Heart examination
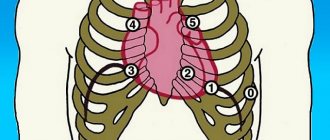
There are 4 points of cardiac auscultation:
- Mitral valve area.
- Aortic valve area.
- Pulmonary valve area.
- Tricuspid valve area.
The heart examination has the following algorithm:
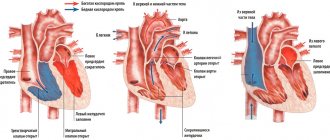
- definition and changes of I, II tones;
- assessment of III and IV tones;
- noise detection;
- listening to three-part rhythms.
Normally, during auscultation of the heart at four points, the doctor hears two abrupt sounds. They are called the first systolic sound, as well as the second diastolic sound. In the presence of pathologies, clicks are heard and rhythm disturbances are observed. If additional sounds of III and IV are heard, which create a gallop rhythm, it means that the myocardium is significantly weakened. This way you can diagnose hypertension, decompensated heart defects, myocarditis and other pathologies.
General listening rules
1. Maintain complete silence in the room where the examination is being carried out.
2. The temperature in the room should be as comfortable as possible for the patient.
3. The area of the body to be auscultated should be bare, as friction from clothing may cause interference.
4. In some cases, the patient's hair may cause interference, so if necessary, moisten it with water, oil or soap solution.
5. The patient must be in the correct position: sitting or standing.
6. Ear olives should fit snugly into the ear canal, but should not cause discomfort.
7. Do not press too hard on the head of the stethoscope, otherwise it may cause pain to the patient.
8. When using a solid stethoscope, do not touch it with your hand to avoid extraneous sounds.
9. Use only one stethoscope.
11. When auscultating the respiratory system, the patient’s breathing should be controlled.
12. When auscultating, do not be distracted, be attentive.
Lung examination
Auscultation of the lungs allows you to determine the type of breathing, detect additional noises and understand when they occur (during inhalation or exhalation). The doctor applies a stethoscope to symmetrical points on the left and right sides of the chest to conduct a comparative diagnosis.
Auscultation of the lungs provides the following algorithm of actions:
- listening from the front in the area of the collarbones with gradual movement down, and then from the back in a similar sequence;
- determination of vesicular and bronchial breathing by listening to points above the larynx and trachea;
- detection of additional sounds in the airways, alveoli or pleura.
When auscultating the points of the lungs, the patient sits or stands. To increase the area of interscapular space for listening, he crosses his arms over his chest. This makes noise detection more efficient. For the most informative auscultation of the lungs (listening for wheezing and clicking), the doctor asks the patient to place his hands behind his head, thereby increasing the area of the axillary zones.
Choosing a Stethoscope
Flexible stethoscope. Such stethoscopes are very convenient for the doctor and the patient. Developed using the latest advanced technologies, the new models significantly enhance sound quality, and the membrane eliminates the feeling of cold in the patient. Disadvantages include the ability to transmit extraneous noise.
A solid stethoscope practically does not change the nature of the sounds heard, however, this type of stethoscope, when pressing on the site of auscultation, can cause pain in the patient.
Abdominal examination
There are 9 points of auscultation of the abdomen:
- 3 epigastric (2 - right and left subcostal zones, 1 - epigastric);
- 3 mesogastric (2 - right and left lateral flanks, 1 - umbilical zone);
- 3 hypogastric (2 - right and left iliac regions, 1 - suprapubic).
During the examination, the patient lies on his back, with his arms and legs extended straight. The doctor is on the right and applies the stethoscope to symmetrical areas of the abdomen in the direction from left to right. Normally, periodic peristalsis is heard. Its pathological strengthening is one of the signs of intestinal obstruction, and its weakening indicates intestinal atony or general peritonitis.
Through points in the abdominal cavity, the renal, iliac, and femoral arteries can be examined. The presence of systolic murmur indicates congenital or acquired narrowing of blood vessels, which is most often observed in atherosclerosis.
