Sinus rhythm
Sinus node - This is a group of cells located in the right atrium that have the ability to produce impulses and transmit these impulses to other myocardial cells.
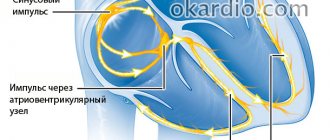
Normally, the impulse arises in the sinus node of the right atrium, covers both atria, then through the atrioventricular node, which is the center of second-order automaticity, the impulse is transmitted to the ventricles and covers them with excitation.
This is how the heart contracts: first the atria, and then the ventricles. If, after conducting an ECG, the doctor concluded “sinus, correct rhythm,” then this means that your heart contracts normally, there are no pathological abnormalities in the functioning of the conduction system. This means that the impulse that causes your heart to contract occurs where it is needed, namely in the sinus node of the right atrium.
ECG and sinus rhythm
Normal sinus rhythm
The simplest and most accessible method of determining heart rhythm is an ECG. This is a method that allows you to determine the frequency and regularity of heart contractions, assess the nature of the rhythm and its source, and diagnose acute or chronic myocardial damage. An ECG is mandatory during preventive examination and medical examination. Any doctor and medical worker with secondary medical education should be able to encrypt a cardiogram.
On the electrocardiogram there is a P wave, which is responsible for the work of the atria, and there is a complex of QRS waves, this complex shows the work of the ventricles. Since the atria normally contract first, then the ventricles, the P wave should always precede the QRS complex.
So, ECG signs of sinus rhythm:
- Constant shape of the P wave (duration 0.1 s, height 2-2.5 mm),
- Equal distance between teeth P-P or RR,
- The P wave always precedes the QRS complex,
- The distance from the P wave to the subsequent Q wave is the same and equal to 0.12-0.2 s,
- Heart rate from 60 to 90 beats per minute.
If these criteria are met on the ECG, this means that the heart rhythm is normal.
What does a patient need to know before an ECG?
Carrying out an ECG
In order for the electrocardiogram data to be as accurate as possible, there are certain rules that the patient must follow before conducting this study. Firstly, try not to be nervous, do not drink alcohol, coffee, strong tea, or smoke before the procedure, since the heart rate will increase, tachycardia will develop and the ECG data will be incorrect. There is no need to overeat and do physical labor. If you follow all the above rules, then recording an ECG will allow you to most accurately diagnose the work of your heart and determine its rhythm and frequency of contractions.
Implantation of an artificial pacemaker (stimulator)
Normally, the heart produces electrical impulses that cause the heart to beat rhythmically.
But, there are various pathologies that lead to rhythm disturbances. Various types of arrhythmias lead to disruption of blood flow through the chambers of the heart and blood vessels of the body, resulting in dizziness, weakness, shortness of breath, progression of heart failure, and loss of consciousness. Of particular danger are bradycardias, blockades, and pacemaker dysfunction, since the absence of impulses will cause the absence of contractions of the heart chambers, and possibly its complete stop. The only reliable method of treatment is surgery - implantation of an electrical pacemaker, which will always maintain rhythmic contractions of the heart and ensure vital functions.
Types of pacemakers
A pacemaker is a special device that, using electrical impulses, sets the heart to the correct rhythm and thereby saves you from life-threatening conditions. The pacemaker consists of 2 parts: a metal case that includes a special chip, a battery and electrodes. Average service life is from 7 to 10 years.
1. Single-chamber pacemaker - equipped with one electrode installed in one chamber of the heart (atrium or ventricle). The disadvantage of this type of device is the stimulation of only “one chamber” without taking into account the own activity and contractions of the other chamber. If the contraction of the atria and the ventricle coincides, the normal flow of blood in the heart is disrupted: blood is refluxed into the atrium and blood-bearing vessels.
2. Double-chamber: installed in the atrium and ventricle of the heart, which ensures synchronous contraction of the ventricles and atria, stimulation becomes physiological, significantly increasing the patient’s functional capabilities. Unlike single-chamber stimulators, in this case, coordinated contractions occur - the atria first and only then the ventricles, ensuring proper blood flow and complete filling of the blood vessels, as in a healthy heart.
A dual-chamber stimulator differs from a single-chamber stimulator in that a single-chamber stimulator has an electrode only in the ventricle and stimulates only the ventricle of the heart or only in the atrium, stimulating only the atrium (only one chamber of the heart, which is why it is called single-chamber). If the electrode stimulates the ventricle, the atria contract independently. This is bad because sometimes the contractions of the atria and ventricles can coincide, then the blood from the atria will not go into the ventricle, as it should, but back into the veins. This will lead to shortness of breath and weakness. And in a dual-chamber stimulator, one electrode is in the atrium, the other in the ventricle (that is, in two chambers of the heart) and coordinates heart contractions so that the ventricles contract after the atria, as befits a healthy heart. Accordingly, dual-chamber stimulation is more physiological.
3. Three-chamber: contains a device for the treatment of heart failure, installed on the right atrium and both ventricles.
For a certain type of heart rhythm disorder, a specific type of pacemaker is indicated.
Indications for surgery:
1. Acquired atrioventricular block of the third degree in adults.
2. Sustained atrioventricular blockade of the second degree or atrioventricular blockade of the third degree of the heart, which occurred after myocardial infarction with blockade in the His-Purkinje system.
3. Bi- and trifascicular blockade
4. Sick sinus syndrome
5. Carotid sinus hypersensitivity syndrome and neurovascular syndromes
Contraindications
For those who need a pacemaker, there are practically no contraindications; the only contraindication to installing a pacemaker may be the unreasonableness of the operation.
