© Author: Balandina Anna Borisovna, doctor of the therapeutic department, especially for SosudInfo.ru (about the authors)
Everyone is familiar with the sacred act of a doctor at the time of examining a patient, which is scientifically called auscultation. The doctor applies a phonendoscope membrane to the chest and listens carefully to the work of the heart. What he hears and what special knowledge he has in order to understand what he hears will be discussed below.
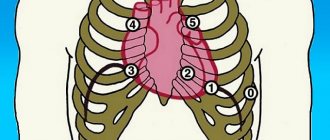
Heart sounds are sound waves produced by the heart muscle and heart valves. They can be heard if you apply a stethoscope or ear to the anterior chest wall. To obtain more detailed information, the doctor listens to sounds at special points near the heart valves.
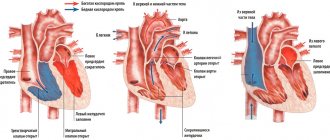
Cardiac cycle
All structures of the heart work in concert and sequentially to ensure efficient blood flow. The duration of one cycle at rest (that is, at 60 beats per minute) is 0.9 seconds. It consists of a contractile phase - systole and a relaxation phase of the myocardium - diastole.
diagram: cardiac cycle
While the heart muscle is relaxed, the pressure in the chambers of the heart is lower than in the vascular bed and blood passively flows into the atria, then into the ventricles. When the latter are filled to ¾ of their volume, the atria contract and forcefully push the remaining volume into them. This process is called atrial systole . Fluid pressure in the ventricles begins to exceed the pressure in the atria, causing the atrioventricular valves to slam shut and separate the cavities from each other.
Blood stretches the muscle fibers of the ventricles, to which they respond with a rapid and powerful contraction - ventricular systole . The pressure in them quickly increases and at the moment when it begins to exceed the pressure in the vascular bed, the valves of the latter aorta and pulmonary trunk open. Blood rushes into the vessels, the ventricles empty and relax. High pressure in the aorta and pulmonary trunk closes the semilunar valves, so fluid does not flow back into the heart.
The systolic phase is followed by complete relaxation of all cavities of the heart - diastole , after which the next stage of filling begins and the cardiac cycle repeats. Diastole is twice as long as systole, so the heart muscle has sufficient time to rest and recover.
Formation of tones
The stretching and contraction of myocardial fibers, the movement of valve flaps and the sound effects of a blood stream give rise to sound vibrations that are picked up by the human ear. Thus, 4 tones are distinguished:
1 heart sound appears during contraction of the heart muscle. It consists of:
- Vibrations of tense myocardial fibers;
- Noise of collapse of the atrioventricular valves;
- Vibrations of the walls of the aorta and pulmonary trunk under the pressure of incoming blood.
Normally, it dominates at the apex of the heart, which corresponds to a point in the 4th intercostal space on the left. Listening to the first tone coincides in time with the appearance of a pulse wave in the carotid artery.
The 2nd heart sound appears a short period of time after the first. It is made up of:
- Collapse of the aortic valve leaflets:
- Collapse of the pulmonary valve flaps.
It is less sonorous than the first and prevails in the 2nd intercostal space on the right and left. The pause after the second sound is longer than after the first, since it corresponds to diastole.
3 heart sound is not obligatory; normally it may be absent. It is born by vibrations of the walls of the ventricles at the moment when they are passively filled with blood. To detect it with the ear, you need sufficient experience in auscultation, a quiet examination room and a thin anterior wall of the chest cavity (which is common in children, adolescents and asthenic adults).
4 heart tone is also optional; its absence is not considered a pathology. It appears at the time of atrial systole, when the ventricles are actively filling with blood. The fourth tone is best heard in children and slender young people whose chest is thin and the heart fits tightly to it.
cardiac auscultation points
Normally, heart sounds are rhythmic, that is, they occur after equal periods of time. For example, with a heart rate of 60 per minute, 0.3 seconds pass after the first sound until the start of the second, and 0.6 seconds after the second until the next first. Each of them is clearly distinguishable by ear, that is, the heart sounds are clear and loud. The first tone is quite low, long, sonorous and begins after a relatively long pause. The second tone is higher, shorter and occurs after a short period of silence. The third and fourth sounds are heard after the second - in the diastolic phase of the cardiac cycle.
Video: Heart Sounds – Training Video
Quiet pulmonary component of the second tone
The pulmonary component of the second sound may be quite quiet and normal. On inhalation, it may not be heard at all, creating the false impression of a paradoxical splitting of the second tone. This is due to the distance of the heart from the surface of the chest due to an increase in lung volume. However, in most cases the components of the second tone can be distinguished. The pulmonary component of the second tone is weakened in pulmonary stenosis. It is also significantly attenuated, usually to the point of complete absence, in tetralogy of Fallot, pulmonary atresia, and transposition of the great vessels.
