Lung tissue contains a large number of tiny sacs called alveoli. Gas exchange, the actual process of respiration, occurs in them.
Our expert in this field:
Sergeev Pyotr Sergeevich
Oncologist, surgeon, chemotherapist, Ph.D. Member of the international society of surgical oncologists EESG
Call the doctor Reviews about the doctor
The outside of the lungs is covered with a thin film - the pulmonary pleura. They are located in the chest, the surface of which is also lined by the pleura, it is called the parietal. There is a small gap between the two layers of pleura, it is called the pleural cavity.
Fluid can accumulate both in the alveoli of the lungs and in the pleural cavity. In the first case it is pulmonary edema, in the second case it is hydrothorax.
The accumulation of fluid in the lungs can occur rapidly, have an acute form, or increase and progress over a long time.
Oncological causes
The cause of pulmonary edema or hydrothorax in cancer patients can be both the cancer itself and its treatment.
For example, fluid accumulation and pulmonary edema can occur as a result of chemotherapy with toxic drugs that depress the heart, or as a complication of radiation therapy. On the other hand, the functioning of the heart can be disrupted by the tumor process.
Another possible reason is disruption of the lymphatic system due to damage to the lymph nodes by metastases or germination of a cancerous tumor.
Most often, fluid accumulation occurs in cancer of the lung, breast, ovary, stomach, body and cervix, melanoma, lymphoma, sarcoma, and leukemia.
With a malignant tumor of the pleura (mesothelioma), the permeability of the vascular wall of the capillaries increases. Fluid from the blood actively enters the lungs, and its pumping by the lymphatic system, on the contrary, worsens. As a result, stagnation and fluid accumulation occurs.
Other reasons are also possible, for example, compression of the heart by a tumor, tumor growth into the superior vena cava, formation of metastasis in the pericardium, tumor growth into the lumen of the bronchus and its overlap.
Oncological diseases are characterized by a gradual, slow development of hydrothorax and pulmonary edema.
Take care of yourself, book a consultation now
Message sent!
expect a call, we will contact you shortly
Consequences of pulmonary edema in the elderly
Pulmonary edema syndrome is dangerous because various complications often develop after it:
- a secondary infection may occur, which can lead to pneumonia, which, in combination with edema, is very difficult to treat;
- The lack of oxygen that accompanies pulmonary edema has a detrimental effect on the functioning of internal organs, especially the brain and heart. The consequences of such exposure can be irreversible and lead to human death;
- development of pneumofibrosis and segmental atelectasis.
The recovery period depends on the underlying disease, the general condition of the body, the patient’s age and other factors. Treatment lasts on average from a week to a month.
If there are no complications and quality medical care is provided, then after ten days the patient will be able to go home.
Toxic pulmonary edema is considered the most complex and prone to recurrence. Patients with this diagnosis spend at least three weeks in the hospital.
But regardless of the causes of pulmonary edema, the disease is considered very serious. In acute alveolar edema, the mortality rate is 20–50%. If swelling accompanies myocardial infarction or anaphylactic shock, the patient dies in 90% of cases.
Even with the timely provision of qualified medical care, there is a high probability of complications such as ischemic damage to the viscera, pneumonia, pulmonary atherosclerosis, etc. If the underlying disease was eliminated in a timely manner, then there is still a risk of resumption of pulmonary edema. In any case, the earlier treatment is started, the greater the chance of survival.
Non-cancer reasons
From the bronchi, through their branches, bronchioles, air enters the alveoli of the lungs. On the other hand, they are surrounded by capillary vessels that have a thin wall. Through it, carbon dioxide is released from the blood into the alveoli, and oxygen enters the blood.
A common cause of fluid accumulation in the lungs is heart failure and high blood pressure (hypertension), which “squeezes” fluid through the vascular wall into the alveolar cavity. In turn, heart failure can be a consequence of a heart attack.
Other possible causes are liver disease (cirrhosis), kidney disease (renal failure), bronchial asthma, diabetes mellitus, pneumonia, tuberculosis, pleurisy, trauma, pulmonary contusion, thromboembolism, intoxication.
The kidneys are responsible for removing fluid from the body. When their work is disrupted, edema occurs and fluid accumulates in different parts of the body, including the lungs.
