Treatment of dry and wet gangrene in the 21st century does not require amputation, and the experience of our center shows this. In most surgical departments of the country, gangrene still remains a disease with a high rate of amputation and death.
Simply restoring blood flow does not allow one to count on rapid closure of tissue defects in the foot and leg. In some cases, the process of necrosis affects bone and tendon structures and independent healing is impossible. In such cases, our specialists are helped by plastic microsurgery methods. The clinic has introduced technologies for transplanting free flaps of tissue on a vascular pedicle. That is, we take skin or muscle on a feeding vessel from an area of the body where there is a lot of skin, fatty tissue and soft tissue, and then we transplant this complex of tissues to the site of a large defect, achieving healing of post-necrotic wounds in most patients.
The use in medicine of modern methods of restoring blood circulation in the limb and reconstructive plastic surgery technologies makes it possible to save the leg and the ability to walk for the vast majority of patients. Such technologies are concentrated in specialized limb salvage centers, such as the Innovative Vascular Center.
Gangrene can be cured and it is actually very simple. After all, it is enough to restore blood flow to the leg, remove dead tissue and heal the remaining wounds. However, these simple principles are still practically not followed anywhere, because some doctors and departments restore blood flow, while others deal with the wound process and removal of dead tissue.
For the treatment of dry gangrene of the lower extremities, they offer a variety of droppers, blood thinners, vasaprostan and other miracle remedies. And when it really becomes clear that such treatment for gangrene of the legs does not eliminate the symptoms, then in a regular surgical department one remedy is used - high amputation.
This outcome encourages patients and their relatives to seek methods of treating gangrene without surgery. Various “folk” remedies are used, from which the infection only flourishes. This includes chewed bread crumbs, salt and urine, and many other “remedies for gangrene” applied to the affected areas. From them, the inflammatory process develops and spreads faster, inevitably leading to amputation for health reasons.
In such a development of events, in most cases, doctors are indirectly to blame, who perceive any tissue necrosis as the need to “save the patient” with the most radical method of treatment. They either do not know information about modern technologies, or they do not believe in it and do not convey it to patients.
Gangrene can be treated without amputation at the Innovative Vascular Center
Treatment of gangrene without amputation in Moscow is carried out in a specialized hospital of the Innovative Vascular Center - the Clinic of Innovative Surgery (CIS). In 2011, according to the ROASH report, our clinic took a leading position in performing vascular reconstructions on the arteries of the leg and foot.
The Innovative Vascular Center is a clinic in Russia where modern high-tech methods of restoring blood flow in the legs, advanced technologies of X-ray endovascular surgery, vascular and reconstructive plastic microsurgery are put into use.
Every year we successfully operate on more than 650 patients with critical ischemia and gangrene of the legs. Modern treatment of gangrene can be carried out by a team of experienced vascular and endovascular surgeons, as well as doctors skilled in the management and closure of necrotic wounds. Such a team can achieve impressive results in the treatment of gangrene. This team must include specialists who not only know how to restore blood flow, but who also know how to treat a patient with multiple vascular lesions, severe comorbidities and serious wound complications.
Wet gangrene, necrosis, long-term non-healing wounds, and black color of the finger are not a reason for amputation for our team, but should be the reason for active surgical tactics to save the limb. We manage to save the leg in most patients with threatening limb ischemia. We are fighting to save our leg until the last possible moment.
In many other “limb salvage centers” there is a separation of vascular, endovascular and reconstructive plastic surgery, so there is no possibility of a holistic approach to the treatment of critical limb ischemia.
In what cases should you urgently consult a doctor?
There are a number of symptoms, the appearance of which may indicate a predisposition or the onset of gangrene of the leg in an elderly person, and requires contacting a medical institution for consultation and diagnosis of the disease:
- constantly cold feet (even in the summer heat);
- fatigue when walking and pain in the legs;
- cramps in the limbs;
- poor healing of even minor wounds;
- loss of sensation in the affected area;
- change in the skin from pale to bluish or marbled, and then to black (in later stages of the disease);
- the patient's refusal to eat and drink;
- non-healing ulcers.
Under no circumstances should these symptoms be ignored. There is a very fine line between dry and wet gangrene, which develops rapidly and poses a threat to the life of an elderly person, especially if the elderly person has high blood sugar. Immediate consultation with a doctor, prevention and treatment will help prevent the development of a serious illness leading to disability and death.
Why are there problems in Russia with treating gangrene without amputation?
- Vascular surgeons in most clinics in our country are afraid of purulent-necrotic wounds like fire and do not accept patients with necrosis on the foot. After all, they deal with “pure” pathology and are afraid of spreading the infection. As a result, only a few clinics perform vascular surgery for gangrene in Russia. The main problem of vascular and surgical departments is that their doctors have little knowledge of what gangrene of the legs is, symptoms, signs and methods of treatment. Severe pain, symptoms of intoxication, even with the development of dry gangrene of the toe are a contraindication for them to perform vascular surgery. Unlike gas gangrene in diabetes mellitus, in dry gangrene there is no reason to fear the spread of infection, since the pathological process occurs only in a certain segment of the limb.
- Endovascular surgeons deal with the problem of chronic arterial insufficiency by eliminating blockages in blood vessels. However, if angioplasty and stenting fail, the situation usually worsens and an open intervention must be done immediately, but they do not know how to do this. While the patient gets to vascular surgeons, the leg may die. Having restored blood flow through the arteries, endovascular surgeons consider their task completed, because they do not deal with wound processes and send patients to the purulent surgery department, where their leg is easily amputated, despite good blood flow. When you ask the endovascular surgeons of the federal centers what gangrene of the legs is, its symptoms and treatment, they will not answer you, because there are still no quotas for the treatment of critical ischemia, so the federal center is simply not interested in treating such patients.
