Treatment tactics for spinal stenosis can be conservative (without surgery), interventional or surgical. Stenosis
is a chronic degenerative process in which the intervertebral foramen, central spinal canal, or lateral recess gradually narrows.
Ultimately, this leads to compression (squeezing) of the spinal cord roots and nerve endings. The patient experiences severe pain in the back or neck, numbness and weakness of the limbs, and other neurological symptoms listed below. The disease progresses due to the fact that fragments of growing cartilage or bone tissue (osteophytes) and hypertrophied soft tissue (ligaments and muscles) wedge into the space occupied by the nerve roots.
Degenerative spinal stenosis is caused by injuries, genetics, metabolic disorders, osteochondrosis, arthrosis or other diseases of the musculoskeletal system. In the initial stages of the degenerative cascade, symptoms of spinal stenosis may not bother you at all. However, if the situation worsens over time, then it is no longer possible to cure the disease without surgery. Removal of stenosis is possible only surgically. In this case, non-traumatic spinal surgeries are performed to decompress (and sometimes stabilize) the deformed segment.
Relative stenosis
The central spinal canal narrows to 12-10 mm.
Treatment of relative stenosis without surgery often gives good results.
The patient is prescribed complex therapy, which includes medications (NSAIDs, NSAIDs), physiotherapy, and exercise therapy. In our clinic, specialists from the Pain Treatment Center will help you choose an effective treatment strategy for central relative stenosis. Don't put off seeing a doctor. Degenerative stenosis does not go away on its own. Over time, the disease worsens and at the next stage causes back or neck pain, and sometimes also neurogenic intermittent claudication syndrome (for example, with lumbar stenosis L3, L4, L5
), paralysis of the limbs.
Diagnostic measures
In order to determine spinal stenosis, the doctor collects information about the symptoms, their severity, medical history, and also conducts a physical examination to study the neurological status.
To accurately diagnose the disease, a specialist may order a patient examination by:
1. X-ray. Thanks to radiography of the spinal column, it is possible to determine the presence of bone changes - bone spines (osteophytes), due to which the space in the spinal canal narrows.
2. MRI (magnetic resonance imaging). This diagnosis involves the use of a powerful magnet and radio waves to obtain a cross-section of the spinal column. The procedure helps to identify disorders in the discs and ligamentous tissue, and the presence of tumors. The main thing that can be determined using MRI is the exact localization of the narrowing of the nerves in the spinal cord.
3. Computed tomography or CT myelogram. If there are contraindications for performing an MRI, the doctor recommends a CT scan to obtain detailed transverse visualization of the spinal column. A CT myelogram involves the administration of a contrast agent before diagnosis. Such a study helps determine the extent of the disease, which is required to prepare the patient for surgery.
Absolute stenosis
The central spinal canal narrows to 10 mm or less. Treatment of absolute stenosis with conservative methods sometimes no longer gives the desired effect. At this stage, pain in the limbs becomes a serious obstacle to an active life. Especially if the patient has neurological symptoms: pain radiates to the legs and hips, there is a feeling of muscle weakness, and the sensitivity of the limbs decreases. Unlike relative stenosis, absolute stenosis is characterized by pronounced clinical symptoms and may be an indication for spinal surgery. Expansion of the central spinal canal by surgery may be most appropriate, since there is a serious risk of complications without surgery. For example, irreversible paralysis of the limbs, which occurs due to vascular ischemia and circulatory disorders in the spinal root.
Causes of occurrence and development
Before starting treatment for lumbar or cervical spinal stenosis, you should find out what causes the onset and development of the disease.
A congenital or primary type of stenosis is formed during the intrauterine development of the human embryo. This happens in the period from 3 to 6 weeks of development. The genetic factor plays a role here. But absolute spinal canal stenosis can also develop due to infectious, toxic factors that affect the fetus.