Health care
Emergency therapy includes the following procedures:
- Using an oxygen mask (oxygenation). If the case is urgent, then the supply of oxygen through a mask is replaced by artificial ventilation.
- The patient is given morphine as a pain reliever and sedative.
- Aminophylline is also introduced, which helps remove excess sodium from the body, dilate the bronchi and improve blood circulation in the renal glands.
- At the same time, doctors monitor the patient's blood pressure. If it exceeds the norm, then the patient is injected with sodium nitroprusside, and if the blood pressure is too low, then dobutamine is injected.
Further therapy includes taking medications. The doctor may prescribe:
- hormonal drugs;
- antibiotics;
- hepatoprotectors;
- antihistamines.
Symptoms
One of the most characteristic symptoms of fluid accumulation in the lungs is shortness of breath. First it occurs during physical activity, then at rest.
Shortness of breath is accompanied by a feeling of lack of air, rapid breathing, suffocation, weakness, fear of death, a feeling of incomplete expansion of the lungs when breathing, and insufficient filling of them with air.
Symptoms usually worsen when lying down. An acute attack of suffocation can cause death.
Insufficient breathing leads to oxygen starvation, hypoxia - pale and blue skin (cyanosis), dizziness, darkening of the eyes, fainting, and headaches.
The nervous system, brain, and psyche suffer from insufficient breathing; restlessness, nervousness, anxiety, and numbness in the arms or legs appear.
Due to the accumulated fluid, body weight increases. Depending on the presence or absence of an inflammatory process, body temperature may be increased or decreased.
Low body temperature is a specific sign of fluid accumulation in the lungs.
Other symptoms are pain in the lung (usually at the bottom or side), persistent, hacking dry cough with the release of viscous mucus with ichor, a feeling of constriction, heaviness in the chest, sweating (especially at night)
We will call you back
Message sent!
expect a call, we will contact you shortly
Complications
The main thing that threatens pulmonary edema in an elderly person is the lack of oxygen in the tissues. Even if the disease has been stopped, the brain will experience serious changes, and the tissues of the heart and lungs will suffer.
Also among other serious consequences of suffering from pulmonary edema are:
- formation of congestion in the lungs;
- organ ischemia;
- emphysema.
Due to oxygen starvation, the patient’s memory will deteriorate, during the daytime he will constantly feel sleepy, general lethargy will be felt, and his mood will begin to deteriorate. You will have to carefully monitor your own condition in order to notice serious deterioration in time and consult a doctor.
Pulmonary edema in old age is a serious pathology. Even if the disease manifests itself in a protracted or subacute form, the risk of complications after therapy is high. An immediate or acute syndrome practically does not allow saving the patient. So at the first symptoms indicating the development of the disease, you need to undergo an examination and consult a doctor so that it is not too late.
Diagnostics
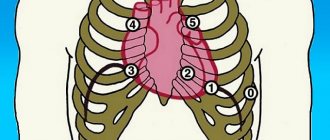
At the initial appointment, the doctor conducts an examination (when breathing, the right or left side of the chest may be delayed), taps, and listens to the patient with a phonendoscope.
The purpose of diagnostic studies is to establish not only the fact and severity of pulmonary edema and/or hydrothorax, but also its cause.
A biochemical blood test, an analysis of the content of gases in the blood, and coagulation help to do this.
Using an X-ray, you can clearly see the accumulation of fluid, estimate its volume, detect a tumor, and damage to the lymph nodes.
More detailed, additional information is provided by computer and magnetic resonance imaging (CT, MRI), ultrasound of the chest.
To confirm or exclude cancer, a puncture or biopsy is performed, followed by a morphological examination (cytological, histological). In the first case, fluid is taken from the pleural cavity, in the second, a fragment of pleural tissue is taken.
Make an appointment with a doctor now
Message sent!
expect a call, we will contact you shortly
How to give first aid
First aid to a patient who has pulmonary edema should be provided by those around him:
- First of all, make the victim sit comfortably, his legs should hang over the seat. This will help reduce the amount of blood entering the pulmonary circle.
- In some cases, the patient can be given medications. For example, if the swelling was caused by heart disease, then it is necessary to put nitroglycerin under the victim’s tongue. Diuretics that reduce venous return (eg, Furosemide) may also help. This medicine is administered intravenously, but the dosage is selected only by a doctor.
