The most acute period
Typical cases of myocardial infarction are characterized by extremely intense pain with pain localized in the chest and radiating to the left shoulder, neck, teeth, ear, collarbone, lower jaw, and interscapular area. The nature of the pain can be squeezing, bursting, burning, pressing, sharp (“dagger-like”). The larger the area of myocardial damage, the more severe the pain.
A painful attack occurs in waves (either intensifying or weakening), lasting from 30 minutes to several hours, and sometimes even a day, and is not relieved by repeated administration of nitroglycerin. The pain is associated with severe weakness, agitation, a feeling of fear, and shortness of breath.
How to help with chickenpox?
There is currently no cure for chickenpox. Usually the disease goes away on its own, and therapy is limited to smearing the rash with aniline dyes with bactericidal properties. A solution of brilliant green (“zelenka”) is usually used. You can take an antipyretic to relieve your general condition.
To relieve itching use:
- solution of iodine tincture (2-3%);
- solution of potassium permanganate (1:5000);
- hydrogen peroxide (3%);
- glycerol.
In some cases, antihistamines can help relieve itching. But you should not take them uncontrollably: it is better to call a doctor at home and determine acceptable medications. Showering is allowed, but without a washcloth to avoid damaging the bubbles. The same applies to the use of towels - after water procedures, you need to carefully pat your body dry with a cloth.
Acute period
In the acute period of myocardial infarction, pain syndrome usually disappears. The persistence of pain is caused by a pronounced degree of ischemia of the peri-infarction zone or the addition of pericarditis.
As a result of the processes of necrosis, myomalacia and perifocal inflammation, fever develops (from 3-5 to 10 or more days). The duration and height of the temperature rise during fever depend on the area of necrosis. Arterial hypotension and signs of heart failure persist and increase.
Publications in the media
Atypical mycobacterial infection is a complex of granulomatous lesions caused by mycobacteria that differ from the classical pathogens - the causative agents of tuberculosis and leprosy.
Etiology. Pathogens are acid-fast bacteria Mycobacterium ulcerans, M. marinum (M. balnei), M. kansasii, M. avium-intracellulare, M. xenopi, M. scrofulaceum.
Epidemiology. Most pathogens are widely distributed in the environment; some live in water and coastal zones, causing diseases in fish, others (for example, Mycobacterium avium-intracellulare) - in birds. Most often, infection occurs through inhalation of mycobacteria, consumption of contaminated products, and penetration of the pathogen through microtraumas of the skin and mucous membranes.
Pathogenesis. Invaded mycobacteria are phagocytosed by macrophages and transported to regional lymph nodes; phagocytic reactions are incomplete, and the pathogen persists in the cytoplasm of macrophages. The inflammatory reaction is insignificant, but a primary affect develops at the site of penetration. Over time, along the regional lymphatic pathways and nodes, a primary complex is formed, characterized by the development of granulomas. Microscopy of biopsy specimens reveals foci of non-caseating necrosis containing acid-fast bacteria.
Clinical picture
• Tuberculosis-like lesions. The pathological process involves the lungs, kidneys, skin and osteoarticular system. Often complicate the course of emphysematous processes. In 40–50% of patients with immunodeficiency conditions, generalized lesions are caused.
• Lymphadenitis. Clinically, they are more often manifested by lesions of the cervical lymph nodes (the so-called scrofula); the latter are painless, can ulcerate or drain outward; systemic manifestations are weak or often absent.
• Skin lesions. Infection of wounds of the extremities received when hitting the wall of the pool or any object on the bottom and banks of the reservoir is considered typical. More often, the formation of an ulcerating granuloma is observed, which is spontaneously limited within a few weeks; in more rare cases, a chronic infection forms.
• Less commonly observed are chronic pulmonary lesions in middle-aged people, which have now been reported everywhere. Possible bursitis of the elbow joint with repeated injuries and skin lesions, cervical lymphadenitis and carpal tunnel syndrome in people with immunodeficiencies (most often after therapy with hormonal drugs).