2
Auscultation of the lungs. Technique, algorithm
Auscultation of the lungs is a research method based on the perception of sounds naturally occurring in the body through indirect or direct contact of the researcher’s ear with the surface of the body.
Auscultation of the lungs using a simple technique
At the same time, this is a very difficult to interpret research method, which in its significance and value in some cases is not inferior to x-ray examination. Listening requires experience, one must have a correct understanding of the sound impressions perceived by the ear, and most importantly, one must be able to find in these extremely diverse acoustic phenomena a reflection of the pathoanatomical processes taking place in the lungs according to the place of listening.
To correctly understand the auscultated lung sounds, it is necessary to pay attention to their nature, strength, relationship to the phases of breathing (i.e., inhalation and exhalation), localization and distribution. The same with percussion, at the beginning we carry out comparative auscultation. Listening at strictly symmetrical places in the chest, we compare the data obtained. It is necessary to mentally compare inhalation with exhalation on the same side, inhalation with exhalation and exhalation with exhalation on opposite sides.
The patient's position during auscultation, depending on the condition, can be any. However, the most comfortable position will be a standing or sitting position with your hands freely lowered or placed on your knees. You should not listen to severe, weak patients in a standing position; – when breathing deeply, they often experience dizziness and fainting. The most incorrect position is when the patient sits on the bed with his legs extended. The patient should be naked to the waist, as clothing often introduces extraneous sounds. It is necessary to teach the patient to breathe correctly: deeply,
calmly, evenly, through the nose and only at the special request of the doctor - through the mouth at an average pace, i.e. take about 25 breaths per minute.
According to the doctor’s sign, at the end of the exhalation, the patient should, without inhaling, cough briefly vigorously, but silently, only with residual air; Take a deep breath again immediately after coughing.
Failure to follow this rule is a big omission: in almost half of patients with tuberculosis, mild wheezing is heard only after coughing. And a doctor who does not instruct the patient how to breathe does not receive what auscultation can give. Proper installation of the stethoscope is also of great importance. If the stethoscope does not fit tightly to the skin, then you can easily hear noises and wheezing that are not really there.
When listening to the lungs, first of all, you need to listen to breathing sounds, determine the nature of breathing, its intensity, and establish the ratio of inhalation and exhalation.
After this, pay attention to possible side noises or wheezing. When listening to respiratory sounds, breathing through the mouth is undesirable (the patient breathes through the nose), while when wheezing, breathing through the mouth will promote stronger air movement in the bronchi and thereby easier formation, and therefore the perception of wheezing.
Then listen to the friction noise of the pleura, which can most often be heard in the inferolateral parts of the chest, where the excursion of the lungs is small, and, therefore, the conditions for listening to the friction noise are the best.
Finally, the voice is heard. Both loud speech and whispers are heard. Both through a stethoscope and directly by the ear. The order of listening places is the same as for percussion, i.e. apexes, anterior surface (top to bottom), lateral surfaces (from the axillary fossae downwards), posterior surface (above the shoulder blades, between them and under the shoulder blades) in symmetrical places alternately.
The sounds or noises that arise when listening to the respiratory organs are divided into three main groups: 1. Breathing noises. 2. Side noises or wheezing and crepitus. 3. Pleural friction noise.
