Heart rate variability means its variability in response to physical, emotional stress and other external and internal factors. The closer it is to normal or slightly higher than average, the easier it is for the body to adapt to new conditions. High values occur in well-trained athletes who lead a healthy lifestyle, when a person receives sufficient loads and recovers well from them.
Low heart rate variability is typical for diseases: angina pectoris, myocardial infarction, diabetic polyneuropathy, changes in the heart muscle with high blood pressure (hypertrophic cardiomyopathy). A decrease in the indicator to critical values indicates the risk of sudden cardiac arrest.
An increase is a sign of the body’s readiness for stress and indicates the correctness of treatment for diseases. For the study, the rhythmography method is used (ECG for 5 minutes and loads or 24-hour monitoring, Apple Watch). Data assessment is carried out using mathematical analysis methods.
What is heart rate variability (HRV)
Pulse variability, or heart rate variability (HRV), is, in simple words, variety, that is, the acceleration and deceleration of contractions.
For example, a person's heart rate is 60 beats per minute. This means that one second passes between successive contractions. If there is variability, then one interval will be 0.8 seconds and the next 1.2 seconds. This is a simplified approach, but in reality both the pulse rate and the intervals between successive beats will change.
This is completely normal, because at rest the rhythm should become slower, but with physical and emotional stress it speeds up in order to improve the nutrition of internal organs and the brain. Heart rate variability is one of the adaptive reactions. Therefore, the faster the heart changes rhythm, the better a person is adapted to survive in a wide variety of environmental conditions.
For example, in well-trained and endurance athletes, the heart pumps slowly at rest, but during activity, a significant acceleration occurs very quickly. Likewise, after training, they need very little time to restore their original performance.
What does it mean if saved?
If heart rate variability is preserved, this means that the heart adequately responds to changes in the level of oxygen in the blood, an increase in the need for nutrients and energy.
Using an example, we can compare the normal reaction of a healthy, active young person and a heart patient. The first at rest will have an average heart rate of 65 beats per minute; at high load it will accelerate to 110-120. Then the heart muscle, brain, and skeletal muscles will receive a normal amount of oxygen to produce energy. At the end of the activity there is no need for a frequent rhythm; it will slow down and return to the original in 5-7 minutes.
With a slow pulse, the myocardium is well supplied with blood, and the strength of contractions increases. Heart rate variability in this case will be in the range of 65-115 beats.
A high resting heart rate is typical for heart patients. It is necessary in order to compensate for weak contractions of the myocardium and deliver as much oxygen as possible to the internal organs and the brain. Then the initial pulse will be 90-95 beats, and its increase to 110-115 may already be accompanied by heart pain and shortness of breath. Return to original values is slow. Patients feel palpitations for a long time after exercise. Heart rate variability is reduced, since the oscillation interval is only 90-115 beats per minute.
Why you need to know heart rate variability
Heart rate variability should be studied for the following purposes:
- assessment of the state of the autonomic nervous system and the balance between its two departments - sympathetic (conditionally stressful) and parasympathetic (responsible for recovery) in healthy people, with neurocirculatory dystonia, diabetes;
- check the body’s adaptive reserve, that is, the ability to work in extreme conditions (for example, a pilot);
- make a forecast of the risk of death in case of myocardial infarction, arrhythmia, heart failure, severe arterial hypertension;
- identify a risk group of patients who have the possibility of critical arrhythmia and need to have a pacemaker installed;
- select a drug or evaluate the effect of treating heart disease;
- determine the level of stress and stress resistance;
- identify the degree of maturity of the nervous system in children and adolescents.
Heart rate variability in sports is used to assess the initial state of the athlete, and then, during training, to determine the correct selection of loads and intervals between training for recovery.
Can it be simpler?
For those who are too lazy to understand all the variety of complex variability parameters, the applications offer a simple “verdict” - for this purpose, HRV indicators are translated into factors that are intuitive to everyone. In the case of Welltory, which I use, these are stress, energy and productivity (in the evening, the “productivity” parameter changes to “heaviness of the day”).
How are these factors calculated? It's quite simple.
