemia of viable myocardium, tolerant to drug and endovascular correction, outside the blood supply zone of a functioning mammarocoronary shunt to the anterior interventricular branch.
• Contraindications to coronary artery bypass grafting •• Absolute: end-stage circulatory failure •• Relative: diffuse distal sclerosis of the coronary arteries (X-syndrome); unfavorable short-term prognosis for life due to concomitant diseases (for example, malignant neoplasms with distant metastasis).
• Specific complications of coronary artery bypass surgery •• Perioperative MI •• Osteomyelitis of the sternum with flap isolation of both internal mammary arteries •• Ischemia of the hand after isolation of the radial artery with a predominantly radial type of blood supply to the hand.
Prognosis • Has a pronounced dependence on the anatomical variant of the lesion of the coronary arteries, left ventricular function, the presence of rhythm disturbances and concomitant pathology • Surgical treatment has little effect on the prognosis for life expectancy, with the exception of cases of three-vessel and stem lesions • Coronary artery bypass grafting has advantages over endovascular correction in in terms of quality of life, frequency of restenosis and the need for repeated interventions • Endovascular treatment has advantages over coronary artery bypass surgery in terms of the duration of hospital treatment, its cost (in Russia this is true only if intervention on one vessel is necessary).
Synonyms: Coronary heart disease, Coronary disease (heart).
Abbreviations • CA – coronary artery
ICD-10 • I25.1 Atherosclerotic heart disease
Expert advice
The success of treatment, the duration and quality of life of the patient largely depend on his motivation and ability to change his attitude towards himself.
I recommend that my patients follow several rules.
Methods for treating atherosclerosis of the coronary vessels of the heart
The patient's priority problem with atherosclerosis of the coronary arteries is the formation of plaques, which can lead to blockage of vital arteries. Therefore, treatment is aimed both at eliminating existing calcifications and at preventing the formation of new ones.
According to clinical recommendations, for atherosclerosis of the coronary arteries, drugs that reduce the level of harmful fats are prescribed; they are successfully used, influencing the first link of the mechanism of plaque formation: statins, fibrates, bile acid sequesters.
In particularly difficult cases, an operation can be performed in which the affected artery is cut and the growths are removed, sometimes part of the artery is removed.
Treatment can only be prescribed by a doctor after appropriate diagnosis. The patient can only follow the rules of prevention.
Causes
As stated above, the cause of atherosclerotic cardiosclerosis is insufficient blood supply to the myocardium, in which the muscle cannot contract normally, and its damaged areas are replaced by connective tissue. The root cause of impaired blood flow is plaques that cause narrowing or blockage of heart vessels. This disease is called atherosclerosis. It is accompanied by the formation of excess cholesterol contained in the blood on the walls of the arteries. We mentioned in detail what factors cause atherosclerosis in a previous publication.