Blood type inheritance
A child inherits a strictly defined number of blood group combinations from his parents. Knowing the blood type of the parents, we can guess what blood type the baby will have.
A couple with the first blood types will never have a child with a blood type other than the first. For children of spouses with the second or third groups, all available diversity is possible, from the first to the fourth.
The table shows the options for inheriting blood type:
| Father | Mother | Child |
| O(I) | O(I) | O(I) |
| A (II) | O(I) or A(II) | |
| B (III) | O(I) or B(III) | |
| AB (IV) | A (II) or B (III) | |
| A (II) | O(I) | O(I) or A(II) |
| A (II) | O(I) or A(II) | |
| B (III) | Any (I, II, III, IV) | |
| AB (IV) | A (II), B (III), AB (IV) | |
| B (III) | O(I) | O(I) or B(III) |
| A (II) | Any (I, II, III, IV) | |
| B (III) | O(I) or B(III) | |
| AB (IV) | A (II), B (III), AB (IV) | |
| AB (IV) | O(I) | A (II) or B (III) |
| A (II) | A (II), B (III), AB (IV) | |
| B (III) | A (II), B (III), AB (IV) | |
| AB (IV) | A (II), B (III), AB (IV) |
Compatibility of blood groups and Rhesus for transfusion
The blood type depends on the antigen that is located on the surface of the red blood cell. There are two types of antigens on red blood cells. They have different structures and define 4 types according to the AB0 system:
- A;
- IN;
- AB;
- 0.
In this system, A and B indicate antigens, and 0 (zero) indicates their absence. On the surface of red blood cells in the blood of group A there is only antigen A, B - only antigen B. Red blood cells of group AB contain both antigens, and 0 does not contain any. Brunilda Nazario explains in her article what blood groups are and how they differ.
Why select a donor's blood type?
The need to select donor biomaterial is a complex, intimate, taboo issue in society. Often couples come to us who want to keep it a secret. Matching the blood types of the donor and the partner becomes important due to the availability of blood group testing. It is important to understand that the blood type variations a child may have depend on the blood type of the parents.
Selection of donor by blood type for married couples
When selecting a sperm donor.
In this case, it does not mean at all that your choice should be strictly limited only to your spouse’s blood type. It is necessary to take into account the options for combinations of blood groups between spouses and choose a donor with a blood type that will give the same options. For example, if you have the fourth blood group, and the partner for whom the biomaterial is being selected has the second, then you should choose from donors with the second, third and fourth blood groups.
Or, suppose both spouses have the third blood group, then it is necessary to consider donors with the first and third blood groups.
| Male blood type | Woman's blood type | Sperm donor |
| O(I) | O(I) | O(I) |
| A (II) | O(I) or A(II) | |
| B (III) | O(I) or B(III) | |
| AB (IV) | O(I) | |
| A (II) | O(I) | O(I) or A(II) |
| A (II) | O(I) or A(II) | |
| B (III) | Any (I, II, III, IV) | |
| AB (IV) | A (II), B (III), AB (IV) | |
| A (II) | O(I) | O(I) or A(II) |
| A (II) | O(I) or A(II) | |
| B (III) | Any (I, II, III, IV) | |
| AB (IV) | A (II), B (III), AB (IV) | |
| B (III) | O(I) | O(I) or B(III) |
| A (II) | Any (I, II, III, IV) | |
| B (III) | O(I) or B(III) | |
| AB (IV) | A (II), B (III), AB (IV) | |
| AB (IV) | O(I) | AB (IV) |
| A (II) | A (II), B (III), AB (IV) | |
| B (III) | A (II), B (III), AB (IV) | |
| AB (IV) | A (II), B (III), AB (IV) |
When selecting egg donors
Here, too, you don’t need to limit yourself to a woman’s blood type. In this case, as when choosing a sperm donor, we select an egg donor based on the possible blood types of both spouses.