Auscultation of the lungs. Algorithm
1. Preparation for auscultation, instructing the patient, identifying and eliminating factors that can cause the appearance of auscultation artifacts 2. Strict symmetry of the auscultation points on the right and left. If asymmetry of the main respiratory sounds is detected and the presence of side (localized) respiratory sounds is suspected, proceed to auscultation in zones 3. Determination of the presence (or absence) and differentiation of the main respiratory sounds A. Determination of the time ratio of the inhalation and exhalation phases B. Determination of the qualitative characteristics of the main respiratory sounds noise
| Vesicular a) Predominance of the inhalation phase over the exhalation phase (3: 1) b) Qualitatively resembles the sound “f” pronounced on exhalation c) Relatively soft | Bronchial a) The inhalation and exhalation phases are equal in duration and exhalation is somewhat predominant b) Qualitatively resembles the sound “x” c) Coarser d) As a rule, determined locally or unilaterally |
4. Assessment of the nature and changes in vesicular respiration a) Physiological vesicular respiration (puerile) b) Pathological vesicular respiration and its characteristics A. Symmetry 1. Its total change 2. Unilateral 3. Local B. Increased vesicular respiration (hard, rough) C. Weakening of vesicular respiration D. Saccaded vesicular respiration E. Unilateral (local) disappearance of vesicular respiration
5. Assessing the nature and changes in bronchial breathing a) Physiological (above the trachea and larynx) b) pathological - in the area where vesicular breathing is supposed to be heard A. Localization (one-sided, local) B. Volume 1. Normal 2. Loud (metallic) 3. Quiet (compressive stelectasis) B. Rare variants (amphoric)
6. Determination of the presence of adverse respiratory sounds A. Over the entire surface of the lungs B. Unilateral C. Local
7. Based on qualitative characteristics (duration, pitch, timbre, stability) and additional auscultatory techniques (forced breathing, coughing, tension and relaxation of the abdominal muscles with the upper respiratory tract closed), a specific respiratory noise is determined
8. Wheezing A. Timbre B. Pitch C. Duration Wet / Dry Small bubbles / Medium bubbles / Large bubbles Whistling / Humming Oral (bubbling breathing) / Oral (rooster crowing)
9. Crepitus Differentiated from fine-bubbly moist rales In contrast to them a) Does not change the caliber (only volume) b) Qualitatively resembles the crackling sound of hair when rubbed near the ear With pleuropneumonia: a) Initial b) Terminal
10. Pleural friction noise Differentiates from dry rales, in contrast to them a) It is heard as if “closer” to the ear b) Does not change in pitch after coughing c) Changes in volume when the phonendoscope is pressed on the chest d) Is usually accompanied by a typical pain syndrome Qualitatively reminiscent crunching snow, creaking door hinge
11. Rare auscultatory symptoms a) Noise of a “falling drop” b) Splashing noise
12. Assessment of the relationship between the main and secondary respiratory sounds 13. Assessment of the relationship of auscultatory symptoms with data obtained by other methods of studying the respiratory system.
Auscultation. Methods, rules
Auscultation (auscultare - listen, listen) is a method of research using the perception of sounds that naturally occur in the body, which are perceived through direct or indirect - with the help of some solid body - contact of our ear with the surface of the body. Listening to voices, coughing, sneezing, loud breathing, wheezing, rumbling in the intestines and other sounds heard at a distance does not apply to the auscultation method.
Auscultation. History of origin
Listening to sounds occurring inside our body was used for diagnostic purposes in ancient times. Thus, in the writings of Hippocrates there are references to the friction noise of the pleura, the sound of splashing in the pleural cavity, and moist rales in the lungs. At the beginning of our era, they undoubtedly knew how to listen to heart sounds. But then, for one and a half thousand years, listening did not play a role in the study of patients.
Listening became a diagnostic method only thanks to the French scientist Rene Laennec (1781-1826), who was a talented clinician, pathologist and teacher at a medical school in Paris.
In Russia, the development of the auscultation method is associated with the names of P.A. Charukovsky and M.Ya. Mudrova. The talented Russian professor Grigory Ivanovich Sokolsky, whose name is associated with the doctrine of rheumatism (Buyo-Sokolsky disease) in his works “On the study of diseases with hearing and a stethoscope” and “The doctrine of chest diseases”, described in detail the auscultatory phenomena heard in heart defects and respiratory diseases .
Auscultation deals with very faint sounds from our body that travel little or nothing through the air. Therefore, if there is at least the thinnest layer of air between the ear and the surface of the body, we do not hear sounds, but begin to perceive them as soon as a continuous communication through the solid body is established between the ear and the sounding body. This is achieved either by direct contact of the ear, for example, with the chest, or by connecting them with some kind of solid body capable of conducting vibrations (a stethoscope). On the same basis, the already inaudible tone of a tuning fork placed in front of the ear is again perceived well and for a long time if the tuning fork is placed on the head. Thus, it was proven that sound conduction in stethoscopes occurs not through the column of air inside them, but along their walls.