- Next, to reduce venous return, you need to apply a cuff to your leg or arm. This will partially compress the veins, leaving only a small flow of air under the pressure cuff. It is especially useful for pulmonary edema in bedridden elderly patients.
- Before the ambulance arrives, the patient should be given sedatives (Relanium is excellent). During this procedure, the amount of catecholamines in the bloodstream will decrease, and the venous flow of blood to the heart muscle will also decrease.
- If the patient suddenly begins to foam, then you need to moisten a cotton swab in medical alcohol and let the patient smell it. By inhaling ethyl alcohol vapor for ten minutes, the patient will be able to hold out until the ambulance arrives. However, sometimes the reaction to alcohol vapor can be completely unexpected - instead of relief, the patient may feel that he does not have enough air. In this case, the tampon should be immediately removed from the nose.
Treatment
If the cause of fluid accumulation is not cancer, drug therapy is used with diuretics (diuretics), cardiac drugs, anti-inflammatory drugs, antibiotics, bronchodilators, expectorants and other drugs as indicated.
For malignant tumors, the use of such drugs may be symptomatic, or they are used to treat concomitant diseases. The main treatments used are chemotherapy or surgery.
- Thoracentesis – pumping out fluid from the pleural cavity. A puncture is made in the chest wall with a thin needle, after which the effusion is pumped out through a tube using an electric suction.
The procedure is performed under local anesthesia. It gives a quick effect, relieves the condition, but after some time the fluid accumulates again, hydrothorax resumes, and this requires repeat thoracentesis.
To avoid repeated punctures of the chest wall, a port system is installed in it, connected by a drainage tube to the pleural cavity. When fluid accumulates, the port opens and the effusion is pumped out using an electric suction device.
The intrapleural port system allows not only to pump out accumulated fluid, but also to inject drugs into the pleural cavity.
- Pleurodesis - introduction into the pleural cavity of sclerosing substances that glue the thoracic and parietal pleura. After this, the liquid has nowhere to accumulate. Pleurodesis is usually performed after draining the effusion (thoracentesis).
In case of oncological diseases, chemotherapy drugs are used for pleurodesis, which have a cytostatic effect and at the same time glue the pleural lobes together.
Along with cytostatics, the international clinic Medica24 uses immunomodulators that destroy cancer cells and show very good results of pleurodesis.
- Removal of pleura for oncological diseases in our clinic, as a rule, it is performed laparoscopically, through minimally invasive surgery.
A thoracoscope with a video camera and surgical instruments are inserted through the punctures. This allows you to avoid incisions and reduce traumatic effects.
The material was prepared by oncologist, thoraco-abdominal surgeon of the International Clinic Medica24 Alexander Valerievich Korotaev.
Prevention of pulmonary edema in the elderly
Prevention of pulmonary edema in older people includes timely treatment of the underlying disease. You need to be constantly monitored by medical specialists, not to come into contact with harmful substances and toxins, not to abuse alcohol and overeating, follow the instructions for using medications, and lead a healthy lifestyle.
If a person has chronic diseases or suffers from hypertension, then you need to regularly visit the doctor and follow all his prescriptions. Secondary, but no less important, measures to prevent pulmonary edema in older people are: a positive attitude, proper nutrition and an active lifestyle.
It is impossible to predict when an attack will occur, but you can reduce the likelihood of it occurring. You also need to remember that timely medical care is the key to saving lives.
To reduce the risk of pulmonary edema in bedridden elderly people, they need to purchase an orthopedic mattress. Even such, at first glance, a trifle can prevent the development of congestive pneumonia.
The patient will need a varied diet high in vitamins, breathing exercises and therapeutic massage.
The air in the room must be humid. This is important to prevent the occurrence of pneumonia. To increase humidity, you can use a special device or ventilate the room in rainy weather.
You need to constantly listen to the breathing of a person confined to bed. It should be smooth and clean, without gurgling or wheezing. If extraneous sounds appear, you must urgently call an ambulance.
For heart failure
In heart failure, systemic circulation becomes significantly more difficult. Insufficient blood flows to the alveoli, they become inflamed. When turning into an acute form, water and oxygen form abundant foam.
Pneumonia develops due to heart pathologies. If therapy is absent or begins untimely, swelling continues to increase.