There are ready-made formulas that researchers have derived mathematically by studying various HRV parameters, objective and subjective factors of human well-being. It turned out that stress level correlates with SDNN and LF, indicators associated with sympathy. Energy is calculated based on the work of the parasympathetic system, that is, the parameters RMSSD and HF: the worse the parasympathetic nervous system works, the more fatigue accumulates - and the energy becomes less. Finally, the productivity/severity of the day is correlated with the work of the prefrontal cortex: the more it is forced to interfere with the control of the heart, the less resource remains for productive work. And this can be determined using the VLF parameter.
How do all these ready-made formulas apply to the life of a particular person? Here's how: these formulas are “calibrated” for each application user. It is clear that we are all different - and it would be unrealistic to predict the well-being of any random person using the same formula. Therefore, the application uses a self-learning algorithm - and takes your measurements and feedback on your well-being (picture in the upper right corner) as initial data.
Heart rate variability: normal
Heart rate variability is assessed using several parameters; their normal values for people of different ages (men and women) are given in the table.
| Age | RR during the day, ms | RR at night, ms | SDNN during the day, ms | SDNN at night, ms |
| 20-39 | 754 | 883 | 59 | 67 |
| 40-59 | 832 | 963 | 51 | 56 |
| 60-80 | 832 | 937 | 45 | 49 |
RR is the duration of the interval between beats, and SDNN is the standard deviation of the intervals between heart beats, that is, the total variability of the rhythm. Measurements are taken in milliseconds (ms).
Other indicators are also used, their generally accepted designations:
- LF: low frequencies in the range of 0.04-0.15 Hz;
- HF: high frequencies in the range of 0.15-0.4 Hz;
- RMSSD: sequential interval difference deviation, shows HRV at elevated heart rate.
These are not the only measurements; there are also several methods for processing indicators: time domain (statistical and geometric), frequency domain, nonlinear and mathematical modeling.
Apple Watch metrics and meaning
For healthy people, it is enough to measure only two main indicators - RR and SDNN. By changing their values, you can monitor the state of the heart and nervous system using the Apple Watch (smart watch). Measurements are taken 2 times a day, so for accuracy you need to wear the bracelet without taking it off. You can get a result sufficient for processing in no less than 10 days.
The readings are usually lower in the evening, and higher in the morning before waking up. HRV is influenced by many external and internal factors. Therefore, it is also important to determine your optimal indicator. To do this, it is recommended to record the SDNN value every morning, and then evaluate your well-being at the end of the day. In this way you can find the value at which there is a good state. Then you should start from your own norm.
Reliability and validity
HRV has been shown to be a reliable and valid indicator of ANS function (10). In addition, in addition to the electrocardiogram (ECG), there are more practical methods for measuring HRV, such as sensor belts (3) and finger pulse sensors (4), which have also been shown to be reliable and valid measurements. In addition, some well-known brands, such as Polar, have released watches that accurately and reliably measure HRV (41, 42, 43). Other studies have also supported the use of certain technologies, such as the Omega Wave System (43) and even smartphone applications, such as the ithleteTM app (3).
When monitoring HRV in an athlete's training plan, instead of RMSSD, an interesting metric for measuring acute and chronic fluctuations in recovery status is gaining popularity - the coefficient of change. But this topic will not be discussed in more detail in this article.
Age/population
According to current research, HRV is a very reliable measure of ANS function in older adults (1, 44, 45, 46). Within-day and between-day HRV assessments have also shown high reliability in elite athletes (47). However, evidence from studies involving children (6–12 years) is inconsistent; in some, reliability is confirmed (48, 49), in others it is not (50, 51). Thus, research into the reliability and validity of HRV for children is needed.
Duration
It usually takes ten minutes to accurately measure HRV (five minutes of stabilization, then five minutes of recording), but with advances in technology and research, ultra-short measurements are now available. Ultrashort measurements of as little as one minute can provide reliable estimates of HRV (47, 52 – 54, 3).
Position
Reliable measurement with ultra-short HRV recording (one minute) is possible in the following positions:
- lying on your back (3, 53 – 55)
- sitting (47, 53)
- standing (53).