The name stethoscope was given by Laennec. His stethoscope originally resembled a paper parcel. It was a hollow wooden tube 33 cm long with the same diameter throughout, which was disassembled in the middle. Modifications to this original form went in different directions: thinning the tube, shortening it, making the ear end more convenient, and using various materials for making the tube.
The stethoscope is a cylindrical tube. In most cases, its wide part is funnel-shaped and is applied to the auricle, and the narrower part, the so-called bell of the stethoscope, is applied to the patient’s body. Stethoscopes are made from various materials: wood, metal, ivory, plastic. Subsequently, instead of rigid stethoscopes, flexible ones were proposed, first recommended by N.F. Filatov. In this case, two rubber tubes come from the bell of a conventional stethoscope, the ends of which are inserted into the researcher’s ears. Finally, the latest modifications of the stethoscope concerning its thoracic end were expressed in the addition of a device for resonance to it in order to enhance sound phenomena. This is how various forms of phonendoscopes arose. First, simple ones, when the chest end of the stethoscope was covered with a rubber membrane, and more complex, when the end part of the phonendoscope was a metal cavity covered with a membrane. Sound phenomena arising in a particular organ are transmitted to the membrane, which vibrates. The cavity covered with this membrane, according to the theory of resonance, amplifies the sound. Sometimes a multiphonendoscope is used in classes with students.
In principle, the term stethoscope given by Laennec does not accurately reflect the purpose of this device, since it comes from two words - stethos - chest and scopeo - look. The advantage of flexible stethoscopes is twofold: convenience of examination for the doctor and the patient and a more significant amplification of sound. They almost do not change the nature of natural sounds and produce little side noise. The disadvantage is a significant change in the natural character of sounds and a large number of easily occurring extraneous noises. They are inconvenient for the doctor and the patient and their use is tedious.
Auscultation of the lungs. Theory
Auscultation, as a research method, deals with very faint sounds from our body, which have very little or no propagation in the air.
We can perceive such sounds under the condition of continuous communication through a solid body between the ear and the sounding body. This is achieved either by direct contact of the ear, for example, with the chest, or by connecting them (the ear and the sounding body) with some kind of solid body capable of conducting vibrations (a stethoscope). If there is at least the thinnest layer of air between the ear and the surface of the body, we do not hear sounds. From this it is clear that in stethoscopes of any design, sound is transmitted not through the column of air inside them, but along their walls, just as in
In our ear, sound vibrations are conducted not through the air of the ear canal, but through the auricle, the wall of the ear canal, the eardrum, etc.
Full stethoscopes are preferred not because they conduct sounds through the air of their canal, but because they are lighter and more capable of vibration.
To maintain the maximum ability of the stethoscope to vibrate, you need to apply it to the body as lightly as possible and not touch it with your hand while listening. The size of the funnel of the chest part of the stethoscope matters: the narrower it is, the more accurately it is possible to localize the sounds being heard, but they are collected from a smaller surface and, therefore, weaker. The wider the funnel, the weaker sounds can be perceived.
Auscultation. Methods
In general, what matters is not the choice of stethoscope or phonendoscope, not the method of listening, but the ability to auscultate. You should always use the same device, since each stethoscope and phonendoscope has its own individual characteristics.
There are two main methods of auscultation:
- A method of immediate or direct auscultation, in which listening is performed directly with the ear attached to the patient’s body. This method is still widespread in France, the homeland of Laennec, the founder of mediocre auscultation. French doctors usually use direct auscultation through a thin cloth.
- The method of mediocre, indirect or instrumental auscultation is carried out using a stethoscope or phonendoscope.
| Advantages | Flaws | |
| Method of immediate or direct auscultation | – large surface of perception – natural character of the sounds heard | – localization of sounds is difficult, especially when listening to the heart; impossibility of use in some parts of the body (in the supraclavicular and axillary fossae); unhygienic, dangerous for infectious diseases. |
| Method of mediocre, indirect or instrumental auscultation | – the ability to localize sounds anywhere in the body and in any position of the patient, which is especially important in seriously ill patients – the hygiene of the method. | – smaller surface of perception – changed nature of sounds heard |
Auscultation. Choosing a Stethoscope Solid Stethoscopes
Advantages: they change little the character of natural sounds, produce little side noise, and at the same time convey tactile sensations along with sounds.
