Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
Heart rhythm disorders (arrhythmias) are conditions in which the heart beats irregularly, too fast, or too slow. With frequent heart contractions - above 100 beats per minute in adults, this condition is called tachycardia, with rare - less than 60 beats per minute, it is called bradycardia. Some types of arrhythmia have no symptoms. If the arrhythmia is symptomatic, then the main complaints are palpitations or a feeling of a pause between heartbeats. Sometimes patients may complain of dizziness, fainting, shortness of breath or chest pain. Most types of arrhythmia are not a serious threat to the patient, but complications such as stroke or heart failure can often occur, and sometimes the arrhythmia can lead to cardiac arrest.
The Innovative Vascular Center employs experienced cardiologists who will help determine exactly why cardiac arrhythmia occurs and prescribe the correct treatment. In addition to drug therapy, our clinic implants artificial pacemakers (pacemakers) of any configuration. Timely and correct treatment allows our patients to avoid many complications, which means prolonging life and improving its quality.
What it is
Arrhythmia is a violation of the regularity and sequence of heart contractions.
Everything that is not sinus rhythm is called this term and includes various pathologies of impulse formation and its conduction. But few ordinary people know this, and it is believed that if a patient told the doctor: “I have an arrhythmia!”, then he understood everything and would immediately solve the problem by prescribing one specific medicine. Alas, everything is not so simple.
There is more than one classification of arrhythmias, but since my task is to introduce readers to the diversity and help them understand it themselves, and not to give a lecture to cardiologists, I will divide them into 2 groups:
- violation of impulse formation - here we include extrasystoles and tachycardias;
- pathology of the same signal - blockade and bradyarrhythmia.
How does normal heart contraction occur? Normally, the sinus node dominates - a power plant that generates impulses and transmits them further through the internodal pathways to the atrioventricular node, from which the signal goes along the His bundle, to its right and left branches, to the Purkinje fibers and to the ventricular myocardium.
Diagnostics
It is possible to diagnose atrial fibrillation during a physical examination. Pathology is indicated by an orderly pulse, irregular heart sounds, and significant fluctuations in their volume. Having discovered these deviations, the doctor refers the patient for instrumental studies. In the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, diagnostics are carried out using:
- taking an ECG during an attack of arrhythmia;
- daily HM-ECG with recorded arrhythmia (ECG using the Holter method);
- data from electrophysiological studies of the heart;
- MRI or MSCT of the heart.
Causes of arrhythmias
There are three groups of reasons:
- cardiac - when there is cardiovascular pathology: coronary disease, hypertension, heart disease, myocarditis, pericarditis, cardiomyopathy, and so on;
- extracardiac – these include diseases of other organs and systems (chronic bronchitis, pathologies of the thyroid gland, gastrointestinal tract), taking medications (antiarrhythmics, sympathomimetics, antidepressants, diuretics, etc.) or toxic effects (smoking, alcohol, drugs), as well as electrolyte disturbances (hypo- or hyperkalemia, hypomagnesemia, etc.);
- idiopathic – when the cause of the arrhythmia could not be identified.
The mechanism of heart rhythm disturbances
The heart has the following abilities:
- automaticity - cardiomyocytes can spontaneously generate an impulse (due to this they are called “pacemakers”);
- excitability - cells perceive the signal and respond to it;
- conduction - the impulse can spread through the conduction system of the heart;
- contractility - the ability to contract in response to a stimulus.
Thus, the myocardium independently generates electrical currents that are conducted along the intracardiac pathways, excite the muscle and cause its contraction.
As noted earlier, arrhythmias arise due to a violation of impulse formation or conduction. The main mechanisms are presented in the figure below.
A change in automaticity in the sinus node is the cause of tachycardia, bradycardia (with weakness of the sinus node) and other arrhythmias. If the excitability of the underlying links of the conduction system, for example, the atrioventricular connection, increases, then it takes on the role of a pacemaker, and an ectopic accelerated rhythm occurs.
Trigger activity is the formation of impulses by cardiomyocytes, which normally do not have a pacemaker (signal-generating) function. This mechanism underlies extrasystoles and tachycardias as well as another, re-entry (in its case, the signal causes one contraction, but under certain conditions it can excite the myocardium repeatedly due to the circulation of current in a circle).
A blockade occurs when an impulse encounters tissue that is unable to respond to the signal, for example, a post-infarction scar that has taken the place of a damaged cardiac conduction system.
Signs and symptoms: what complaints do patients have?
The palette of clinical manifestations is varied and colorful: from normal health to loss of consciousness and arrhythmogenic shock.
Depending on the type of arrhythmia, psycho-emotional status and concomitant diseases, patients present the following complaints:
- heart sinking;
- heart beats against the chest;
- cardiopalmus;
- dizziness, darkening of the eyes;
- shortness of breath, feeling of lack of air;
- weakness, fatigue;
- loss of consciousness and so on.