The condition manifests itself in a chronic form and is protracted. Symptoms may be erased. The doctor does not immediately understand whether the underlying cause is respiratory or heart failure.
To identify the damaging factor, a comprehensive examination is required. General clinical tests of biological fluids (blood, urine, leukocyte formula, coagulogram), ultrasound, MRI, CT, radiography are prescribed.
ethnoscience
You can treat effusion at home only if there is a small amount of it (as determined by x-ray), mild symptoms, and after consultation with your doctor. You can get rid of effusion in the lungs using folk remedies after eliminating the causative factor - the underlying disease that led to the complication.
To remove excess water, take 1 tbsp. spoons of parsley decoction: 500 g of fresh parsley pour 700 ml of milk, bring to a boil, cool. To speed up the process of removing phlegm, drink honey tincture. Compound:
- 200 g of dried or fresh viburnum berries;
- linden flowers, knotweed, plantain - 2 tbsp. spoons;
- coltsfoot - 1-3 sheets;
- vodka – 500 ml;
- honey – 50 ml.
Herbs and berries are poured with vodka, honey is added, stirred until the honey dissolves. Leave for 2 days in a dark place. Take 1 tbsp. spoons 3 times a day until sputum stops coming out. To get rid of a dry cough, stop an attack of bronchitis, and reduce the severity of inflammatory processes in the lungs, take anise decoction. Compound:
- flax seeds - 1 tbsp. l;
- boiling water – 200 ml;
- cognac – 1 tbsp. l;
- honey - 1 tbsp. l.
Pour boiling water over the seeds, cook over low heat for 10 minutes, cover with a lid to infuse for 15 minutes. Take 4 times a day, 1 tbsp. spoon. To strengthen the immune system and speed up the discharge of sputum, take onion juice once a day, 1 tbsp. l: one finely chopped onion sprinkled with 1-2 tbsp. l. sugar, after 10-15 minutes squeeze the juice through cheesecloth.
Important! Traditional methods of treatment can be combined with drug therapy.
Contraindications to pleurodesis
- Pathological conditions that prevent the expansion of the lung. For example, it could be congestive lung - stagnation of blood in the pulmonary veins.
- Insufficient drainage. Before performing pleurodesis, fluid must be removed from the pleural cavity.
- Recent chest radiation therapy and chest tube placement for more than 10 days reduce the likelihood that pleurodesis will be performed successfully.
- An assessment of the patient's condition according to the Karnofsky index of less than 50% and a body mass index of less than 25 kg/m2 are also risk factors for unsuccessful pleurodesis.
- Infectious process in the pleura.
- Discharge of more than 150 ml of fluid through the drainage tube. The optimal situation for pleurodesis is the release of no more than 100 ml of fluid during the last 24 hours.
- The patient's categorical refusal to undergo the procedure.
- The patient's life expectancy is less than three months. In such cases, to alleviate the patient's condition, thoracentesis is periodically performed.
BIBLIOGRAPHY
- Renkin E: Some consequences of capillary permeability to macro-molecules: tarling's hypothesis reconsidered. Am J Physiol 1986, 250:H706–H710.
- Staub N: The pathogenesis of pulmonary edema. Prog Cardiovasc Dis 1980, 23:53–80.
- Matthay MA: Pathophysiology of pulmonary edema. Clin Chest Med 1985, 6:301–314.
- Lewis FR, Elings VB, Sturm JA: Bedside measurement of lung water. J Surg Res 1979, 27:250–261.
- Sivak ED, Starr NJ, Graves JW, et al.: Extravascular lung water values in patients undergoing coronary artery bypass surgery. Crit Care Med 1982, 10:593–596.
- Sibbald WJ, Warshawski FJ, Short AK, et al.: Clinical studies of mea-suring extravascular lung water by the thermal dye technique in critically ill patients. Chest 1983, 83:725–731.
- Gallagher JD, Moore RA, Kerns D, et al.: Effects of advanced age on extravascular lung water accumulation during coronary artery bypass surgery. Crit Care Med 1985, 13:68–71.
- Bongard FS, Matthay M, Mackersie RC, Lewis FR: Morphologic and physiologic correlates of increased extravascular lung water. Surgery 1984, 96:395–403.