Also the cause of congenital stenosis is:
- chondrodystrophy or achondroplasia (chronic). This manifests itself in intrauterine bone growth disorder. In this case, the spinal canal narrows due to shortening or thickening of the vertebral arches, fusion of the vertebrae themselves;
- Diastematomyelia. It is characterized by bifurcation of the spinal cord, separation of the spinal canal by a septum (it consists of either bone or cartilage tissue).
Secondary spinal stenosis appears and develops in childhood or in adulthood.
The following reasons may contribute to this:
- traumatic displacement of the vertebrae or intracanal hematomas;
- changes in the intervertebral joints, which manifest themselves in the growth of bone tissue inside the spinal canal. These changes are degenerative-dystrophic in nature;
- anatomical defect of the spinal arch;
- intervertebral hernia;
- inflammation in ankylosing spondylitis (in this case, the capsules of the intervertebral joints thicken);
- Forestier's disease;
- cysts and tumors that appear inside the spinal canal.
Regardless of the cause, treatment for spinal stenosis should begin as soon as the disease is detected.
Lumbar stenosis
An extremely common type of degenerative stenosis, which is diagnosed in 85-90% of cases. Symptoms significantly reduce the patient’s quality of life, since lumbar stenosis is characterized not only by pain in the back and lower back, but also in the limbs. Very often manifests itself as a syndrome of neurogenic intermittent claudication. The patient feels weakness, numbness and pain in the legs. It is important to understand that paresis of the limbs is completely reversible only with timely treatment. The most common clinical cases include L3 - L4 or L5 - L4 stenosis (low back pain radiating to the leg). Another common variant is L5-S1 spinal canal stenosis. At this level, the lumbar region passes into the sacral region, that is, it is a fairly mobile and susceptible to load segment. With lumbar stenosis L5 - S1, the patient also suffers from pain that “radiates” to the legs.
If there are indications for surgery for lumbar stenosis, neurosurgeons at the Pirogov Clinic perform them using the latest endoscopic technology or microsurgical instruments. This eliminates the need for additional installation of implants and metal structures. Thus, patients recover in a short time - without heavy rehabilitation.
Treatment methods
Spinal stenosis can be treated conservatively or surgically. But inexorable medical statistics indicate that only 32–45% of patients experience positive dynamics due to the use of medications, physiotherapy and exercise therapy. But even in such situations, treatment of stenosis without surgery does not lead to recovery, but only contributes to a slight improvement in the condition, especially if stenosis of the left or right root canal L5-S1 or another segment is diagnosed.
Conservative therapy includes:
- taking individually selected drugs from the group of NSAIDs, muscle relaxants, vitamins, drugs to improve blood flow, chondroprotectors, etc.;
- blockades with anesthetics;
- corticosteroid injections;
- phonophoresis;
- magnetic therapy;
- SMT therapy;
- Exercise therapy.
Therefore, today the only way to avoid the development of complications and achieve complete elimination of unpleasant symptoms is surgical treatment. Stenosis surgery is designed primarily to eliminate those factors that led to compression of the spinal cord and its nerve roots. For this purpose, decompression operations are performed. During these procedures, the herniated disc or vertebral arch that causes canal stenosis is removed. If necessary, stabilization of the spine is performed in order to fix the vertebrae in the anatomically correct position and avoid their displacement in the future, i.e., to prevent relapse.
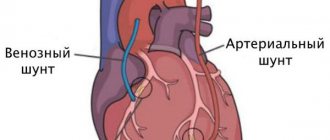
Decompression interventions
Initially, decompression interventions are used to eliminate the effect of compression of the spinal canal. Today, in the arsenal of spinal surgeons there are 3 types of techniques that are used for disc herniation with stenosis, including L5-S1:
- Classic discectomy is an operation that involves removing the entire intervertebral disc through an incision of up to 10 cm. It is indicated for anterior compression of the spinal cord by a herniated protrusion of the intervertebral disc, including if there are 2 hernias and stenosis. Although there are more gentle methods for removing pathological formations, open discectomy leaves no chance for their re-formation in the same area of the spine, which completely eliminates the risk of relapse of the disease. A titanium implant (cage) is installed in place of the removed disc, providing reliable support for the vertebrae.