Reasons for upward or downward changes
The following causes a decrease in heart rate variability in healthy people:
- fatigue;
- stress overexertion;
- lack of sleep and rest;
- smoking;
- alcohol abuse;
- excessive intensity and frequent training;
- colds;
- dehydration.
In diseases, a decrease in HRV indicates their progression. Normally, variability increases after rest, normalization of the daily routine, recovery, massage sessions, and relaxation. In athletes, HRV increases with adequate training. For patients, an increase can be achieved by strictly following the doctor’s recommendations for treatment, correcting habits and lifestyle.
What is the danger
The danger is a decrease in HRV in patients with heart diseases - angina, heart attack, myocardial changes with high blood pressure. This sign is regarded as:
- deterioration of the heart muscle;
- disease progression;
- limit of compensatory capabilities (for example, the heart cannot withstand a high load during hypertension);
- risk of death.
In an athlete, a decrease in heart rate variability reflects overtraining and deterioration in physical fitness.
How does training affect HRV?
Without going into detail as it is beyond the scope of this article, we will briefly look at how performance manifests itself through HRV.
Increases in parasympathetic modulation (the ability of the PNS to modulate/control its functions, such as by lowering heart rate) and HRV are the result of classic physiological adaptations typically seen following exposure to endurance training. In short, endurance training increases the workload of the heart, which leads to an increase in left ventricular volume and wall thickness, as well as end-diastolic volume (due to increased plasma volume and decreased peripheral resistance), ultimately increasing stroke volume. Increased stroke volume means decreased heart rate to maintain similar cardiac output (at least at rest and during submaximal exercise). This results in a reduction in the metabolic load on the heart, increasing the efficiency of the time-pressure relationship. The decrease in resting heart rate is partly due to an increase in parasympathetic modulation, which is reflected through an increase in HRV (6).
Reduced heart rate variability: what does it mean, signs and symptoms
If rhythm variability is sharply reduced, this means that the heart muscle has exhausted its ability to compensate for high load or insufficient blood supply. The patient also has disturbances in the regulation of the rhythm of contractions on the part of the nervous and endocrine systems. The most studied signs of a drop in HRV are symptoms of angina pectoris, myocardial infarction, heart failure, and diabetic polyneuropathy.
Unstable angina
As HRV levels decrease in patients, the frequency and severity of attacks of chest pain increases. The ST segment drops on the ECG, reflecting deterioration of the coronary blood supply. With SDNN <40, the risk of sudden death within a month increases 8 times.
Myocardial infarction
A decrease in HRV reflects the depth and extent of the infarction and the severity of acute heart failure. The greater the increase in the tone of the sympathetic nervous system (increased heart rate), the higher the risk of a life-threatening form of arrhythmia - ventricular fibrillation with sudden cardiac arrest.
Heart failure
The higher the heart rate and the lower its variability, the more severe the circulatory failure. Patients experience shortness of breath and palpitations with lower levels of physical activity or even at rest. A drop in indicators reflects a decrease in the strength of myocardial contractions.
Diabetic polyneuropathy
With this complication of diabetes mellitus, a decrease in HRV makes it possible to detect deterioration in the innervation of the heart and other internal organs at a stage when there are no obvious symptoms. Typically, a slight change in indicators during an orthostatic test (transition to a standing position from a lying position). This means that the nervous system cannot provide an adequate change in heart rate during exercise.
Prospects for further research
With its growing reputation as an effective marker of recovery status and a likely marker of illness and injury, future research should be directed toward elucidating the true potential of HRV. This means that future research should explore:
- relationship between HRV and diseases
- relationship between HRV and trauma
- strength and power training based on HRV
- acute and chronic effects of HRV monitoring on performance
- reliability of HRV for children
- How accurately does HRV reflect recovery status in various athletic populations (endurance, strength/power, group sports athletes) and various other populations (men, women, geriatric and pediatric).