Changes in tones
Heart sounds are essentially sound waves, so their changes occur when the conduction of sound is disrupted and the structures that produce these sounds are pathological. There are two main groups of reasons why heart sounds sound different from the norm:
- Physiological – they are related to the characteristics of the person being studied and his functional state. For example, excess subcutaneous fat near the pericardium and on the anterior chest wall in obese people impairs sound conduction, so heart sounds become muffled.
- Pathological - they occur when the structures of the heart and the vessels extending from it are damaged. Thus, narrowing of the atrioventricular opening and compaction of its valves leads to the appearance of a clicking first tone. When they collapse, dense sashes produce a louder sound than normal, elastic ones.
Heart sounds are called muffled when they lose their clarity and become difficult to distinguish. Weak dull tones at all points of auscultation suggest:
changes in heart sounds characteristic of certain disorders
- Diffuse damage to the myocardium with a decrease in its ability to contract - extensive myocardial infarction, myocarditis, atherosclerotic cardiosclerosis;
- Effusion pericarditis;
- Deterioration of sound conduction for reasons not related to the heart - emphysema, pneumothorax.
The weakening of one tone at any point of auscultation gives a fairly accurate description of changes in the heart:
- Muffling of the first tone at the apex of the heart indicates myocarditis, sclerosis of the heart muscle, partial destruction or insufficiency of the atrioventricular valves;
- Muffling of the second tone in the 2nd intercostal space on the right occurs with insufficiency of the aortic valve or narrowing (stenosis) of its mouth;
- Muffling of the second tone in the 2nd intercostal space on the left indicates insufficiency of the pulmonary valve or stenosis of its mouth.
In some diseases, changes in heart sounds are so specific that they receive a separate name. Thus, mitral stenosis is characterized by a “quail rhythm”: the clapping first tone is replaced by an unchanged second tone, after which an echo of the first appears - an additional pathological tone. A three- or four-part “gallop rhythm” occurs with severe myocardial damage. In this case, the blood quickly stretches the thinned walls of the ventricle and their vibrations give rise to an additional tone.
An increase in all heart sounds at all points of auscultation occurs in children and asthenic people, since their anterior chest wall is thin and the heart lies quite close to the phonendoscope membrane. The pathology is characterized by an increase in the volume of individual tones in a certain location:
- A loud first sound at the apex occurs with narrowing of the left atrioventricular orifice, sclerosis of the mitral valve leaflets, tachycardia;
- A loud second sound in the 2nd intercostal space on the left indicates an increase in pressure in the pulmonary circulation, which leads to stronger collapse of the pulmonary valve leaflets;
- A loud second sound in the 2nd intercostal space on the left indicates increased pressure in the aorta, atherosclerosis, and hardening of the aortic wall.
Arrhythmic tones indicate a disturbance in the conduction system of the heart. Heart contractions occur at different intervals, since not every electrical signal passes through the entire thickness of the myocardium. Severe atrioventricular block, in which the work of the atria is not coordinated with the work of the ventricles, leads to the appearance of a “gun tone”. It is caused by a simultaneous contraction of all chambers of the heart.
Double tone is the replacement of one long sound with two short ones. It is associated with desynchronization of the valves and myocardium. The splitting of the first tone occurs due to:
- Non-simultaneous closure of the mitral and tricuspid valves with mitral/tricuspid stenosis;
- Disturbances in the electrical conductivity of the myocardium, due to which the atria and ventricles contract at different times.
The bifurcation of the second tone is associated with a discrepancy in the time of collapse of the aortic and pulmonary valves, which indicates:
- Excessive pressure in the pulmonary circulation;
- Arterial hypertension;
- Left ventricular hypertrophy with mitral stenosis, due to which its systole ends later and the aortic valve closes late.
With ischemic heart disease, changes in heart sounds depend on the stage of the disease and the changes that have occurred in the myocardium. At the onset of the disease, pathological changes are mild and heart sounds remain normal during the interictal period. During an attack, they become muffled, irregular, and a “gallop rhythm” may appear. The progression of the disease leads to persistent myocardial dysfunction with the preservation of the described changes even outside of an angina attack.
It should be remembered that a change in the nature of heart sounds does not always indicate pathology of the cardiovascular system. Fever, thyrotoxicosis, diphtheria and many other causes lead to changes in heart rhythm, the appearance of additional tones or their muffling. Therefore, the doctor interprets auscultatory data in the context of the entire clinical picture, which makes it possible to most accurately determine the nature of the emerging pathology.
Question 4. Reasons for weakening and strengthening (emphasis) of tone II
Weakening of the second tone
is recognized in the presence of such a symptom as a decrease in the sound of tone II in comparison with tone I, or with the same degree of sonority of both tones at the base of the heart (the place of auscultation of the aorta and pulmonary artery).
Weakening of the II tone over the aorta is very characteristic of heart disease - aortic valve insufficiency. The cause of aortic regurgitation syndrome is the complete or partial destruction of the valve leaflets, their scarring and reduction in area.
In the absence of the valve's obturator function, blood flows back through the gap (regurgitates) from the aorta into the left ventricle. A decrease in the area of the valve leaflets and the absence of a push of blood onto the leaflets leads to a decrease in the sonority of the second tone in the aorta.