- Microsurgical discectomy - surgical intervention has the same goals as open surgery, but is carried out with special instruments through a miniature incision, the length of which does not exceed 3 cm. Therefore, after it, patients recover easier and faster. But microsurgical discectomy does not allow fixation of the vertebrae with anterior stabilization systems, which is necessary when spinal stenosis and hernia are interrelated.
- Decompression laminectomy – This operation is used for posterior compression of the spinal cord. It consists of partial removal of the vertebral arches in the affected area, followed by stabilization of the spinal column with special structures.
All types of surgical interventions are performed in the medical field. Some of the best spinal surgeons in Moscow are capable of performing operations of any degree of complexity, and the availability of modern equipment makes it possible not only to accurately pre-assess all the risks and potential benefits of each procedure, but also to perform it with precise accuracy.
Stabilizing interventions
After compression of the spinal cord is removed, surgeons must fix the spine in a physiological position and create optimal conditions for proper load distribution during physical work. Depending on the location of the narrowing, the following can be used:
- Systems that stabilize the anterior support columns are cages with bone chips.
- Posterior stabilization systems – used for fixed connection of vertebral bodies, titanium structures for transpedicular fixation.
Both options for stabilizing systems are considered the optimal treatment option for the disease. Interbody cages allow you to reliably fasten the anterior column of the spinal column and prevent relapse of the disease, and transpedicular implants reliably stabilize the spine, preventing it from moving.
Special dynamic stabilization systems are also used. There are several types of such structures, each of which has its own strictly limited scope. This:
- Interspinous U-implants – systems of this kind are designed for dynamic fixation of the spinous processes of the lumbar spine, including spinal canal stenosis at the level of L3–L4, L4–L5, which may be an indication for their installation. The U-system allows you to slightly reduce the load on the posterior support columns and increase the area of the spinal canal, thereby relieving pain caused by spondylous joints of the vertebra.
- A transpedicular fixation system with nontinol rods is also indicated for installation in the lumbar spine for reliable connection of adjacent vertebral bodies. This system makes it possible to maintain a large range of movements, due to which motor abilities are practically not limited.
- Dynamic interbody implant – designed for installation in place of a removed disc when spinal canal stenosis of the cervical or lumbar spine is diagnosed. Its design features allow you to maintain a fairly good range of motion.
Their disadvantage can be considered the impossibility of use in cases of spinal instability, since they do not provide a pronounced therapeutic effect and are unable to hold the vertebrae in the desired position. Also, over time, their mobility is lost.
Cervical stenosis
Less common than lumbar stenosis. However, due to the high mobility of the segment and its comparative fragility, spinal surgery (endoscopic or microsurgical) may require additional installation of an intervertebral disc implant or interbody cage. This is necessary to stabilize the spinal segment and prevent the development of degenerative complications in the future. With cervical stenosis, local pain occurs, radiating to the arms and atrophy of the muscles of the upper extremities. Neurosurgeons at the Pirogov Clinic prefer minimally invasive endoscopic operations and interventional pain treatment, which avoid traumatic operations with the installation of metal structures.
If you have been diagnosed with cervical stenosis and have been experiencing pain that is resistant to conservative therapy for more than 12 weeks, send the images to your neurosurgeon through a special form on our website to clarify which treatment would be most appropriate in your case.
Possible complications
The disease must be treated on time. If you do not do this, changes will appear, many of which will become irreversible:
- Partial or complete immobilization of the legs.
- The patient does not feel pain, cold, or warmth. Or there is sensitivity, but it is reduced.
- Gradual atrophy of the leg muscles occurs.