Research methods • Isolation and identification of the pathogen by growth rate, formation of pigments (in the light or in the dark) and pathogenicity for laboratory animals • Antibodies to Mycobacterium kansasii cross-react with Ag from Mycobacterium tuberculosis and a positive Mantoux test is noted in infected individuals.
Differential diagnosis • Leprosy • Tuberculosis • Borreliosis • Plague.
Treatment • For pulmonary lesions •• A combination of isoniazid 600 mg, rifampicin 300 mg, streptomycin 1 g and ethambutol 15–25 mg/kg 1 time per day is recommended •• For M. marinum lesions - minocycline 100 mg every 12 hours for 6 –8 weeks •• For lesions of M. kansasii and M. xenopi, standard anti-tuberculosis therapy is effective with mandatory administration of rifampicin •• Surgery is recommended for localized lesions in young patients without pathology of other organs and systems • For lymphadenitis - in children from 1 to 5 years, surgical treatment is indicated • For skin lesions caused by M. marinum - tetracycline (1-2 g/day) and a combination of rifampicin and ethambutol for 3-6 months • For infections caused by wounds or foreign bodies •• Surgical debridement and removal of a foreign body •• Drug therapy: doxycycline (200–400 mg/day), cefoxitin (200 mg/kg/day), amikacin (10–15 mg/day) for 3–6 months • For disseminated lesions - a combination of antituberculosis drugs drugs (as for pulmonary lesions) only reduces bacteremia and temporarily relieves symptoms.
Course and prognosis. The course is progressive. More than 20% of patients experience relapses of the disease within 5 years.
ICD-10. A31 Infections caused by other mycobacteria
Atypical forms of myocardial infarction
Sometimes there is an atypical course of myocardial infarction with localization of pain in atypical places (in the throat, fingers of the left hand, in the area of the left scapula or cervicothoracic spine, in the epigastrium, in the lower jaw) or painless forms, the leading symptoms of which may be cough and severe suffocation, collapse, edema, arrhythmias, dizziness and confusion.
Atypical forms of myocardial infarction are more common in elderly patients with severe signs of cardiosclerosis, circulatory failure, and secondary myocardial infarction.
However, only the most acute period usually proceeds atypically; further development of myocardial infarction becomes typical.
The erased course of myocardial infarction is painless and is accidentally detected on an ECG.
How to recognize chickenpox?
To get sick, two conditions are enough: to be near someone with chickenpox and not have a history of it. Everyone gets infected with it, regardless of age and immunity strength. Nothing can be done during the incubation period. All we have to do is wait for the first signs:
- temperature rise to 38-39 degrees;
- general malaise;
- decreased appetite;
- the appearance of a characteristic rash.
At first, the rash is rare and looks like spots or pimples. Under no circumstances should you squeeze them out: the scar will be very deep. The volume of the rash gradually increases, covering all parts of the body.
In the early stages, chickenpox can be mistaken for an allergic reaction. But contact dermatitis rarely spreads throughout the body and never develops into blisters.
In this case, the person feels severe itching. Scratching chickenpox is also not advisable. This will not bring relief, but there is a risk of getting a lot of scars on the skin or causing a secondary infection.
Abdominal type of infarction
When cardiomyocytes are damaged as a result of ischemia in the posterior-inferior region of the heart, the abdominal or gastralgic form develops. According to statistics, it occurs in 2% of patients who are admitted to the cardiology department with myocardial infarction. Most often, this option is observed with transmural necrosis.
If a person has previously had problems with the digestive system (pancreatitis, cholecystitis, hepatitis, gastritis), then he attributes all the signs to these diseases and simply swallows the usual pills. Or goes for a consultation with a therapist or gastroenterologist.
The abdominal variant manifests itself in the form of the following symptoms:
- dyspepsia (nausea, vomiting, diarrhea);
- acute pain in the upper abdomen, often on the right or in the epigastrium, with irradiation into the chest, between the shoulder blades, and back;
- increased blood pressure;
- increased heart rate;
- bloating and intestinal paresis.