If the valves are completely destroyed, the second sound in the aorta may not be heard at all.
Weakening of the II tone on the pulmonary artery occurs with rather rare valvular heart defects: insufficiency of the pulmonary artery valve and narrowing of its mouth. The mechanism for weakening the tone in these cases is the same conditions as for similar aortic defects.
Strengthening, emphasis
of the second tone
. Normally, in adults, when listening and comparing the second tone in the aorta and pulmonary artery, it is noted that their volume is the same.
This is explained by the fact that the pulmonary valve is located closer to the chest than the aortic valve, due to which the transmission of sound phenomena from them is equalized, although greater blood pressure in the aorta also produces a greater push force on the aortic valve leaflets when they close.
In children and young people, tone II on the pulmonary artery is often stronger than on the aorta - the emphasis of tone II on the pulmonary artery. This is explained by the fact that the pressure in the aorta in children is lower than in adults, and the pulmonary artery is located closer to the anterior wall of the chest (site of auscultation).
Under certain pathological conditions, the volume of tone II in the aorta and pulmonary artery becomes unequal. In cases where the II tone on the aorta significantly prevails over the I tone, and, in addition, becomes louder than the II tone of the pulmonary artery, they say that the II tone on the aorta is intensified and emphasized.
Since the volume of the second tone depends on the force of the blood impulse of the aortic or pulmonary artery valves at the beginning of diastole, it increases in parallel with the increase in blood pressure in the vessels.
An emphasis on the second tone on the aorta is observed in arterial hypertension and hypertension.
The emphasis of tone II on the pulmonary artery is observed with hypertension in the pulmonary artery and high pressure in the pulmonary circulation, for example, with mitral heart defects, when there is stagnation of blood in the pulmonary circulation.
The audible accent of the second tone on the aorta in patients without arterial hypertension may indicate atherosclerosis of the aorta, when the dilated aorta and its thickened wall better conduct sounds to the point of auscultation. In the latter case, the sound of tone II may acquire a metallic tint.
Question 5. Splitting, splitting of heart sounds
Double tones are a condition when, during auscultation of the heart, instead of one continuous sound, two sounds are heard following each other after a short period of time. If the time interval between these two sounds is very small and there is no complete impression of the separateness of the sounds, then they talk about splitting the tone. This condition can occur in both I and II.
Splitting (incomplete separation) and bifurcation (complete separation) of both I and II tones can be physiological, i.e., found in completely healthy people, or pathological, observed in certain heart diseases. Physiological separation of tones is more common in young people and is usually associated with sexual intercourse breathing, therefore it is inconsistent.
The splitting and bifurcation of the I tone is caused by the non-simultaneous closure of the mitral and tricuspid valves.
In healthy people, this phenomenon can sometimes appear during exhalation, when, due to increased pressure in the chest, more blood enters the left parts of the heart than the right, which causes asynchronous closure with faster closure of the mitral valve. Therefore, the sound phenomena of the valvular component of the AV valves are perceived separately during exhalation, while during inhalation the tone is heard as one sound.
Splitting or bifurcation of the I tone in pathological conditions is especially characteristic of blockade of one of the branches of the His bundle, when excitation to one of the ventricles arrives late, which means that the mechanical process of contraction of the ventricles begins later. The atrioventricular valve of the “blocked” ventricle lags behind in closing. This separation of tone does not depend on the phases of breathing - it is constant.
Separation II tone is heard more often on the pulmonary artery. It is explained by the non-simultaneous closure of the aortic and pulmonary artery valves.
Under physiological conditions, this phenomenon occurs and is more pronounced during inspiration, when, with a decrease in intrathoracic pressure, the suction effect of the chest causes a slightly larger volume of blood to pass through the right than the left parts of the heart.
In such a situation, systolic emptying of the right ventricle requires more time than the left. Therefore, the pulmonary component of the second tone lags significantly behind the aortic component. This is the mechanism of splitting and bifurcation of the second tone, which is heard during inspiration, especially with deep breathing.
In patients with increased blood pressure in the pulmonary circulation (mitral heart defects, pulmonary hypertension, thromboembolism of the branches of the pulmonary artery), the duration of systole of the right ventricle, in comparison with the left, also increases, which causes a significant lag of the pulmonary component of the second tone from the aortic component. This is the most common mechanism of splitting and bifurcation of tone II.
In patients with bundle branch block, especially the right bundle branch, splitting of the second tone is also possible due to the asynchronism of the end of systole of the right and left ventricles.
With right bundle branch block, the onset of right ventricular diastole, manifested by the pulmonary component of tone II, occurs significantly later than the onset of left ventricular diastole.
Moreover, with such a pathology, both heart sounds may be split.
“Three-member rhythms” associated with the appearance of additional diastolic or systolic tones should be distinguished from bifurcation of heart sounds.
Source: //studfile.net/preview/536935/page:25/