© Author: Balandina Anna Borisovna, doctor of the therapeutic department, especially for SosudInfo.ru (about the authors)
Everyone is familiar with the sacred act of a doctor at the time of examining a patient, which is scientifically called auscultation. The doctor applies a phonendoscope membrane to the chest and listens carefully to the work of the heart. What he hears and what special knowledge he has in order to understand what he hears will be discussed below.
Heart sounds are sound waves produced by the heart muscle and heart valves. They can be heard if you apply a stethoscope or ear to the anterior chest wall. To obtain more detailed information, the doctor listens to sounds at special points near the heart valves.
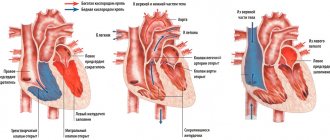
Cardiac cycle
All structures of the heart work in concert and sequentially to ensure efficient blood flow. The duration of one cycle at rest (that is, at 60 beats per minute) is 0.9 seconds. It consists of a contractile phase - systole and a relaxation phase of the myocardium - diastole.
diagram: cardiac cycle
While the heart muscle is relaxed, the pressure in the chambers of the heart is lower than in the vascular bed and blood passively flows into the atria, then into the ventricles. When the latter are filled to ¾ of their volume, the atria contract and forcefully push the remaining volume into them. This process is called atrial systole . Fluid pressure in the ventricles begins to exceed the pressure in the atria, causing the atrioventricular valves to slam shut and separate the cavities from each other.
Blood stretches the muscle fibers of the ventricles, to which they respond with a rapid and powerful contraction - ventricular systole . The pressure in them quickly increases and at the moment when it begins to exceed the pressure in the vascular bed, the valves of the latter aorta and pulmonary trunk open. Blood rushes into the vessels, the ventricles empty and relax. High pressure in the aorta and pulmonary trunk closes the semilunar valves, so fluid does not flow back into the heart.
The systolic phase is followed by complete relaxation of all cavities of the heart - diastole , after which the next stage of filling begins and the cardiac cycle repeats. Diastole is twice as long as systole, so the heart muscle has sufficient time to rest and recover.
Formation of tones
The stretching and contraction of myocardial fibers, the movement of valve flaps and the sound effects of a blood stream give rise to sound vibrations that are picked up by the human ear. Thus, 4 tones are distinguished:
1 heart sound appears during contraction of the heart muscle. It consists of:
- Vibrations of tense myocardial fibers;
- Noise of collapse of the atrioventricular valves;
- Vibrations of the walls of the aorta and pulmonary trunk under the pressure of incoming blood.
Normally, it dominates at the apex of the heart, which corresponds to a point in the 4th intercostal space on the left. Listening to the first tone coincides in time with the appearance of a pulse wave in the carotid artery.
The 2nd heart sound appears a short period of time after the first. It is made up of:
- Collapse of the aortic valve leaflets:
- Collapse of the pulmonary valve flaps.
It is less sonorous than the first and prevails in the 2nd intercostal space on the right and left. The pause after the second sound is longer than after the first, since it corresponds to diastole.
3 heart sound is not obligatory; normally it may be absent. It is born by vibrations of the walls of the ventricles at the moment when they are passively filled with blood. To detect it with the ear, you need sufficient experience in auscultation, a quiet examination room and a thin anterior wall of the chest cavity (which is common in children, adolescents and asthenic adults).
4 heart tone is also optional; its absence is not considered a pathology. It appears at the time of atrial systole, when the ventricles are actively filling with blood. The fourth tone is best heard in children and slender young people whose chest is thin and the heart fits tightly to it.
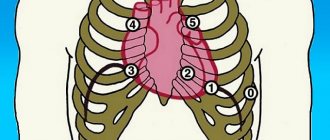
cardiac auscultation points
Normally, heart sounds are rhythmic, that is, they occur after equal periods of time. For example, with a heart rate of 60 per minute, 0.3 seconds pass after the first sound until the start of the second, and 0.6 seconds after the second until the next first. Each of them is clearly distinguishable by ear, that is, the heart sounds are clear and loud. The first tone is quite low, long, sonorous and begins after a relatively long pause. The second tone is higher, shorter and occurs after a short period of silence. The third and fourth sounds are heard after the second - in the diastolic phase of the cardiac cycle.
Video: Heart Sounds – Training Video
Characteristics of heart sounds
HEART SOUND
Auscultation of the heart and great vessels
carried out to identify and analyze sound vibrations resulting from the work of the heart. Auscultation allows you to obtain information about the work of the heart, its structure and function, as well as the condition of the great vessels (aorta, pulmonary vessels). The volume and reliability of information depends on:
· compliance with the basic rules of auscultation;
· use of additional techniques (listening in various positions, after dosed physical activity, at the height of maximum inhalation and exhalation, after holding the breath and simulating breathing movements);
· thoroughness and consistency of auscultation;
· presence or absence of hearing pathology from the doctor;
· the doctor’s ability to focus his attention on sounds;
· the doctor’s ability to analyze sound information, the correctness and consistency of the analysis;
· experience as a doctor;
· the doctor’s ability to identify side effects. murmurs that occur outside the heart when incorrect. auscultation technique.
Auscultation of the heart reveals sound phenomena that are classified as heart sounds , extracardiac murmurs (associated with pericardial pathology, intracardial murmurs (occur both in healthy people under certain conditions and in pathologies of the heart, blood vessels, and valve apparatus)
The opening of the valves is not accompanied by distinct vibrations, i.e. almost silently, and the closure is accompanied by a complex auscultation pattern, which is regarded as sounds I and II.