- Staub NC: Clinical use of lung water measurements. Report of a workshop. Chest 1986, 90:588–594.
- Schuster DP: The evaluation of pulmonary endothelial barrier function: quantifying pulmonary edema and lung injury. In: Pulmonary Edema. Edited by Matthay MA, Ingbar DH. New York: Marcel Dekker, Inc., 1998:121–161.
- Snashall PD, Keyes SJ, Morgan BM, et al.: The radiographic detection of acute pulmonary oedema. A comparison of radiographic appearances, densitometry and lung water in dogs. Br J Radiol 1981, 54:277–288.
- Gattinoni L, Presenti A, Torresin A, et al.: Adult respiratory distress syndrome profiles by computed tomography. J Thorac Imaging 1986, 1:25–30.
- Wheeler A, Carroll F, Bernard G: Radiographic issues in adult respi-atory distress syndrome. New Horiz 1993, 1:471–477.
- Halperin B, Feeley T, Mihm F, et al.: Evaluation of the portable chest roentgenogram for quantitating extravascular lung water in critically ill adults. Chest 1985, 88:649–652.
- Eisenberg PR, Hansbrough JR, Anderson D, Schuster DP: A prospecious study of lung water measurements during patient management in an intensive care unit. Am Rev Respir Dis 1987, 136:662–668.
- Hedlund LW, Vock P, Effmann EL, Lischko MM, Putman CE: Hydrostatic pulmonary edema. An analysis of lung density changes by computed tomography. Invest Radiol 1984, 19:254–262.
- Forster BB, Muller NL, Mayo JR, et al.: High-resolution computed tomography of experimental hydrostatic pulmonary edema. Chest 1992, 101:1434–1437.
- 18. Mayo JR: Magnetic resonance imaging of the chest. Where we stand. Radiol Clin North Am 1994, 32:795–809.
- Lancaster L, Bogdan AR, Kundel HL, McAffee B: Sodium MRI with coated magnetite: measurement of extravascular lung water in rats. Magn Reson Med 1991, 19:96–104.
- Cutillo AG, Morris AH, Ailion DC, et al.: Assessment of lung water distribution by nuclear magnetic resonance. A new method for quantifying and monitoring experimental lung injury. Am Rev Respir Dis 1988, 137:1371–1378.
- Morris AH, Blatter DD, Case TA, et al.: A new nuclear magnetic resonance property of the lung. J Appl Physiol 1985, 58:759–762.
- Cutillo AG, Morris AH, Ailion DC, Durney CH, Case TA: Determination of lung water content and distribution by nuclear magnetic resonance imaging. J Thorac Imag 1986, 1:39–51.
- Mayo JR, Muller NL, Forster BB, Okazawa M, Pare PD: Magnetic res-onance imaging of hydrostatic pulmonary edema in isolated dog lungs: comparison with computed tomography. Can Assoc Radiol J 1990, 41:281–286.
- Wexler HR, Nicholson RL, Prato FS, et al.: Quantitation of lung water by nuclear magnetic resonance imaging. A preliminary study. Invest Radiol 1985, 20:583–590.
- Phillips DM, Allen PS, Man SF: Assessment of temporal changes in pulmonary edema with NMR imaging. J Appl Physiol 1989, 66:1197–1208.
- Caruthers SD, Paschal CB, Pou NA, Roselli RJ, Harris TR: Regional measurements of pulmonary edema by using magnetic resonance imaging. J Appl Physiol 1998, 84:2143–2153.
- Rhodes CG: Measurement of lung water using nuclear magnetic resonance imaging [letter]. Br J Radiol 1986, 59:1135–1136.
- Cutillo A, Goodrich K, Krishnamurthy G, et al.: Lung water measure-me by nuclear magnetic resonance: correlation with morphome-try. J Appl Physiol 1995, 79:2163–2168.
- Mayo JR, MacKay AL, Whittall KP, Baile EM, Pare PD: Measurement of lung water content and pleural pressure gradient with magnetic resonance imaging. J Thorac Imag 1995, 10:73–81.
- Berthezene Y, Vexler V, Jerome H, et al.: Differentiation of capillary leak and hydrostatic pulmonary edema with a macromolecular MR imaging contrast agent. Radiology 1991, 181:773–777.