The main reason for these manifestations is the close location of the back of the heart to the diaphragm. Therefore, pain occurs in the abdominal area. After some time, it gradually moves into the chest, and the person’s blood pressure drops sharply. And most often, unfortunately, I have to meet with the patient at this stage.
To identify the abdominal form of a heart attack, I pay attention to the following:
- In case of severe pain, any person takes a forced position, in which it becomes a little easier for him. In case of pathology of the abdominal organs, he lies on his side or on his back with his knees bent and brought to the stomach. The condition improves if you take a sitting position with your legs down or lie with a high headboard.
- When you start to find out your medical history, earlier signs of ischemic heart disease are revealed (pain behind the sternum, which develops after physical or psycho-emotional stress and is relieved by Nitroglycerone). If you have a history of acute abdomen—unpleasant sensations after breaking your diet—a regular painkiller or antispasmodic will help.
- An external examination reveals signs of cyanosis of the nasolabial triangle; there is a noticeable expression of anxiety on the face, as the patient experiences fear of death. The tongue is not affected by cardiac pathology.
- In peritonitis and infarction, there is a similarity in the slowing of contraction frequency. But in the first case it happens more slowly. If the problem is extensive damage to the heart muscle, then a rhythm disturbance and a sharp decrease in pressure are simultaneously recorded.
- Palpation and bimanual examination of the abdomen with cardiomyocyte necrosis cannot determine a clear localization of the problem. Continuing palpation usually leads to relief of the unpleasant sensation. If the disorder occurs in the abdominal cavity, then most often it is possible to feel the area of the causative organ, and the pain increases significantly.
Epidemiology
Genital herpes, being a special case of herpetic infection, is one of the most common sexually transmitted diseases, and differs from other diseases of this group in the lifelong carriage of the pathogen in the human body, which determines the high percentage of formation of recurrent forms of the disease.
Transmission routes
Transmission usually occurs through close contact with a sick person or a virus carrier. The virus penetrates through the mucous membranes of the genital organs, urethra, rectum or microcracks in the skin.
In couples where one partner is infected, the probability of infection of the second partner within a year is 10%. In most cases, infection occurs when the infected partner has not had a clinically significant recurrence of genital herpes. Asymptomatic and unrecognized forms of infection play an important role in the spread of the virus. The virus can be excreted in sperm; cases of infection of women during artificial insemination have been described. Speaking about the routes of transmission of the virus, it is necessary to note the important epidemiological significance of oral-genital contacts, which are associated with an increase in the frequency of isolation of herpes type 1 from the genitourinary system.
Who gets sick more often?
Among college students, antibodies to the herpes virus type II are detected in 4% of those examined, among university students - in 9%, among representatives of the middle strata of society - in 25%; among patients in dermatovenerological clinics with heterosexual orientation – 26%; among homosexuals and lesbians – 46%, among prostitutes – 70–80%. Antibodies to genital herpes are more often detected in representatives of the Negroid race than in whites. Women are infected more often than men, with the same number of sexual partners during their lifetime. In developed countries, the virus affects 10–20% of the adult population.
Numerous studies on the general population have shown that the incidence rate increases with age: isolated cases are detected in a group of patients aged 0–14 years; the highest incidence is recorded in the age group 20–29 years; the second peak incidence occurs at 35–40 years of age.
The main risk factors for developing the virus are a large number of sexual partners throughout life, early onset of sexual activity, homosexuality in men, belonging to the black race, female gender and a history of sexually transmitted infections.
Mandatory registration of genital herpes was introduced in the Russian Federation in 1993. During the period 1993–99, the incidence of this virus in Russia increased from 8.5 cases to 16.3 per 100 thousand population. The incidence in Moscow increased from 11.0 to 74.8 cases per 100 thousand population and almost reached the level of European countries.
Clinical features of herpetic infection in women
Herpes of the urethra and bladder
Herpetic urethritis in women is subjectively manifested by pain and cramping at the beginning of urination, and a frequent urge to urinate. With herpetic cystitis, hematuria, pain at the end of urination, blood in the urine, and pain in the bladder area appear.