Indications for heart rate studies
Heart rate variability studies are needed when:
- attacks of chest pain;
- frequent fluctuations in pulse and blood pressure;
- signs of electrical instability of the myocardium - ventricular extrasystoles, complex arrhythmias with increased heart rate;
- the need to distinguish a functional rhythm disturbance (for example, in neurosis) from an organic one in heart disease;
- determining the stage of hypertension (from the second HRV decreases);
- assessing the risk of complications and poor prognosis in patients with cardiac pathology.
For healthy people, research is necessary when selecting a training regimen and professional selection for work with high stress on the body.
Mobile applications for HRV measurement
In practice, everyone who wants to take measurements at home has many options for this. Let's look at popular applications.
Elite HRV
An application for measuring heart rate variability, helps assess readiness for competitions.
The app displays a display of HRV, how breathing rates change, breathing guides, and how the body reacts to stress.
To activate and further use the application, a chest sensor is required. What measurements does the application show:
- Morning readiness. The measurement takes 2.5 minutes and must be measured daily in the morning. The indicator obtained in the morning is the most correct and shows the true state.
- Free metering. You can take measurements at any time of the day to assess the activity of the body.
This is what the final figure looks like:
- A green indicator indicates that today the body can withstand much more stress than at other times.
- Yellow represents the sympathetic system area and warns you that you are under more stress than usual. The recovery system is tense and has difficulty coping with the stress load.
- Red shows that you are stressed and in order not to overtrain, it is better to rest.
You need to pay attention to this and not overexert yourself during sports training. If you plan to exercise with the same intensity, then after physical activity there should be a rest for several days.
In order for the application to display the correct measurements, you need to enter data into it and you need to do this a few days before the measurement begins. Measurements need to be taken daily.
The app team has also released an educational HRV Course (in English only) for in-depth study of the topic.
Welltory
The application evaluates not only heart rate variability, but also determines how living standards affect physical condition.
The application displays the intervals between heart beats and shows the state of the body's autonomic system - energy reserves and stress level. Welltory is used in sports medicine and is available for smartphones.
You can find out your pulse, stress state and energy by placing your finger on the phone’s camera. The flash will record a video showing the heart rate and the time interval between contractions. Intervals reflect the work of the autonomic system.
It is recommended to take measurements daily. With regular measurements you will always know about the state of the body.
The application counts your heart rate and other data when you place your index finger on your smartphone's camera. Then, the app will display your stress level. Also, the application will help you correct your breathing technique. This will allow you to perform better in sports training.
The project team has also prepared many educational videos and materials on the topic of variability and stress management.
HRV4training (PRO)
The application measures heart rhythm, using not only the smartphone camera, but also Bluetooth chest sensors. Not only HRV is displayed, but also the oxygen saturation of the body. This is important for those who are involved in running sports, stress level, analysis of sports load on the body.
The application is suitable for professional teams, contains integration with sports applications and calendars, coach access and other advanced features.
Rules for rhythmography
Rhythmography requires strict adherence to the rules for ECG registration:
- time of day – from 9 am to 12 noon;
- temperature in the office – 20-22 degrees;
- complete silence;
- pre-ventilation for 30 minutes;
- semi-darkened room;
- absence of a health worker in the office during the recording period;
- lying or sitting position with support on the back of a chair;
- before starting recording, you need to give time to adapt (7-10 minutes);
- There should be no discomfort.
For women, days are chosen taking into account the menstrual cycle - usually 2-3 days after the end of bleeding and no later than 5 days before the next period.
Preparation for the procedure
The day before rhythmography, alcohol consumption, feasting, and night shifts are not recommended. You cannot take pills, drink coffee, play sports, or be nervous 12 hours before. Come for examination 2 hours after eating. In the office, you must turn off the phone and exclude all extraneous conversations.
Features of the study
After a short recording of the initial ECG (several cycles of 5 minutes), the doctor performs stress tests:
- respiratory - delay, acceleration, deceleration, long and short exhalation;
- change of body position - the patient is asked to stand up;
- squeezing the expander;
- vagal tests - massage near the carotid artery, eyeballs, cooling of the face, feet, hands;
- arithmetic exercises;
- taking medications that slow or speed up your heart rate.