- Cutillo AG, Goodrich KC, Ganesan K, et al.: Alveolar air/tissue inter-face and nuclear magnetic resonance behavior of normal and edematous lungs. Am J Respir Crit Care Med 1995, 151:1018–1026.
- Schuster DP: Positron emission tomography: theory and its application to the study of lung disease. Am Rev Respir Dis 1989, 139:818–840.
- Schuster DP, Marklin GF, Mintun MA, Ter-Pogossian MM: PET measurement of regional lung density: 1. J Comput Assist Tomogr 1986, 10:723–729.
- Rhodes C, Hughes, JMB: Pulmonary studies using positron emission tomography. Eur Respir J 1995, 8:1001–1017.
- Schuster DP, Mintun MA, Green MA, Ter-Pogossian MM: Regional lung water and hematocrit determined by positron emission tomography. J Appl Physiol 1985, 59:860–868.
- Schuster DP, Marklin GF, Mintun MA: Regional changes in extravascular lung water detected by positron emission tomography. J Appl Physiol 1986, 60:1170–1178.
- Velazquez M, Haller J, Amundsen T, Schuster DP: Regional lung water measurements with PET: accuracy, reproducibility, and lin-earity. J Nucl Med 1991, 32:719–725.
- Spinale FG, Reines HD, Cook MC, Crawford FA: Noninvasive estimation of extravascular lung water using bioimpedance. J Surg Res 1989, 47:535–540.
- Zellner JL, Spinale FG, Crawford FA: Bioimpedance: a novel method for the determination of extravascular lung water. J Surg Res 1990, 48:454–459.
- Nierman DM, Eisen DI, Fein ED, et al.: Transthoraic bioimpedance can measure extravascular lung water in acute lung injury. J Surg Res 1996, 65:101–108.
- Adler A, Amyot R, Guardo R, Bates JHT, Berthiaume Y: Monitoring changes in lung air and liquid volumes with electrical impedance tomography. J Appl Physiol 1997, 83:1762–1767.
- Effros RM: Lung water measurements with the mean transit time approach. J Appl Physiol 1985, 59:673–683.
- Sivak ED, Wiedemann HP: Clinical measurement of extravascular lung water. Crit Care Clin 1986, 2:511–526.
- Allison RC, Carlile PV Jr, Gray BA: Thermodilution measurement of lung water. Clin Chest Med 1985, 6:439–457.
- Pfeiffer U, Backus G, Blumel G, et al.: A fiberoptics based system for integrated monitoring of cardiac output, intrathoracic blood volume, extravascular lung water, O 2 saturation, and a–v differ-ences. In: Practical Applications of Fiberoptics in Critical Care Monitoring. Edited by Lewis F, Pfeiffer U. Berlin: Springer-Verlag, 1990: 114–125.
- Schuster DP, Calandrino FS: Single versus double indicator dilution measurements of extravascular lung water. Crit Care Med 1991, 19:84–88.
- Sibbald WJ, Short AK, Warshawski FJ, Cunningham DG, Cheung H: Thermal dye measurements of extravascular lung water in critically ill patients. Intravascular Starling forces and extravascular lung water in the adult respiratory distress syndrome. Chest 1985, 87:585–592.
- Bock JC, Lewis FR: Clinical relevance of lung water measurement with the thermal-dye dilution technique. J Surg Res 1990, 48:254–265.
- Wickerts CJ, Jakobsson J, Frostell C, Hedenstierna G: Measurement of extravascular lung water by thermal-dye dilution technique: mechanisms of cardiac output dependence. Intensive Care Med 1990, 16:115–120.
- Fallon KD, Drake RE, Laine GA, Gabel JC: Effect of cardiac output on extravascular lung water estimates made with the Edwards lung water computer. Anesthesiol 1985, 62:505–508.
- Zeravik J, Borg U, Pfeiffer U: Efficacy of pressure support ventilation dependent on extravascular lung water. Chest 1990, 97:1412–1419.
- Haider M, Schad H: Effect of positive end-expiratory airway pressure (PEEP) on extravascular thermal lung water estimation in the dog. In: Practical Applications of Fiberoptics in Critical Care Monitoring. Edited by Lewis F, Pfeiffer U. Berlin: Springer-Verlag, 1990:96–104.