- General surgeons in departments of purulent surgery have no idea about the level of blood supply to tissues and do not know the methods of reconstructive plastic surgery that allow closing large wound defects. For them, there is no better treatment for gangrene than to do amputation, as high as possible, in order to forget about a difficult patient. They consider even the first signs of gangrene in the initial stage to be a threat to the patient’s life and suggest amputating the leg, fearing possible blood poisoning.
Symptoms and complications
Areas affected by gangrene are usually warm and swollen.
The skin may be pale at first, but soon turns red or brown and finally greenish-black. The affected area may become severely scarred and require reconstructive surgery. If significant tissue death occurs, the affected body part may even need to be removed. Sometimes a brown liquid forms under the skin, causing large blisters to grow. If clostridia is the cause of gangrene, gas produced by the bacteria may be seen in these blisters.
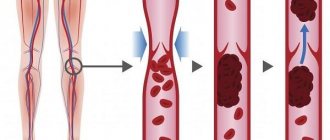
Substances produced by bacteria are very toxic to human tissue and kill healthy cells by reducing oxygen levels. If the infection does not stop, these bacterial toxins will soon enter the bloodstream and begin to poison vital organs (so-called toxic shock), causing immediate kidney failure.
Gangrene of the lower extremities treatment with modern methods
The approach to treating gangrene varies depending on its causes. In our clinic, the treatment of choice for gangrene of the leg is treatment without amputation. Every year, patients with critical ischemia who have already been sentenced to amputation in other vascular and surgical departments are operated on in the hospital of the Innovative Vascular Center. For most of them, we manage to keep their legs and the ability to walk. The main reason for our success is the use of advanced technologies and the narrow specialization of our vascular surgeons.
Establishing diagnosis
Gas gangrene is characterized by a necrotizing (flesh-destroying) bacterial infection that can be recognized by a doctor. The doctor will take a tissue sample or perhaps some fluid from the blisters. The sample is tested in the laboratory. However, treatment will not wait for results. The doctor will immediately begin giving you a broad-spectrum antibiotic.
If the infection is severe, sometimes an X-ray or MRI of the soft tissue is used to detect gas deep under the skin. If surgery is required, these scans will indicate exactly where the bacteria are and what needs to be removed.
Hybrid surgery in the treatment of dry gangrene without amputation
This is the combined use of bypass surgery and angioplasty to solve the problem of restoring blood flow within a single intervention. Hybrid surgeries are performed in our clinic to achieve optimal clinical results for complex vascular lesions. They expand the possibilities of vascular surgery and allow us to save the leg in the vast majority of patients with gangrene. A shunt works well only when the artery above and below it is well patent. If there are atherosclerotic plaques and narrowings above or below the shunt, then blood stagnates in such a shunt and thrombosis occurs. A shunt to treat gangrene allows you to bypass long-term blockages in the arteries, and then by performing angiography and angioplasty below the shunt, we ensure unimpeded blood flow to the foot and toes. The use of such tactics allowed us to save the leg in 96% of patients with impending ischemia.
CAUSES
Gangrene can develop for one or more reasons:
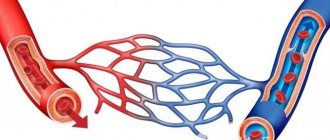
- Lack of blood supply.
Blood provides oxygen and nutrients to cells, as well as components of the immune system and antibodies that prevent infections. Without proper blood supply, cells cannot survive and tissues are destroyed. - Infection.
If bacteria multiply unchecked for a long time, the infection itself can lead to tissue necrosis, causing gangrene.
Prognosis after gangrene treatment
The clinical outcome that gangrene leads to depends on the condition of the internal organs (heart and kidneys) and the form of gangrene. The causes of soft tissue gangrene in most cases are associated with the processes of gradual blockage of blood vessels, which develops not only in the arteries of the legs, but also in other vascular systems (brain, heart, abdominal organs). Life expectancy after reconstructive vascular operations depends on possible vascular accidents in other areas (myocardial infarction or ischemic stroke), but it has been established that after amputation of one leg, 70% of patients die in the next two years, and after successful vascular operations, long-term mortality is not more than 10% per year.
Diagnostics
Diagnosis of gangrene is not difficult and includes:
- Inspection of the affected area (visual);
- Arterio- or phlebography;
- Ultrasound Doppler examination of blood vessels;
- Rheovasography;
- CT and MRI;
- Duplex scanning with contrast agent;
- General blood analysis;
- Blood chemistry;
- Bacteriological examination of biomaterial taken from the affected area.
A correct diagnosis can be made in all cases.
PREVENTION
Here are some tips to help you reduce your risk of developing gangrene:
If you have diabetes, inspect your hands and feet daily for cuts, sores, and signs of infection such as redness, swelling, or discharge. Ask your doctor to examine your hands and feet at least once a year.
Carrying extra pounds not only increases your risk of developing diabetes, but it also puts pressure on your arteries, reducing blood flow and increasing the possibility of infection and slow wound healing.
Chronic use of tobacco products can damage blood vessels.
Wash open wounds with mild soap and water and try to keep them clean and dry while they heal.
Frostbite on the skin can lead to gangrene; frostbite reduces blood circulation in the affected area. If you notice that any area of your skin is pale, hard, cold, or numb after prolonged exposure to cold temperatures, consult your doctor.
FORECAST
Typically, people with dry gangrene have a better prognosis because dry gangrene is not associated with a bacterial infection and spreads more slowly than other types of gangrene. However, when infected gangrene is diagnosed and treated quickly, the likelihood of recovery is greater.
Older people, people who are immunocompromised or have underlying health conditions (such as diabetes, atherosclerosis, or some types of cancer), and those who seek medical help for advanced cases of gangrene are more likely to have complications from gangrene.