Usually choose 2-4 types from those listed. When recording an ECG on a daily basis, the patient leads his usual lifestyle, but is required to record the time of sleep, meals, physical activity and its type, stress loads, and pain.
Decoding the results
After processing the results obtained, data is obtained on the functional state of the body; the decoding does not indicate the indicator of activity of regulatory systems (abbreviated PARS). It is considered a special program based on points. Taken into account:
- heart rate and variability;
- the ratio of sympathetic influences (stress, activity) and parasympathetic (rest, recovery);
- heart response to stress.
The points received are deciphered as follows:
- from 1 to 2 – the norm, the body reacts adequately to loads, the state of working (optimal) tension;
- from 3 to 4 – moderate tension of adaptive mechanisms, occurs during stress, transition to new working conditions, moving;
- 5 points – pronounced tension in the nervous and endocrine systems, but a healthy body can cope on its own, and in case of illness it is enough to reduce the effect of external factors;
- 6-7 points – overexertion, medicinal support of the body is required, complete exclusion of stress loads;
- 8-10 points – a critical failure of adaptation; a course of treatment will be required.
Introduction
In healthy individuals, the time interval between two adjacent heartbeats is constantly changing. This variability is commonly called heart rate variability (HRV) [1, 2, 21]. A change in heart rhythm is a universal response of the body to any impact. It is determined by the balance of sympathetic and parasympathetic influences [12]. This is what numerous HRV analysis methods are based on. It has been proven that heart rate is an indicator of abnormalities that occur in the autonomic nervous system, and changes in heart rate are the earliest prognostic sign of many diseases of the cardiovascular, nervous, respiratory, endocrine systems, etc. [22]. In clinical practice, HRV analysis is also used to select optimal doses of drugs, taking into account the autonomic tone of the body and to monitor the therapy [13, 17].
HRV analysis methods
To determine HRV, the results of ECG monitoring over a time period of at least 5 minutes are used. HRV is an additional parameter that can be assessed based on ECG monitoring data (in addition to identifying ST segment depression, determining the number of extrasystoles, etc.). In modern clinical practice, various methods of HRV analysis are used, which can be divided into two main groups: analysis in the time domain and analysis in the frequency domain.
Among the methods of analysis in the time domain, there are two main directions: statistical methods based on the assessment of various characteristics of RR intervals, and geometric methods, which consist in assessing the shape and parameters of the histogram of the distribution of RR intervals for the studied period of time [4, 13].
Methods of the second group (spectral) are used to identify characteristic time periods in the dynamics of changes in the duration of RR intervals. In addition, spectral analysis evaluates the contribution of certain periodic components to dynamic changes in the duration of RR intervals. They may be:
- high-frequency oscillations, mainly reflecting the influence of the parasympathetic division of the autonomic nervous system on the heart rhythm;
- low-frequency oscillations, mainly characterizing the effect of the sympathetic division of the autonomic nervous system on the heart rhythm;
- very low-frequency fluctuations, caused primarily by humoral influences on the heart rhythm.
In addition, using spectral analysis methods, it is possible to determine the balance of sympathetic and parasympathetic influences and the resulting activity of the autonomic influence on the heart rhythm.
It should be noted that the parameters of temporal and spectral analyzes of HRV during ECG monitoring are interrelated; in the specialized literature one can find their physiological interpretation [2].
Clinical significance of HRV analysis
HRV acquired independent clinical significance in the 1980s, when it was found that HRV is a very important and independent predictor of mortality in patients who have suffered a myocardial infarction. A number of factors contributed to the widespread use of various HRV analysis methods:
the creation of technical means that make it easy, accurate and non-invasive to measure RR intervals and blood pressure, as well as the widespread use of powerful personal computers;
development of physiological concepts that consider changes in HRV as a reflection of deviations in the sympathetic-parasympathetic balance of heart rate regulation.
Currently, a large number of studies have demonstrated a decrease in HRV in many pathological processes at the stage of their progression.