- first degree atrioventricular block without clinical manifestations;
- proximal atrioventricular block of the first type of the second degree, without clinical manifestations;
- atrioventricular block that can regress (for example, caused by medication).
List of examinations before surgery.
- General blood test, general urine test, valid for 10 days.
- Blood type and Rh factor are valid for 1 month.
- Coagulogram (in case of taking warfarin for arrhythmia - discontinuation of warfarin 7 days before hospitalization, INR acceptable for hospitalization is 1.5), valid for 10 days.
- Biochemical blood test, valid for 10 days.
- Blood test for HIV, HCV, Hbs, valid for 1 month.
- Copy of HM-ECG, valid for 2 months.
- Copy of ECHO-CG, valid for 1 month.
- Fluorography, valid for 1 year.
- Copy of passport, policy, SNILS.
Operation.
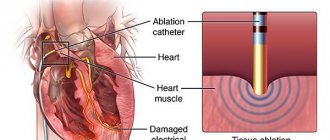
The operation is low-traumatic and relatively safe. It takes from 40 minutes to 2 hours (depending on the type of stimulator). The operation is performed under local anesthesia: a solution of novocaine or lidocaine is injected into the subclavian area (usually on the left). An incision up to 5 cm long is made below the collarbone. A pocket (bed) is formed under the skin in which the stimulator body will be located. Through the subclavian vein, the electrode is inserted into the cavity of the right atrium or ventricle with a single-chamber stimulator, and into the cavity of the right atrium and ventricle with a two-chamber stimulator. There are several types of electrodes:
1. with passive fixation, which independently cling to the heart
2. with active fixation, which are fixed in the heart using a “screw”
Then, the surgeon finds the most sensitive place to stimulate. The electrodes are fixed and connected to the stimulator body. The wound is sutured layer by layer.
In the postoperative period, antibiotic and anti-inflammatory therapy is carried out to prevent purulent complications and dressings. The length of stay in the hospital is 3-4 days.
Possible complications
As with any surgical intervention, there are possible complications after pacemaker implantation (up to 1%). These are bleeding, pneumothorax, cardiac perforation, risk of suppuration and device malfunction, electrode displacement, insulation failure, “pacemaker” syndrome, and infectious complications.
Life after ECS.
After surgery, you can live a full and happy life. No restrictions on:
- in eating,
– driving a vehicle,
– playing sports (it is necessary to avoid exercises that pose a threat of injury to the area of the implanted stimulator: contact sports, shooting with a gun, rifles, scuba diving,
– traveling (you must have a stimulant passport with you);
It is necessary to avoid exposure to high power equipment, “magnetic frames”. Carry your cell phone in the opposite chest pocket, and hold the phone on the opposite side when talking. A cardiologist regularly examines a patient with a pacemaker to evaluate pacemaker function, adjust pacing programs, and assess battery charge. Such examinations should not be neglected, since if the pacemaker stops, the heart may also stop.
After the operation, doctors monitor and control the operation of your stimulator, regularly schedule examinations for you to check the operation of the stimulator, the battery charge, and view the chronology of events that are recorded in the ECS memory to correct therapy, because the work of your heart depends on the correctly selected program.
In our Heart Clinic, pacemakers are implanted free of charge for patients under compulsory medical insurance.
Heart rate in children
Heartbeat in children
The heartbeat of newborns and toddlers is much faster than that of an adult. If you place your palm on the chest of a small child, you can hear how fast and loud the tiny heart beats. The younger the child, the more often his heart beats. For example, the norm for a newborn baby is a heart rate of up to 140 beats per minute, and when feeding or crying, it can reach 180 beats per minute.
This is explained by the fact that babies have a more intense metabolism and the fact that the heart is less susceptible to the influence of the vagus nerve, which slows down the heartbeat. By two years of age, the average heart rate is 120-125 per minute, by six - 100-105, and by ten to twelve years the child’s heart rate will correspond to that of an adult.
These physiological features characteristic of childhood should be taken into account by the parent, and not panic if, when deciphering the cardiogram, the doctor writes a three-digit number, determining the heart rate of your child. Perhaps a rapid heartbeat is normal for his age. And if the intervals between heart contractions are the same, the P wave accompanies each set of ventricular contractions - this means sinus rhythm, and in this case there is no cause for concern.
Organic arrhythmias
Organic arrhythmias include:
- Arrhythmias arising from coronary heart disease (myocardial infarction, angina). Arrhythmia is caused by damage to the heart muscle. It makes it difficult for electrical impulses to propagate correctly through the conduction system of the heart. Sometimes damage can even affect the cells of the main pacemaker - the sinus node. In place of the dead cells, a scar of connective tissue (cardiosclerosis) is formed, which is not able to perform the functions of a healthy myocardium. This, in turn, leads to the formation of arrhythmogenic foci and the appearance of rhythm and conduction disturbances.
- Rhythm disturbances that occur after an inflammatory process in the heart muscle - myocarditis. As a consequence, after suffering from inflammation, the myocardium is also replaced by connective tissue (cardiosclerosis).
- Arrhythmias observed in cardiomyopathies. For an unknown reason, myocardial cells are damaged, the pumping function of the heart is disrupted, and heart failure develops. In addition, various rhythm disturbances are very often associated.
- Arrhythmias that appear with various heart defects (congenital and acquired during life). It should be noted that there are congenital primary diseases of the conduction system of the heart itself.