These symptoms are accompanied by a feeling of fear and are not always specific. A similar picture of the disease is also described by somatically (physically) healthy people suffering from panic attacks, neuroses or phobias. In these situations, we are talking about psychosomatics, and work with a psychotherapist is required, and not treatment by a cardiologist.
Case study: arrhythmia in a woman
There was an interesting case in my practice: a middle-aged woman came in complaining of episodes of loss of consciousness. They occurred during physical activity (climbing stairs, riding a bicycle), which was accompanied by severe shortness of breath, and before falling, she felt a palpitation. Before contacting a cardiologist, the patient was examined by a neurologist, but no abnormalities were identified.
When conducting echocardiography of the heart, the following was visualized: secondary hypertrophic cardiomyopathy, which developed as a result of subvalvular aortic stenosis. Thickened left ventricular myocardium is a risk factor for the development of life-threatening tachycardias and sudden cardiac death. During 24-hour ECG monitoring, runs of ventricular arrhythmia of varying duration were recorded.
The patient was sent for surgical treatment - correction of the heart defect and ablation (cauterization) of the arrhythmia area.
Features in men
A special feature of arrhythmia in men is “holiday heart syndrome.” This is a condition in which, after short-term consumption of large doses of alcohol (usually during feasts), arrhythmia occurs. More often, atrial fibrillation (atrial fibrillation) or ventricular arrhythmias occur.
Clinically, this syndrome is manifested by a feeling of palpitations, a feeling of weakness, shortness of breath, and chest discomfort, which can lead to arrhythmogenic death. The mechanisms of alcohol’s effect on the heart include both direct toxic effects and increased activity of the sympathetic nervous system and electrolyte imbalance. In chronic alcoholism, cardiomyopathy develops, the main manifestations of which are heart failure and cardiac arrhythmias.
If you stop drinking alcohol in time, there is a chance to restore the pumping function of the heart, but scientists have not been able to find out where the limit is when it is not too late. The attitude towards drinking in our country is very frivolous; people believe that alcohol “cleanses blood vessels” and its consumption is associated with health benefits. Yes, systematically drinking people rarely have heart attacks - they die from sudden arrhythmias, before thrombosis occurs.
When do interruptions in the functioning of the heart of organic origin occur?
As for extrasystoles of organic origin, this is the result of pathological changes in the heart itself in the form of the following diseases:
- IHD, such as previous myocardial infarction
- myocardial dystrophy
- cardiosclerosis
- various channelopathies (long QT syndrome, Brugada syndrome)
- the presence of congenital additional pathways (for example, WPW syndrome)
- dilated cardiomyopathy
- atrial enlargement
- myocarditis
- acquired and/or congenital heart defects (for example, atrial septal defect or aortic valve stenosis)
- pericarditis and other heart diseases
The reason for this extrasystole is the presence of a focus, for example, scar tissue, which has an unfavorable prognostic value.
The causes of paroxysmal (episodic) heart rate accelerations are approximately the same. With all the components, supraventricular rhythm disturbances are safer, in contrast to ventricular ones.
Classification of arrhythmias
Since the article is general education, I will not overload you with scientific terms, pathophysiology and other characteristics, but in general terms I will explain into which main groups arrhythmias are divided.
According to their source (topographically), they are supraventricular (everything that arises above the atrioventricular node) and ventricular. Based on the rhythm frequency, tachycardia (with a heart rate of more than 90-100 per minute) and bradycardia (slowing the rhythm to 50-60 beats or less) are distinguished. Tachycardias, in turn, are divided into supraventricular and ventricular, paroxysmal and non-paroxysmal.
Bradycardia is based on a violation of impulse conduction - blockade, which can be sinoatrial, atrioventricular, interatrial and intraventricular. These are the most common arrhythmias, and such a classification gives an idea of how they should be treated.
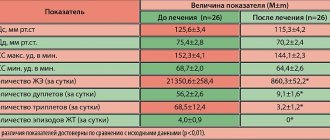
Table 1. Classification of arrhythmias.
By localization:
|
By heart rate:
|
Tachycardia:
|
Blockades:
|
I will separately highlight extrasystole - the “queen” among arrhythmias. The overwhelming number of patients come to me with exactly this problem. Extrasystoles are extraordinary contractions of the heart. They occur in everyone - both in healthy people and in people with various diseases - and often deprive patients of peace and sleep due to the painful sensations they experience during rhythm disturbances.
An interesting paradox is associated with this type of rhythm disturbance: in healthy individuals they do not pose a threat to life, despite the striking manifestations of symptoms. In people with serious organic diseases, extrasystoles can be asymptomatic and be an accidental finding on an electrocardiogram or daily ECG monitoring.
Forecast
Cardiac arrhythmias are dangerous because they can lead to sudden cardiac arrest due to complete blockade of conduction. In severe arrhythmia, there is a high risk of ventricular fibrillation, which can be fatal. Atrial fibrillation leads to the formation of blood clots in the atria and their transfer to other organs with the development of stroke and gangrene of the extremities. The probability of an unfavorable outcome in patients with arrhythmias depends on the form of rhythm disturbance and is more than 20% per year. You should not rely on folk remedies - arrhythmia is very dangerous and requires correction by a professional cardiologist.