Cardiovascular pathology. Over the past two decades, much evidence has been obtained of the relationship between the state of autonomic regulation of the rhythmic activity of the heart and mortality from cardiovascular diseases. Based on an analysis of the ratio of high-frequency and low-frequency oscillations, it has been experimentally proven that in the presence of life-threatening arrhythmias, sympathetic tone prevails over parasympathetic activity [1, 19, 21]. In a population-based study of the North American Multicenter Study Group of Patients After Myocardial Infarction, a low standard deviation of 24-hour RR intervals was found to be strongly correlated with the risk of sudden death, and this correlation was more pronounced than between the risk of sudden death and indicators of left ventricular ejection fraction, number ventricular extrasystoles and episodes of paroxysmal tachycardia (according to the results of ECG monitoring), exercise tolerance [2]. It has been proven that a decrease in HRV is a predictor of death in chronic heart failure, reflecting changes in the activity of the autonomic nervous system in this pathology [10]. In our study, we found a decrease in a number of time parameters of HRV as the course of coronary heart disease worsened [15]. DPLiao et al. (1996) postulated that a decrease in parasympathetic activity (spectral analysis of HRV) is associated with the risk of developing malignant arterial hypertension [11].
Diabetic autonomic neuropathy, a complication of diabetes mellitus, is expressed in early and disseminated neuronal degeneration of small nerve fibers of both the sympathetic and parasympathetic parts of the autonomic nervous system, and from the moment of clinical manifestation is characterized by an expected mortality of about 50%. It has been shown that during the clinical manifestation of autonomic neuropathy, HRV sharply decreases: the number of adjacent RR intervals that differ by more than 50 ms decreases [20].
Pulmonary pathology. Changes in HRV have been identified in various pulmonary diseases, which affect not only the respiratory function, but also the cardiovascular system. For example, in the work of A.V. Sokolov (2000), the diagnosis of respiratory failure syndrome and the degree of its severity in patients with chronic bronchitis was studied [14]. It has been shown that the main manifestations of respiratory failure syndrome in patients with chronic bronchitis are not only the symptom complex of shortness of breath, but also a decrease in HRV. The work of KM Yum, SN Kim (1997) proved that with an increase in pressure in the pulmonary artery in patients with chronic cor pulmonale, the power of both high-frequency and low-frequency components of HRV decreases [31]. R.H. Zulkarneev (1997) studied the cardiorespiratory pattern (analysis of HRV and respiratory cycle variability) of patients with bronchial asthma. A decrease in total HRV, as well as its high-frequency and low-frequency components, was demonstrated as the severity of bronchial asthma increased, indicating a general decrease in the autonomic influence on the heart rhythm [9]. The works of JP Watson (1999) and A. Noda (1998) examined the relationship between autonomic dysfunction (based on HRV analysis) and the severity of arterial hypoxemia. A decrease in a number of HRV parameters was found with increasing arterial hypoxemia in patients with chronic obstructive bronchitis [27, 29].
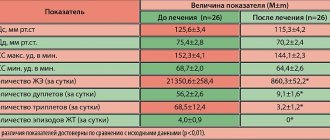
Effect of drugs on HRV
Based on ideas about the clinical significance of HRV, many studies have studied changes in HRV parameters under the influence of various drugs in order to assess the possibility of their use to correct the autonomic regulation of heart rhythm and improve the prognosis of the disease, as well as to improve the quality of life of patients. To date, it has not been possible to obtain drugs that selectively regulate HRV and do not affect other body functions, however, it has been found that many well-known drugs widely used in the clinic affect HRV, which is often considered as their side effect. In some cases, it is positive (increased HRV), in others it is negative (decreased HRV).
Beta adrenergic agonists. In the works of T. Jartti et al. (1997, 1998) demonstrated a decrease in HRV when exposed to salbutamol (Salmeterol, Salamol, Salgim, Saltos) [24, 25]. These authors, in particular, conducted a randomized, double-blind, placebo-controlled study of patients with bronchial asthma, which assessed pulmonary function, systolic blood pressure and spectral analysis of HRV data for 20 minutes before and after (2 hours) inhalation of salbutamol (50 mcg per day in two doses). As it turned out, salbutamol reduced overall HRV by increasing sympathetic influence with a significant improvement in external respiratory function [25]. On the other hand, in the work of M.R. Yakushina (1995) demonstrated that in patients with chronic obstructive bronchitis with moderate and severe bronchial obstruction, treatment with Saltos (6 mg 2 times a day for 10 days) led to an improvement in the state of the autonomic nervous system and a decrease in sympathetic influences [18]. Thus, the prescription of drugs from this group to patients with chronic obstructive diseases with concomitant cardiac pathology should be carried out with caution, preferably under the control of HRV analysis during daily ECG monitoring.