Flaws. The examination is inconvenient and tedious for the doctor and the patient, painful when pressed.
Flexible stethoscopes
Advantages: ease of examination for the doctor and the patient, the ability to see his facial expression and significant amplification of sound.
Flaws. Significant change in the natural character of sounds. For beginners in auscultation, it is better to use a stethoscope, and it makes no difference which is better - hard or soft. It is not the method or method of auscultation that decides the matter, but the ability to auscultate.
Auscultation. Rules
- Auscultation is carried out in a warm room; it is necessary that silence be maintained, since the appearance of muscle tremors will interfere with auscultation.
- The patient's body should be bare, as friction of clothing can cause collateral noise.
- You should pay attention to the hair on the body, since the friction of the instrument against the hair imitates typical pathological auscultatory phenomena. Moisten or soap the hair at the listening site to avoid unwanted noise.
- The bell of a stethoscope or phonendoscope should be tightly, but not tightly applied to the listening surface (apply evenly, tightly, but lightly to the listening surface).
- The position of the doctor and the patient should be comfortable.
- It is better not to touch the solid stethoscope with your hand while listening to avoid unwanted sounds and a decrease in sound conductivity.
- When listening to a patient in a standing or sitting position, the doctor should clasp (hug) the patient with his free hand so that they form a single whole.
- Do not press the stethoscope so as not to cause pain to the patient.
- Use the same stethoscope whenever possible.
- When listening to the respiratory system, control the breathing of the subject.
- Listen systematically and persistently.
You need to get used to being distracted from everything around you. For this purpose, it is useful to close your eyes and plug your free ear when listening (to eliminate unnecessary sound and visual irritation).
Usually comparative auscultation is performed, in which the listening order is the same as for comparative percussion.
Listen in symmetrical areas and alternately on one side or the other, comparing each time the auscultation data in the following order: apexes, anterior surface of the lungs from top to bottom in symmetrical areas, lateral surfaces (from the axillary fossae downwards, preferably with arms thrown behind the head) , posterior surface in the supra-, inter- and subscapular areas.
First, they listen to breathing sounds, which are called basic, that is, they determine the nature of breathing, its intensity, the ratio of inhalation and exhalation. Then they pay attention to side noises or wheezing, crepitus, pleural friction noise, and then listen to the voice.
Auscultation of the lungs
Auscultation of the lungs is performed according to a certain plan: first in front and above, moving down and to the sides. Then in the same sequence - from behind and along the side lines.
Places for listening to the lungs: a—in front; b - behind
Auscultation determines the nature of respiratory sounds that form auscultatory types of breathing:
vesicular - inhalation and ]/3 exhalation are heard in the form of the sound “f”; hard (puerile in children under six years of age) _ both inhalation and exhalation can be heard with the sound “f”; bronchial - you can hear inhalation and exhalation with the sound “x”; amphoric - inhalation is similar to the sound produced by forcefully blowing air into the narrow neck of an empty glass vessel. Indicates the presence of a smooth-walled cavity in the lung (abscess, Glossary Link cavity); saccaded - inhalation consists of two or more phases. It happens when there is a tumor or foreign body in the trachea or large bronchus. Normally, vesicular breathing is heard below the angles of the scapula in the back, on the lateral surfaces of the chest and in front below the 2nd rib and lateral periosternal lines; bronchial - in the interscapular space and behind the sternum - in front.
Types of breathing:
o - vesicular; 6 - weakened vesicular; c - enhanced vesicular; g - bronchial; d — weakened bronchial; e - enhanced bronchial; g - bronchovesicular; z - saccade
Adverse breath sounds:
crepitus - a small crackling sound when inhaling, evidence of pathology in the alveoli; pleural friction noise - inhalation and exhalation are similar to the crunch of snow underfoot or the friction of two sheets of paper - evidence of pathology of the pleural layers (they have become rough). The pleural friction noise is sometimes similar to crepitus or moist fine bubbling rales.