| Male blood type | Woman's blood type | Egg donor |
| O(I) | O(I) | O(I) |
| A (II) | O(I) or A(II) | |
| B (III) | O(I) or B(III) | |
| AB (IV) | AB (IV) | |
| A (II) | O(I) | O(I) or A(II) |
| A (II) | O(I) or A(II) | |
| B (III) | Any (I, II, III, IV) | |
| AB (IV) | A (II), B (III), AB (IV) | |
| B (III) | O(I) | O(I) or B(III) |
| A (II) | Any (I, II, III, IV) | |
| B (III) | O(I) or B(III) | |
| AB (IV) | A (II), B (III), AB (IV) | |
| AB (IV) | O(I) | AB (IV) |
| A (II) | A (II), B (III), AB (IV) | |
| B (III) | A (II), B (III), AB (IV) | |
| AB (IV) | A (II), B (III), AB (IV) |
Be that as it may, selecting a donor based on blood type remains an ethical issue. From a medical point of view, it does not matter.
AB0 system
This blood group system was discovered by Karl Landsteiner in 1900, for which he was awarded the Nobel Prize in 1930. The erythrocyte is covered with a plasmalemma about 7 nm thick, into which antigens of the ABO systems and the Rh factor are embedded. Each person's blood plasma contains antibodies against red blood cell antigens that are not contained in his own blood. K. Landsteiner described four blood groups (Fig. 1). When blood taken from different people is mixed and blood groups are incompatible, agglutination (sticking together) of red blood cells occurs as a result of the antigen-antibody reaction.
Rice. 1. Four blood groups according to the AB0 system.
A number of specific polysaccharide-amino acid complexes that have antigenic properties are built into the erythrocyte membrane. Glycosylation is ensured by special enzymes - glycosyltransferases, the genes of which are located on chromosome 9 and have three different alleles: A, B and 0. The protein of gene 0 transfers a short oligosaccharide chain; in the case of gene A, N-acetyl-D-galactosamine is additionally attached to this chain , in the presence of gene B – D-galactose (Fig. 2). The work of gligosyltransferases A and B ensures the formation of the corresponding agglutinogens.
Rice. 2. Structure of oligosaccharides of the H-antigen, which is responsible for the blood groups of the AB0 system.
Specific agglutinins anti-A (α) and anti-B (β) are formed in the blood plasma. Essentially, these are antibodies produced by the immune system. They are constantly contained in human blood and are believed to be produced as an immune response to intestinal microflora. To prevent agglutination, pairs A and anti-A, B and anti-B should not be present in the blood at the same time. Therefore, the immune system learns to recognize its own red blood cells and not react to their agglutinogens.
Thus, the following combinations are possible:
- I (0) – anti-A+anti-B;
- II (A) – A+anti-B;
- III (B) – B+anti-A;
- IV (AB) – A+B.
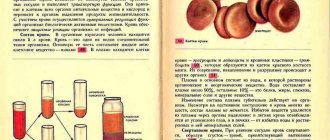
When transfusing blood, to prevent red blood cells from sticking together, it is necessary that the donor's red blood cells do not contain agglutinogens, to which the recipient's blood plasma contains agglutinins. The blood transfusion scheme is shown in Fig. 3. Erythrocytes of blood group I do not contain agglutinogens, it can be transfused to any recipient; people with this blood group are called universal donors. Red blood cells of blood group IV contain both agglutinogens, but there are no agglutinins in the plasma, therefore, people with this blood group can be transfused with any other, and such people are called universal recipients.
Rice. 3. Blood transfusion scheme.
The exception to this pattern is the Bombay phenomenon. It was discovered through human blood transfusions during a malaria outbreak in India in 1952. It turned out that some people do not form an oligosaccharide backbone to which glycosyltransferases A and B transfer additional sugars. Thus, even if genes A and B are present, glycosyltransferases do not have a substrate with which to work. In such people, in addition to the presence of anti-A and anti-B agglutinins, agglutination occurs even after transfusion of group I blood. Carriers of such blood are universal donors.
Blood group testing is quite simple. To do this, a drop of the blood being tested is mixed with sera of blood groups I-III. Depending on where the agglutination occurred, the blood type can be determined (Fig. 4). In the case of the Bombay phenomenon, agglutination will occur in all three wells. Currently, instead of serums, tsoliklones are used - monoclonal antibodies to agglutinogens.
It is worth noting that the agglutination reaction occurs between red blood cells and blood plasma. When mixing blood plasma from different groups, agglutination will not occur.