Herpetic cystitis
In a woman, the first and only sign of HSV infection may be in the genitourinary tract. It often occurs in the first 1-3 months after the start of sexual activity or a change of sexual partner.
Herpes of the anal area and rectum
The lesion in the anal area usually represents a recurrent fissure, which is often a reason for diagnostic errors. Such patients with an erroneous diagnosis of “anal fissure” end up with surgeons. The itchy form of herpes anus and herpetic lesions of hemorrhoids are also difficult to diagnose.
The list of diseases etiologically associated with HSV is constantly growing. According to the literature, in 3.6% of women suffering from treatment-resistant colpitis and cervical leukoplakia, HSV is one of the etiological factors of the disease. A new form of latent intrauterine HSV-II infection with localization of the pathological process in the glandular epithelium of the endometrium is described. It has been proven that HSV can cause the development of endometritis and salpingoophoritis.
The asymptomatic form of herpes of the internal genitalia is detected in 20-40% of women suffering from herpes of the buttocks and thighs. This important circumstance must be taken into account when planning pregnancy in women with this form of GC due to the existing likelihood of developing complications of HSV infection during pregnancy.
The etiopathogenetic role of HSV in cervical cancer has been established. The above emphasizes the growing etiological role of HSV in the structure of diseases of the pelvic organs in women.
Herpes and pregnancy
The prevalence of HSV among pregnant women in the United States is 22-36%, in Europe 14-19%. Viremia in women during pregnancy can cause fetal death, stillbirth, and premature birth. Herpes viruses cause up to 30% of spontaneous abortions in early pregnancy and over 50% of late miscarriages; they are second only to the rubella virus in terms of teratogenicity (the development of fetal deformities).
The most severe forms of neonatal herpes develop when a newborn is infected with the herpes simplex virus during childbirth. With primary herpes in the mother, from 30% to 80% of children are infected, with recurrent herpes – 3–5%. Infection of the fetus during delivery, if the mother had herpetic eruptions at the end of pregnancy, occurs in 50% of women with RGG; however, 60–80% of infected children develop encephalitis.
Case from practice
A patient was admitted for consultation with a complaint of pain in the upper back and left wrist joint.
Ointments and NSAIDs had no effect. He is registered with coronary artery disease and post-infarction cardiosclerosis. On examination, the patient has slight shortness of breath, pale skin, and severe sweating. The attack began as a result of a strong psycho-emotional shock. ECG: sinus arrhythmia, single extrasystoles, left-sided hypertrophy. Along the anterior wall there is a scar after a large-focal infarction and at the same time signs of ischemia with transition to the apex and lateral part. (ST segment above isoline I, II, V1-V5, aVF). A blood test confirmed an increase in myoglobin and CPK. He was sent to the hospital with a diagnosis of acute heart attack.
Asymptomatic
This variant of the development of a heart attack is the most severe, since the person has no clinical symptoms at all.
In rare cases it is observed:
- mild shortness of breath;
- an episodic attack resembling angina pectoris or chest discomfort;
- insomnia;
- increased sweating;
- rare and quickly passing rhythm disturbances.
Such attacks occur suddenly and then pass. Since they do not cause much discomfort, the person forgets about it and does not see a doctor. The only immediate diagnostic method may be an ECG, but it is not prescribed for the same reasons. It’s not uncommon for me to see cicatricial changes on the cardiogram in a number of patients who suffered a heart attack on their legs without even knowing it.
Diagnostics
When I suspect an atypical myocardial infarction, I immediately do an ECG as a matter of urgency, monitor the blood pressure level, listen to heart sounds and assess the general condition.
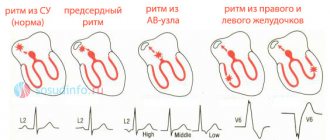
ECG
In the abdominal form, I pay special attention to the typical signs of acute cardiac ischemia along the posteroinferior wall. This is indicated by a rise in ST above the isoline, the appearance of a pathological Q wave in leads II, III, aVF, V5-V6. If the lower wall is involved in the process, then additional recording of pulses in V7 and V8 helps to detect the deviation.