Features:
after coughing, wheezing changes its character or disappears; with strong pressure on the chest with a stethoscope, the pleural friction noise intensifies (wheezing does not); crepitus is heard only during the inhalation phase, and wheezing and pleural friction noise are heard in both phases of breathing; with the mouth and nose closed and the abdomen moving, the pleural friction noise is heard, but wheezing and crepitus are not; wheezing: dry - whistling, wheezing, buzzing - occurs in the bronchi due to narrowing of their lumen or due to the accumulation of viscous sputum; wet - small, medium, large bubbles, reminiscent of the sound of bursting air bubbles passed through water. They occur in the bronchi of the appropriate caliber when liquid sputum accumulates in them.
What is lung auscultation?
Auscultation is a method based on listening to changes in sounds that occur during the functioning of internal organs and systems. In the case of respiratory dysfunction, the doctor assesses the nature of the functioning of the lungs and bronchi.
A technique for studying breathing in a similar way was developed during the time of Hippocrates (IV-III centuries BC). To diagnose respiratory pathology, the doctor, during a standard examination of the patient, put his ear to the chest and listened for any extraneous or altered sounds.
The described method is called direct auscultation. In modern medicine, in 99% of cases an indirect version of the technique is used. Doctors use special instruments to auscultate the lungs - phonendoscopes (stethoscopes).
The device consists of a membrane and/or funnel that fits tightly against the area of the body being examined. The latter is connected by tubes (sound ducts) with rigid arms ending in ear olives. Due to the concentration of sound from the focus being studied, the doctor clearly hears what is happening under the membrane.
Auscultation of the lungs should be performed in all patients suffering from some form of respiratory pathology. The diagnostic method is simple, does not require the use of additional equipment and remains the basis for the initial assessment of the patient’s lung condition.
Auscultation of the lungs in children
Auscultation of the lungs in children is an important diagnostic method that allows us to identify pathology of the respiratory system in young patients. The examination technology coincides with the principle of the procedure in adults.
Features of lung auscultation in children:
- The need to use smaller membranes or funnels;
- Poor development of the chest muscles, which leads to a significant increase in breathing sounds. This type of breathing is called puerile;
- The need for more careful control of the temperature of the phonendoscope applied to the child’s skin. Children react negatively to the touch of a membrane or funnel that is too cold.
The sequence of points and the principles of the procedure described above are relevant for small patients. Using auscultation, the presence and nature of wheezing, the localization of the inflammatory process, and the progression of organic or functional changes in the bronchopulmonary system are recorded.
Important! When using auscultation in children, the doctor always remembers that young patients are rarely distinguished by patience. Therefore, experienced pediatricians carry out diagnostics quickly, trying to turn the examination into a game.
Sometimes, for high-quality auscultation in a restless child, the doctor needs 2-3 attempts. Otherwise, the information obtained remains unreliable and may affect the choice of treatment method.
What you need to know and possible consequences
Auscultation of the lungs is the generally accepted standard for diagnosing diseases of the respiratory system. The procedure is safe for the patient. During the examination, the person does not feel any discomfort except for the touch of a cool phonendoscope. The duration of the examination depends on the severity of the pathology. On average, a doctor needs 2-5 minutes to fully carry out the corresponding procedure.
Undesirable consequences of auscultation are a myth. It is extremely difficult to harm a patient using the appropriate technique.
For what diseases
Over two thousand years of history of listening to the lungs, doctors have accumulated experience in diagnosing various diseases “by ear”. At medical universities, young doctors are taught how to recognize this or that pathology using a phonendoscope.
Diseases that are diagnosed using auscultation:
- Acute or chronic bronchitis;
- Pneumonia. Pneumonia is a serious pathology that changes the function of the relevant organs. Auscultation of the lungs during pneumonia is a method used additionally to monitor the quality of therapy;
- Bronchial asthma;
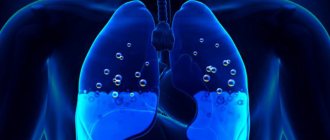
- Hydro- or pneumothorax - accumulation of fluid or air in the pleural cavity;
- Acute pulmonary edema is stagnation of blood in the tissues of the corresponding organ.