Manifestations on the cardiogram
Let's consider the signs of arrhythmia on the electrocardiogram using the example of extrasystole, tachycardia and blockade of impulse conduction.
If a patient has an extrasystole, for example an atrial one, his ECG will look like this: against the background of a regular sinus rhythm, where there are equal intervals between the ventricular complexes, an extraordinary contraction appears, followed by a pause of varying duration depending on the type of extrasystole.
We will analyze tachycardia using two examples: paroxysmal AV nodal and ventricular. With the first type of arrhythmia, an episode of rhythm with a high frequency is recorded on the ECG, while it remains constant throughout the entire paroxysm. The complexes on the cardiogram are narrow and the P waves, characteristic of sinus rhythm, will not be visible.
With ventricular tachycardia, dilated deformed complexes are recorded, reminiscent of bundle branch blocks; heart rate is more than 120 beats per minute.
In the case of blockade development, for example, 1st degree AV block, on the ECG we see an extension of the PQ interval by more than 0.2 seconds, which reflects a disturbance in the conduction of impulses from the atria to the ventricles. With 2nd degree AV block Mobitz 2 there is a sudden loss of the complex, while the PQ interval is either prolonged or normal.
List of the best pills
The heart rate for a healthy person should be 60-80 per minute. With an increase or decrease in their number, arrhythmia develops. You can normalize your heartbeat with the help of medications.
The selection of medications necessary for treatment depends on the symptoms of the disease and whether the heart rate is increased or decreased.
The list of the best tablets for the treatment of arrhythmia includes:
- Drugs that restore heart rate, with an increased rhythm, based on the quinine series. Medicines from this series are toxic and pose a potential threat in case of overdose, so they are only available with a doctor's prescription. The drugs are available in the form of tablets and gelatin capsules. The action inside the body begins 10-15 minutes after administration. When the medicine is administered intravenously, the effect begins immediately.
- For ventricular arrhythmias, the drug Etatsizin is prescribed. It is available in the form of tablets and injection solutions. the use of Etacizin is contraindicated in patients with low blood pressure.
- A safer drug for lowering blood pressure and stabilizing heart rate are beta-blockers. The range of application of these drugs is very wide. It is prescribed for atrial fibrillation and sinus tachycardia. The drug is widely used to prevent the development of heart attacks and strokes.
- Means to slow down repolarization. The most popular drug in this series is Amiodarone, available in the form of tablets for the treatment of arrhythmia and solutions for injections. It is characterized by fast action. It is used as an emergency aid during attacks and as a medicine for cardiac arrhythmia in the elderly.
- Potassium and calcium channel blockers. The most effective drugs in this class are Verapamil and Diltiazem. They are used to quickly stop arrhythmic attacks. A significant advantage of the drugs in this series is their low cost.
- As an emergency aid for chest pain and slow pulse, it is effective to use a mixture of tincture of valerian, lily of the valley and belladonna. For increased heart rate, use drops of Valocordin or Corvalol, after dissolving 30-40 drops in a small amount of water.
ethnoscience
The list of drugs used to treat cardiac arrhythmia in folk medicine is impressive. At home, they use infusions and decoctions of medicinal plants, alcohol tinctures, and vitamin mixtures.
The most common remedy is rosehip decoction. 1 tbsp. a spoonful of fruit is poured into two glasses of boiling water and infused for 10-15 minutes and filtered. Drink ½ cup with 1 teaspoon of honey twice a day.
It is possible to combine rose hips with hawthorn. 2 tbsp. spoons of rose hips are poured into 500 ml. boiling water, leave for 60 minutes, add hawthorn to the infusion. Drink ½ glass on an empty stomach. This remedy is recommended for use for atrial fibrillation.
Melissa decoction effectively helps relieve nervousness and stress. To prepare 1 tbsp. pour a spoonful of lemon balm leaves into 500 ml of water, bring to a boil and leave for 30 minutes. Consume three times a day before meals. Attacks of cardiac arrhythmia are more easily tolerated if taken as a sedative.
An infusion of viburnum berries is effective in the fight. Pounded berries are poured with water at room temperature, left for 6-8 hours, filtered and consumed before meals three times a day for a month.
Often, for arrhythmia, a decoction of valerian root is used. 2 tbsp. spoons, pour 150 ml of water, boil over low heat for 20 minutes, leave for 30-40 minutes, consume before meals three times a day.
A widely used recipe for an alcohol tincture made from hawthorn berries. 15 grams of dry fruits are poured with 150 ml of vodka or diluted alcohol, infused in a dark place for 10-15 days. Take 10 drops, adding ½ glass of water.
A mixture of dried fruits and honey is an effective remedy for the general strengthening of the heart muscle.
To prepare, take raisins, dried apricots, nuts and prunes in equal proportions, mix with honey and lemon juice. Use the resulting product in the morning after meals, 2 tbsp. spoons. Use the mixture for 30 days.