The arrhythmic form complicates diagnosis, the typical picture is smoothed out. Therefore, first you need to stop the attack with medications, and only after that repeat the cardiogram. All other types of pathology require a dynamic ECG. It is best to do this every hour during the most acute period and as the patient’s condition changes in any direction or install monitoring.
Lab tests
Differential diagnosis necessarily includes the interpretation of test results from the laboratory:
- General and biochemical blood tests. Allows you to identify indirect signs of inflammation, high cholesterol, thyroid dysfunction and diabetes.
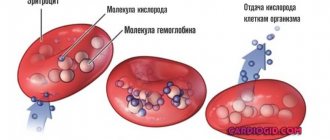
- Blood for markers (substances formed as a result of myocardial necrosis). An increase in troponin and myoglobin on the first day from the onset of ischemia, as well as creatine phosphokinase (CPK) and lactate dehydrogenase (LDH) at a later stage of disease development (up to 3 days) will be indicative.
An increase in the level of markers can also be observed in other diseases (renal dysfunction, a sharp increase in blood pressure, sarcoidosis). Therefore, such diagnostics are auxiliary.
Instrumental studies
For any form of heart attack, and especially for atypical ones, it is necessary to conduct the following studies:
- EchoCG. Helps visualize the processes occurring in the heart in real time. The presence of necrosis in the myocardium is determined by a decrease in contraction activity in this area. At the same time, the condition of the blood vessels, the operation of the valve apparatus and the size of the chambers of the organ are assessed.
- Scintigraphy. To carry it out, a radioisotope agent is introduced, which accumulates most of all in the necrosis zone. It is clearly visible on the image if the affected area is large. Used as a last resort.
In the abdominal form, you may need to consult a surgeon or gastroenterologist. Cerebral does not exclude simultaneous ischemia in the heart and brain and an encephalogram is necessary. Severe back or joint pain requires examination by a rheumatologist or vertebrologist.
Clinical forms
- Typical;
- Atypical;
- with macrosymptoms;
- with microsymptoms;
- Asymptomatic form;
It is very difficult to establish the real incidence of damage to the internal genital organs in both women and men, since in 25-40%, and according to some data, in 60% of patients, the disease occurs without subjective sensations. It can be assumed that this pathology occurs much more often than it is diagnosed.
With herpes of the internal genitalia there may be no complaints. Sometimes they note periodically appearing light mucous discharge from the urethra and vagina. During laboratory examination of smears of the cervical canal, vagina and urethra, an increased number of leukocytes is periodically noted (30-40 in the field of view of the urethral discharge, 200-250 or more in the field of view when examining smears from the vagina), indicating the presence of an inflammatory process.
The asymptomatic form of genital herpes of the internal genitalia (asymptomatic shedding of the virus) is characterized by the absence in patients of any complaints about the genital area, objective clinical data confirming inflammation. During a laboratory examination of the discharge of the urogenital tract, HSV is isolated, while in smears there are no signs of inflammation (leukocytosis). In 25-30% of men with idiopathic (when the cause of infertility is not clear) infertility, HSV is isolated from semen.
It is known that genital herpes, in 70-80% of cases, occurs in the form of a microbial association, in combination with chlamydia, urea-, mycoplasma, strepto-, staphylococci, fungal flora. It is possible that the genitals may be affected by HSV, gonococcus, treponema pallidum, and viral diseases transmitted through sexual contact, which indicates the need for a thorough examination of patients to exclude STIs and HIV infection.
Cerebral
In cases of this type, signs of cerebrovascular accident come first:
- dizziness;
- fainting, impaired consciousness (lethargy or coma);
- nausea and vomiting that does not bring relief;
- absence of chest pain or its mild severity;
- focal neurological symptoms (muscle paresis, speech impairment).
The real diagnosis can only be determined by performing an ECG or encephalography, after which the patient should be consulted by a neurologist.