Lateral and central stenosis is a serious disease that should only be treated by a doctor. After thorough examinations, he will select the optimal therapy, help relieve pain, improve blood flow, and cure concomitant diseases. You should not self-medicate, but after consulting with a doctor, you can undergo physical therapy, therapeutic massage, perform special exercises, and also use compresses and lotions with decoctions of medicinal herbs.
Symptoms of spinal stenosis
- Pathological compression of the nerve roots, which leads to their ischemia, causes specific symptoms of spinal stenosis:
- Back pain that occurs when walking and radiates to the legs (legs, front or back of the thigh);
- Numbness and discomfort in the legs occur with a certain position of the spine (bending the torso, walking down the stairs, prolonged static standing position);
- Back pain becomes less intense or disappears altogether with a certain position of the spine (for example, if the patient is sitting, bending or squatting);
- Muscle weakness, numbness and decreased sensitivity of the limbs are especially noticeable after physical activity;
- Problems with urination and bowel movements;
- Problems with potency and erectile dysfunction.
- If, along with severe pain and paresis of the limbs, the patient experiences the last 2 symptoms, emergency spinal surgery may be necessary.
MRI images BEFORE
and
AFTER
surgery for foraminal spinal stenosis using the endoscopic method.
The roots are marked in red (dots and lines). Blue color shows the bone-ligamentous structures that compress the root. The green arrow, as well as the white color in the pictures, shows the free space for the spine. The goal of the operation has been achieved! Endoscopic decompression was performed by a neurosurgeon, a doctor of the highest category, candidate of medical sciences. Sciences Meredzhi Amir Muratovich
.
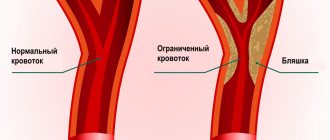
Degenerative diseases
Spinal stenosis most often occurs due to degenerative changes that occur as a result of aging. But degenerative changes can be due to morphological changes or an inflammatory process. As the body ages, the ligaments thicken and calcify (formation of a depot of calcium salts inside the ligaments). Growths also occur in the area of the vertebrae and joints - these growths are called osteophytes. When one part of the spine suffers, the load on the intact part of the spine increases. For example, when a disc herniates, compression of the root or spinal cord occurs. When hypermobility of a spinal segment occurs, the capsules of the facet joints thicken due to efforts to stabilize the segment, which can also lead to the formation of osteophytes. These osteophytes reduce the space of the intervertebral foramina and exert compression on the nerve roots.
Spondylolisthesis is a condition where one vertebra slips towards another. Spondylolisthesis occurs due to degenerative changes or trauma or is extremely rarely congenital. Disturbed biomechanics of the spine due to listhesis can lead to pressure from the slipped vertebra and along with it the disc, to pressure on the spinal cord or roots.
Age-related degenerative changes in the spine are the most common causes of spinal stenosis. Stenosis is often caused by two forms of arthritis (osteoarthritis and rheumatoid arthritis).
Osteoarthritis is the most common form of arthritis and typically occurs in middle-aged and older adults. It is a chronic, degenerative process that can involve many joints of the body. With this disease, wear and thinning of the surface layer of the cartilage tissue of the joints occurs and often there is excessive bone growth, osteophytes and a decrease in the functionality of the joints. When the facet joints and discs are involved in the process, a condition occurs that is called spondylosis. Spondylosis can be accompanied by disc degeneration with bone growths, which can lead to both a narrowing of the spinal canal and intervertebral foramina.
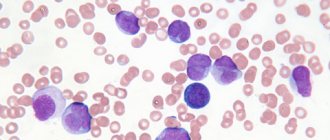
Rheumatoid arthritis usually affects people earlier in life than osteoarthritis and is associated with inflammation and thickening of the soft tissue (synovium) of the joints. And although rheumatoid arthritis is not so often the cause of spinal stenosis, damage to the ligaments of the bones of the joints can be quite serious and begins with synovitis. Segments with excessive mobility (for example, the cervical spine) are primarily affected by rheumatoid arthritis. Other conditions not associated with degenerative changes in the body include the following: Spinal tumors - overgrowth of tissue that can put direct pressure on the spinal cord or narrow the spinal canal. In addition, the growth of tumor tissue can lead to bone resorption or bone fragmentation.