Rice. 4. Blood group analysis. 1 – I (0) group, 2 – II (A) blood group, 3 – III (B) blood group, 4 – IV (AB) blood group.
Blood donation in facts and figures
There is a scientifically proven fact that blood donation is beneficial for a healthy person. It's like a shock to the body due to blood loss. Man is a representative of the animal kingdom, and in the process of evolution he was adapted to lose blood from time to time. And over the last, say, 150 years, thanks to scientific and technological progress, medical capabilities, and improved living standards in general, blood loss has been minimized. Women physiologically lose blood once a month, but men do not lose blood at all. Their bodies are not adapted, and losing a relatively small volume of blood can be dangerous. And if a person is a regular donor, then he is trained in blood donation, and blood loss in emergency situations will not be so dangerous for him. In general, blood loss is a signal to mobilize the entire body. All systems begin to function under conditions aimed at compensating for blood loss. And, of course, blood donation has great psychological and social value. When a person goes for this, he tunes in to altruism.
In order to fully satisfy the need of hospitals for donor blood, it is necessary that for every 1000 people there should be 40 donations per year.
There are types of donation in which only plasma or granulocytes are taken from the body. After this procedure, recovery occurs faster than with a regular donation.
Scientists from the University of Kuopio in Finland, who followed a group of 2,862 men over 40 years of age for 9 years, estimate that regular donation reduces the risk of myocardial infarction by 88%.
Blood groups O (I), A (II), B (III) and AB (IV) are found not only in humans, but also in monkeys. True, our closest relatives, chimpanzees, during the course of evolution, for some reason, lost their III and IV blood groups, but their I and II groups are exactly the same as ours. In the first half of the twentieth century, experiments were carried out that showed that we could well be donors for each other. This is not practiced due to the risk of transmitting infections - and in general, it is easier to find a human donor than a chimpanzee donor!
Many donors note that donating blood dramatically improves their mood. Most likely, this is due not only to the satisfaction of a good deed, but also to the fact that blood loss is stress for the body, and under stress our brain releases endorphins.
In old school textbooks, the concepts of “universal donor” and “universal recipient” were used, but today in the vast majority of cases, blood of the same group as that of the recipient is used. The need for blood of all groups is equally great. If the group is rare, this means that there are few such donors; if the group is common, it means there are many recipients in need of such blood.
Prevalence of different blood groups in the world:
- O(I) Rh + 36%
- A(II) Rh + 28%
- B(III) Rh + 21%
- AB(IV) Rh + 5%
- O(I) Rh - 4%
- A(II) Rh – 4%
- B(III) Rh - 1%
- AB(IV) Rh – 1%
Head of the City Center for Transfusiology of the 6th City Clinical Hospital,
transfusiologist of the highest qualification category, candidate of medical sciences O.V. Klimovich
The importance of Rh for people with 4 BG
An equally important issue during blood transfusion or conception of offspring is the Rh factor, which divides each GC into two subgroups: negative and positive.
We will talk about additional antigen D, which is also a protein product and is located on the erythrocyte membrane. Its presence is recorded in Rh-positive people, and its absence in Rh-negative people. The indicator is of great importance in determining blood compatibility.
People who do not have the Rh antigen have more pronounced immune defense reactions, for example, implant rejection or allergies occur more often.
Prevalence of people by BG and Rh factor
Blood Center
When a doctor talks about your blood type, he usually means two things: your ABO blood group and your Rh (Rh factor).
A person's blood type is determined by the antigens found on their red blood cells. An antigen is a structure on the surface of a cell. If it is foreign to the body, then the human defense system will react to it. Therefore, it is necessary to take into account blood groups when transfusion: the donor’s blood group is determined at the Blood Center, and the patient’s blood group is determined before the transfusion.
AB0 system
The most important is the ABO blood group system, according to which blood is divided into groups A, B, O and AB. It is determined by two antigens located on the surface of red blood cells:
- group A - only antigen A is found on the surface of red blood cells
- group B – only antigen B is found on the surface of red blood cells
- group AB - both A and B antigens are found on the surface of red blood cells
- group O - there is neither antigen A nor antigen B on the surface of red blood cells.