M-anticholinergics. In the dissertation work of A.B Shabunina (2000), it was shown that monotherapy with ipratropium bromide (Atrovent) in a daily dose of 120-180 mcg for 12 weeks leads to optimization of the autonomic regulation of heart rhythm in chronic obstructive bronchitis, reducing the severity of sympathicotonia in such patients [ 16]. This makes it possible to use Atrovent for chronic obstructive bronchitis with concomitant cardiac pathology.
Angiotensin-converting enzyme inhibitors. Many domestic and foreign studies have demonstrated an improvement in HRV parameters, and therefore an improvement in the prognosis regarding the risk of sudden death and the development of life-threatening arrhythmias in patients with diseases of the cardiovascular system when using angiotensin-converting enzyme inhibitors. Thus, in the work of I. Derad et al. (1996) showed an increase in parasympathetic tone and a decrease in sympathetic tone of the autonomic nervous system when using enalapril (Ednit, Enap, Enam, Enarenal, Vero-elanapril). This study also found that in patients with coronary artery disease, 6 hours after oral administration of fosinopril (Monopril) at a dose of 20 mg and elanapril (100 mg), there was a significant increase in parasympathetic activity, a decrease in the concentration of catecholamines and cortisol in the blood plasma [22]. The results of the study by K. Jansson et al. (1999) indicate that captopril (25 mg 2 times a day for 6 months) increases HRV in patients with idiopathic dilated cardiomyopathy, and this effect persists for at least 1 month after discontinuation of the drug [23]. In the work of A.V. Zavadkin and N.S. Stepanova (2000) assessed the effect of Ednit (5 mg per day for 12 weeks) on ventricular ectopic activity and HRV against the background of heart failure. After 12 weeks of therapy, daily HRV indicators improved and the number of significant and life-threatening ventricular extrasystoles significantly decreased [7].
Beta blockers. Drugs in this group change the spectrum of heart rhythm towards increasing its high-frequency component; the contribution of the mid-frequency and low-frequency components, on the contrary, decreases, which indicates the normalization of the autonomic regulation of the heart rhythm. In patients with coronary artery disease, beta blockers lead to a significant increase in HRV due to increased influence of the parasympathetic nervous system and prevent increased sympathetic influences in the early morning hours. A. Kardos et al. (1998) studied the effect of lipophilic (metoprolol) and hydrophilic (atenolol) beta-blockers on autonomic balance in 50 patients who had suffered a myocardial infarction. Atenolol (Catenol, Tenormin) at a dose of 50 mg/day and metoprolol (Betaloc, Vasocardin, Corvitol, Metocard) at a dose of 100 mg/day were used for 4 weeks. In this work, both at rest and during exercise (psychological stress, orthostatic test), heart rate and the balance of sympathetic and parasympathetic influences were lower in the group of patients receiving atenolol. Similar results obtained by L. Juje et al. [11], indicate a less pronounced effect of atenolol on the autonomic nervous system compared to metoprolol. B. Wennerblom et al. (1998) showed that metoprolol at a dose of 100 mg per day, reducing the tone of the sympathetic nervous system, improved the prognosis of the disease in patients with coronary artery disease with exertional angina (functional class II-III) [30]. I.S. Yavelov et al (1999) found that in patients with unstable angina, after 1 week of regular use of metoprolol and atenolol (at an average daily dose of 282 and 148 mg per day, respectively), there was a normalization of HRV and a relative increase in vagal activity, and an increase in HRV occurred only in patients with an average initial resting heart rate of more than 67 beats/min [17]. In a study by A. Mortara et al. (2000) noted an increase in the indicators of temporary analysis of HRV in patients with chronic heart failure with long-term exposure to the non-selective beta blocker carvedilol (Dilatrend) at a dose of 12.5 mg 2 times a day [26]. I.V. Demidova et al (2000) demonstrated the high activity of the new cardioselective beta-blocker bisoprolol (Concor), which significantly increased HRV parameters in patients with post-infarction heart failure (NYHA functional class III-IV) when prescribed for 16 weeks at a dose of 5 mg 1 once a day [5].