Injuries and vertebral fractures can cause a narrowing of the canal; in addition, with complicated fractures, there may be an impact of bone fragments on the spinal cord or roots.
Paget's disease is a chronic bone disease characterized by abnormal growth of bone tissue that becomes thick and brittle (which increases the risk of fractures). The result is joint pain and arthritis. The disease can develop in any part of the body, but most often in the spine. Structural changes in the bone tissue of the spine can lead to a narrowing of the spinal canal and cause severe neurological symptoms.
Fluorosis is excessive levels of fluoride in the body. May occur due to inhalation of industrial gases and dust, ingestion of food containing high levels of fluoride, or accidental ingestion of food containing high levels of fluoride insecticides. Excess fluoride can lead to hardening of ligaments and/or softening of bones and degenerative changes leading to spinal stenosis.
Ossification of the posterior longitudinal ligament occurs when calcifications accumulate in the ligament, which runs along the entire spine. These calcium deposits actually convert ligamentous tissue into bone. And these calcium deposits can put pressure on the nerves in the spinal canal.
Diagnosis of stenosis
You should not guess about the disease based on the symptoms. Diagnosis of spinal canal stenosis is only possible using MRI results. The quality of the images must be at least 1.5 Tesla so that the doctor can accurately determine the specifics of the degenerative change, its location, and then prescribe effective treatment. The patient is also prescribed a survey spondylography with functional tests, which allows one to determine the mobility of the cervical, thoracic or lumbar segment. If there is a possibility of facet syndrome, CT and selective blockade of intervertebral joints may be additionally prescribed. If there are indications for spinal surgery or interventional pain treatment, diagnosis and treatment tactics are prescribed individually, depending on the clinical picture.
Risk factors
Many patients diagnosed with spinal stenosis are over 50 years of age. However, against the background of degenerative changes in the tissues of the spine, the disease can develop at a younger age, so do not forget about other risk factors.
The appearance of a narrowing in the spinal canal can be caused by injuries, congenital deformation of the spinal column in the form of scoliosis and genetic diseases that affect the formation of bone and muscle tissue throughout the body as a whole. Thanks to imaging methods, it is possible to determine exactly what triggered the onset of the disease.
Surgery for spinal stenosis
Doctors at the Pirogov Clinic treat degenerative stenoses both conservatively and surgically. All spine surgeries are performed using the latest endoscopic or microsurgical technology, as well as X-ray or radiofrequency equipment.
In most cases, preference is given to endoscopic operations for spinal stenosis
. They allow you to avoid the installation of implants - with the exception of cervical stenosis and cases where spondylolisthesis and instability of the spinal segment are also observed. In addition, such operations are characterized by maximum controllability, minimal risks, and for patients, rapid recovery after endoscopic surgery for spinal stenosis is tolerated most comfortably. The pain in the legs goes away immediately after the operation, and hospitalization in the clinic is only 1 day.
Find out more about endoscopic spine surgeries.
Stenosis surgery performed using microsurgical method
, also refers to minimally traumatic interventions. It is advisable (and may even be the only solution) if, along with expansion of the spinal canal and decompression of the spinal roots, stabilization of the spinal segment is necessary. Such operations show good clinical results and, unlike traditional open spinal surgeries, allow the patient to recover quickly and avoid the risk of disability.