Using the described technique, tuberculosis or lung cancer can be suspected. However, these diagnoses cannot be established without the use of auxiliary methods.
Important! Auscultation is the primary diagnostic method, allowing the doctor to get a general picture of pulmonary dysfunction. To clarify the cause of the symptoms characteristic of a particular case, additional procedures are required. Otherwise, important details that affect the patient's outcome may be missed.
Additional breath sounds
The noises described above are the main ones. In addition to bronchial and vesicular breathing, additional sound phenomena can be recorded during auscultation, which affect the understanding of the pathology developing in the patient’s lungs.
Wheezing
Wheezing is an auxiliary breathing noise associated with the passage of air masses through the respiratory tract, in which additional obstacles are formed (sputum, pus, blood). During contact with a liquid, turbulence of the gas mixture occurs, which leads to the appearance of a corresponding phenomenon.
Wheezing occurs:
- dry;
- wet;
- mixed.
Dry wheezing is formed when the airways are blocked by thick and viscous mucus. Depending on the diameter of the section of the respiratory tract where the block occurs, the height, timbre and duration of the corresponding phenomenon changes. There are buzzing, whistling wheezing sounds. The latter are more common and are characteristic of bronchial asthma.
Moist rales differ in the mechanism of their occurrence. For the corresponding sound to appear, air must pass through a liquid medium with the formation of bubbles, which, when bursting, provide the appearance of the described phenomenon. Depending on the localization of the pathological process and the diameter of the area of the affected respiratory tract, wheezing can be small-, medium- and large-bubble. The cause of this sound is the accumulation of blood, pus, and liquid sputum in the bronchi.
Crepitus
Crepitation is a sound characteristic of the early and late stages of pneumonia. Unlike moist rales, the pathogenetic basis for the appearance of noise remains the penetration of fluid into the cavity of the alveoli. During exhalation, the corresponding structures decrease in size. The liquid envelops the walls of the bubbles, which leads to sticking together. During inhalation, air fills the alveoli, which is accompanied by the walls peeling off with a characteristic click.
This sound occurs simultaneously in all bubbles, which creates a corresponding auscultatory picture that resembles rubbing hair near the ear.
A characteristic feature of crepitus remains the need for deep inspiration to straighten the alveoli. With shallow breathing, the phenomenon is not recorded. Therefore, for differential diagnosis of early and late stages of pneumonia, it is imperative to ask the patient to breathe deeply.
Crepitus additionally occurs in all lung diseases that are accompanied by the penetration of fluid into the respiratory vesicles.
Pleural friction rub
Pleural friction noise is a pathological phenomenon that is not associated with dysfunction of the lung tissue specifically. The source of the problem becomes the pleural cavity, the visceral and parietal layer of the corresponding connective tissue structure. Normally, all of these elements are smooth and elastic.
In the presence of an inflammatory or infectious process, partial leakage of plasma into the specified space is observed. Quite quickly, excess liquid is absorbed back into the vessels, however, the dry part in the form of fibrin remains.
The result is the deposition of hard fibers on the surface of the pleura. During the next respiratory movements during auscultation, the doctor records noise that occurs due to friction of fibrin conglomerates. The sound phenomenon resembles the rustling of snow underfoot. The typical cause is dry (fibrinous) pleurisy.
At the same time, the patient is worried about increased body temperature, chest pain, and discomfort during deep breathing.
The pleural friction noise resembles crepitus or moist rales. For differential diagnosis, the patient is asked to close his mouth and nose with his hands and imitate the respiratory movements of the chest.
If the noise remains, then the pleura is affected. With wheezing and crepitus, the connection with the air flow is always maintained. Additionally, you can ask the patient to cough. Wheezing and crepitus change their character after the appropriate test, which is not typical for pleural friction noise.