Antiarrhythmic drugs. Data on the effect of propafenone (Ritmonorm) on HRV are contradictory. According to V.M. Mikhailov [12], it, like beta blockers, enhances parasympathetic activity and, thereby, improves HRV, but its effect is weaker than that of metoprolol and other beta blockers. It has been noted that propafenone (but not amiodarone) reduces the temporal characteristics of HRV in patients with chronic ventricular arrhythmias [2]. It has also been demonstrated that it reduces HRV by reducing the ratio of its low-frequency and high-frequency characteristics [2]. P.V. Dmitryuk (1997) showed that, regardless of the state of the autonomic nervous system, this drug increases the tone of the sympathetic department and at the same time weakens the vagal effect on the heart [6]. Thus, propafenone may have multidirectional effects on HRV, and its use is probably undesirable in patients who have suffered a myocardial infarction.
Calcium antagonists. The effect of calcium antagonists on HRV is highly variable. Diltiazem (Aldizem, Diacordin, Cardil) reduces low-frequency components of the spectrum in patients with acute myocardial infarction (while improving the prognosis of the disease) to the same extent as beta blockers. Nifedipine (Adalat, Cordeflex, Cordafen, Cordipin, Corinfar, Nifedex) does not have a similar effect [10]. In the work of O.A. Goloshchapova et al. (2000) showed that nifedipine (using both a conventional treatment regimen and retard forms of the drug) reduces HRV in the majority of patients with arterial hypertension [3]. Thus, in patients with cardiovascular diseases, it is advisable to use calcium antagonists (diltiazem and its analogues, but not nifedipine) to improve HRV.
Estrogens. According to G. Rosano (1993), in healthy postmenopausal women, hormone replacement therapy with 17b-estradiol (Estradiol, Climar, Estrofem) at a dose of 1 mg per day for 4 months significantly increases HRV indicators, which indicates normalization of autonomic nervous function systems in relation to control over the cardiovascular system [28].
Conclusion
Based on the data on the effect of a number of pharmaceuticals on HRV, it seems advisable to use some of them to increase HRV in order to improve the prognosis of cardiovascular diseases as a result of correction of the autonomic regulation of heart rate. First of all, beta blockers and angiotensin-converting enzyme inhibitors should be considered promising in this regard.
Rate variability is sharply reduced: how to treat
If there is a sharp decrease in heart rate variability, you must:
- reduction of load (reduction of physical activity, elimination of anxiety, conflicts);
- refusal of stressful changes (for example, change in climate, work, diet, business trip, participation in competitions);
- sleep at least 8 hours at night, if necessary, rest during the day;
- transition to a healthy diet - vegetables, fruits growing in the area of residence, lean meat, fish, dairy products, a minimum of processed and canned food, no spicy, fatty foods, alcohol, strong tea, coffee;
- provide an opportunity for relaxation for the nervous system - breathing exercises, walks in nature, light massage sessions, aromatherapy, listening to calm music.
If there are heart diseases, the doctor reviews treatment regimens; they can be supplemented with drugs that improve metabolism in the myocardium (for example, Preductal, Mildronate).
Increased variability: what to do
With increased heart rate variability, the body is ready for stress, so this period is considered optimal for any active exercise. Athletes with high performance demonstrate success in competitions; you can plan a change in climatic conditions (for example, a trip to hot countries on vacation or an expedition to the north). Any complex projects at such a time are considered especially successful.
Pulse variability means its variability when changing external and internal environmental conditions. If it is normal, then the body is well adapted to stress, and if it is reduced, rest and recuperation are needed. Low levels in heart patients are dangerous due to critical cardiac dysfunction.