Unfortunately, sometimes it is impossible to do without the installation of metal structures and endoscopic surgery is impossible. A difficult case from the practice of neurosurgeon Mereja Amir Muratovich
. The patient developed stenosis complicated by spondylolisthesis due to displacement of the vertebrae, which caused acute compression of the roots of the spinal canal. To avoid destabilization of the L4-L5 spinal segment and avoid severe consequences in the future, it was decided to fix the segment with screws and install an interbody cage. The operation was performed with pinpoint precision—the pain and weakness in the patient’s legs disappeared immediately after the intervention. The case was difficult and exceptional, but thanks to the experience and skill of our specialists, the patient was able to recover within 1 day.
Find out more about microsurgical operations on the spine.
Risk and prognosis of surgical treatment
Any surgical intervention is associated with risk during general anesthesia and the risk is high in elderly patients. The risk of surgical intervention itself for spinal stenosis is possible damage to the dural membranes, infectious complications, and thrombus formation. The presence of concomitant somatic pathology is a factor influencing the possibility of surgical treatment. As a rule, the result of surgical treatment is a rapid regression of symptoms, due to the fact that the causes of pressure on the nerve structures are eliminated. But in some cases, symptoms may persist for a long time even after surgery. This usually happens in cases where in the preoperative period there was prolonged compression on the nerves or spinal cord and damage to the nerve structure itself occurred. Long-term results of surgical treatment depend on the degree of degenerative changes in the spine and the effectiveness of rehabilitation.
Recovery after surgery for stenosis
After surgical decompression of the nerve endings and spinal roots, the pain in the limbs goes away immediately. Associated neurological symptoms (numbness and weakness) may take a little longer to resolve, depending on how long the patient has endured the symptoms and how much the disease has progressed. For several hours after surgery, the patient can stand and walk around the room. For 1-2 days (depending on the chosen method of surgery for stenosis), the patient is under the supervision of a doctor and medical staff. The doctor can then send him home with recommendations for the recovery period. After a month, it is advisable to come for a follow-up examination with a neurosurgeon - the doctor is always in touch and guides his patients until the recovery is successfully completed. The patient may be indicated for correction of motor habits. As a rule, no further additional restoration measures are required.
Features of rehabilitation
Once surgery is completed, patients are allowed to get up on their feet the same day or the next morning. During the normal course of the recovery period, discharge from the hospital occurs after 3–4 days. Each patient receives detailed recommendations from the doctor, strict adherence to which is the key to obtaining the most pronounced effect from the operations performed.
All patients are recommended:
- during the entire rehabilitation period, do not lift anything heavier than 3 kg;
- it is important to avoid vibration, shock, sudden movements, turns, and monotonous movements;
- Serious physical activity is unacceptable;
- Light household work is allowed, but if you experience pain, weakness or other symptoms, you should consult your doctor;
- on the recommendation of a doctor, it is necessary to begin performing special exercises and then regularly engage in exercise therapy under the guidance of a rehabilitation specialist;
- 4 weeks after surgery you should start swimming.
On average, the recovery period is 6–8 weeks. Accurate implementation of all medical recommendations allows you to reduce it and speed up the patient’s return to their usual lifestyle.
Why is it worth having surgery for stenosis at the Pirogov Clinic?
The Pirogov Clinic has accumulated 20 years of experience in minimally invasive spine surgeries. The clinic is equipped with modern endoscopic technology, as well as radiofrequency equipment, which in the world practice of spinal neurosurgery is the “gold standard” for the treatment of degenerative diseases of the musculoskeletal system. The operations are performed by a candidate of medical sciences. Sciences, leading neurosurgeon in St. Petersburg and leader of positive reviews from patients on independent platforms (for example, Napopravku.ru). In addition, we can offer our patients:
- Free remote consultation with a neurosurgeon (second opinion) on your disease;
- Availability of all highly specialized medical specialists in one place, as well as our own diagnostic laboratory;
- Service under VHI policies;
- Affordable prices, as well as assistance in obtaining a loan for treatment.
If you have any questions, leave a request for a call back through our website or call (812) 320-70-00 - we are always happy to help you!
Make an appointment