If a person has blood type A, B or 0, then his blood plasma also contains antibodies that destroy antigens that the person himself does not have. Examples: If you have blood type A, then you cannot be transfused with blood of group B, because in this case there are antibodies in your blood that fight against B antigens. If you have blood type 0, then there are antibodies in your blood that fight both against A and B antigens.
If a person has blood type AB, then he does not have such antibodies, so he can be transfused with blood of any group. Therefore, a carrier of blood group AB can be called a universal patient.
A carrier of blood group 0 with a negative Rh factor is in turn called a universal donor, since his red blood cells are suitable for all patients.
Rhesus (Rh) - accessory
Rh factor (Rh) can be positive (+) or negative (-). This depends on the presence of antigen D on the surface of red blood cells. If the D antigen is present, the person is considered Rh positive, and if the D antigen is absent, then the person is Rh negative.
If a person is Rh negative, they may develop antibodies when they come into contact with Rh positive blood (for example, during pregnancy or through a blood transfusion). These antibodies can cause problems during pregnancy for a woman who is Rh negative if she is carrying a child who is Rh positive.
In addition to the ABO and Rh systems, about thirty more blood group systems have been discovered to date. Clinically, the most important of these are the Kell, Kidd and Duffy systems. The Kell system also tests the blood of donors.
How is blood type determined?
To determine the blood type, it is mixed with a reagent containing known antibodies.
Three drops of blood taken from one person are applied to the base: the anti-A test reagent is added to one drop, the anti-B test reagent is added to another drop, and the anti-D test reagent is added to the third, i.e. test reagent Rh. If blood clots form in the first drop, i.e. red blood cells stick together (agglutination), then the person has antigen A. If the red blood cells in another drop do not stick together, then the person does not have antigen B; and if agglutination occurs in the third drop, this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive.
The compatibility of the blood type of the donor and the recipient is extremely important, otherwise the recipient may have dangerous reactions to the blood transfusion.
Inheritance of blood groups
A person inherits from his father and mother to the same extent. Therefore, the hereditary substance has a double structure: one part from the mother and the other from the father. Speaking about the inheritance of blood groups, it is necessary to keep in mind that:
- Most of our genes exist in two copies
- Each parent transfers (based on a random selection) one of these copies to their children
- Genes occur in different versions (alleles)
- Some versions of the gene are stronger than others
| AVO system | Rh system | |||||
In the AB0 system, antigens are presented in three versions A, B and 0. Given that the hereditary substance contains two parts, six different combinations can occur: Genes
The stronger part appears, both equally, or a combination of both. In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows: | ||||||
| Genes | Blood type | |||||
| A.A. | A | |||||
| A0 | A | |||||
| AB | AB | |||||
| B0 | B | |||||
| BB | B | |||||
| 00 | 0 | |||||
Example: A mother has a combination of A0 genes in her hereditary substance, and her blood type is designated A (at the same time, she is a carrier of the blood group gene 0, and there is a possibility that she will pass it on to the child). The father's blood type is designated 0, and his hereditary substance contains a combination of genes 00. Accordingly, he can only pass on 0 to the child, i.e. lack of antigens. Thus, their child may have blood type A (A0) or 0 (00).
In the Rh system, things are somewhat simpler, since there are only two options: the D antigen is either present (Rh factor positive) or absent (Rh factor negative). A positive Rh factor dominates over a negative one. Genes
| Blood type | |
| +/+ | positive |
| +/- | positive |
| -/- | negative |
Example: if the mother has Rh positive blood, and there is a hidden negative version, that is, the (+/-) allele, and the father has exactly the same combination, and they both pass on the negative allele, then two Rh positive parents can be born a child with a negative Rh factor.
Plasma compatibility
The rules for plasma compatibility are identical to the rules for compatibility by blood group, however, the following feature must be noted here: due to the content of the first group of agglutinins α and β in the plasma, this plasma should be administered in a limited volume (Ottenberg’s rule). And plasma of the fourth group can be transfused to patients with any group, because it does not contain agglutinins at all.
In cases where the need for urgent blood transfusion exceeds the risk level of possible consequences from blood transfusion of samples that have not been fully tested, the responsibility falls on the doctor. Therefore, if possible, surgical procedures should be delayed until adequately matched blood samples can be found. Also, special attention should be paid to clear and correct filling out of documents, for which purpose the office must be kept quiet and orderly on the desktop.