The first sound occurs when the atrioventricular valves (mitral and tricuspid) close. Louder, longer lasting. This is a systolic sound, as it is heard at the beginning of systole.
The second tone is formed when the semilunar valves of the aorta and pulmonary artery close.
The first sound is called systolic and according to the mechanism of formation it consists of 4 components :
- the main component is the valve component, represented by amplitude oscillations resulting from the movement of the cusps of the mitral and tricuspid valves at the end of diastole and the beginning of systole, with the initial oscillation observed when the cusps of the mitral valve close, and the final oscillation when the cusps of the tricuspid valve close, therefore the mitral and tricuspid components are distinguished ;
- muscle component - low-amplitude oscillations are layered on high-amplitude oscillations of the main component ( isometric ventricular tension , appears approximately 0.02 seconds before the valve component and is layered on it); and also arise as a result of asynchronous contractions of the ventricles during systole, i.e. as a result of contraction of the papillary muscles and interventricular septum, which ensure the closure of the mitral and tricuspid valves;
- vascular component - low-amplitude oscillations that occur at the moment of opening of the aortic and pulmonary valves as a result of vibration of the walls of the aorta and pulmonary artery under the influence of the blood flow moving from the ventricles to the great vessels at the beginning of ventricular systole (the ejection period). These oscillations occur after the valve component at approximately 0.02 seconds;
- atrial component – low-amplitude oscillations resulting from atrial systole. This component precedes the valve component of the first tone. It is detected only in the presence of mechanical atrial systole, disappears with atrial fibrillation, nodal and idioventricular rhythm, AV block (absence of atrial excitation wave).
The second sound is called diastolic and occurs as a result of the closure of the cusps of the semilunar valves of the aorta and pulmonary artery. It begins diastole and ends systole. Consists of 2 components :
1. the valve component arises as a result of the movement of the leaflets of the semilunar valves of the aorta and pulmonary artery at the moment of their slamming;
2. the vascular component is associated with vibration of the walls of the aorta and pulmonary artery under the influence of the blood flow directed towards the ventricles.
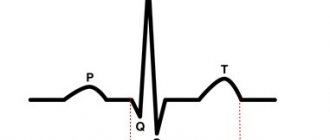
When analyzing heart sounds, it is necessary to determine their number and find out the first . At a normal heart rate, the solution to this problem is clear: the first sound occurs after a longer pause, i.e. diastole, II tone – after after a short pause, i.e. systole. For tachycardia, especially in children, when systole is equal to diastole, this method is not informative and the following technique is used: auscultation in combination with palpation of the pulse in the carotid artery; the tone that coincides with the pulse wave is I.
In adolescents and young people with a thin chest wall and a hyperkinetic type of hemodynamics (increased speed and increased strength, during physical and mental stress), additional III and IV tones (physiological) appear. Their appearance is associated with vibrations of the walls of the ventricles under the influence of blood moving from the atria to the ventricles during ventricular diastole.
III tone is protodiastolic, because appears at the beginning of diastole immediately after the second sound. It is better heard by direct auscultation at the apex of the heart. It is a weak, low, short sound. It is a sign of good development of the ventricular myocardium. With an increase in the tone of the ventricular myocardium in the phase of rapid filling in ventricular diastole, the myocardium begins to oscillate and vibrate. It is heard 0.14 -0.20 after the second tone.
IV tone is presystolic, because appears at the end of diastole, precedes the first sound. Very quiet, short sound. It is heard in individuals with increased ventricular myocardial tone and is caused by fluctuations in the ventricular myocardium when blood enters them during atrial systole. Most often heard in an upright position in athletes and after emotional stress. This is due to the fact that the atria are sensitive to sympathetic influences, therefore, with an increase in the tone of the sympathetic nervous system, there is some advance of contractions of the atria from the ventricles and therefore the fourth component of the 1st sound begins to be heard separately from the 1st tone and is called the 4th tone.
Changes in tones
Heart sounds are essentially sound waves, so their changes occur when the conduction of sound is disrupted and the structures that produce these sounds are pathological. There are two main groups of reasons why heart sounds sound different from the norm:
- Physiological – they are related to the characteristics of the person being studied and his functional state. For example, excess subcutaneous fat near the pericardium and on the anterior chest wall in obese people impairs sound conduction, so heart sounds become muffled.
- Pathological - they occur when the structures of the heart and the vessels extending from it are damaged. Thus, narrowing of the atrioventricular opening and compaction of its valves leads to the appearance of a clicking first tone. When they collapse, dense sashes produce a louder sound than normal, elastic ones.
Heart sounds are called muffled when they lose their clarity and become difficult to distinguish. Weak dull tones at all points of auscultation suggest:
changes in heart sounds characteristic of certain disorders
- Diffuse damage to the myocardium with a decrease in its ability to contract - extensive myocardial infarction, myocarditis, atherosclerotic cardiosclerosis;
- Effusion pericarditis;
- Deterioration of sound conduction for reasons not related to the heart - emphysema, pneumothorax.
The weakening of one tone at any point of auscultation gives a fairly accurate description of changes in the heart:
- Muffling of the first tone at the apex of the heart indicates myocarditis, sclerosis of the heart muscle, partial destruction or insufficiency of the atrioventricular valves;
- Muffling of the second tone in the 2nd intercostal space on the right occurs with insufficiency of the aortic valve or narrowing (stenosis) of its mouth;
- Muffling of the second tone in the 2nd intercostal space on the left indicates insufficiency of the pulmonary valve or stenosis of its mouth.
In some diseases, changes in heart sounds are so specific that they receive a separate name. Thus, mitral stenosis is characterized by a “quail rhythm”: the clapping first tone is replaced by an unchanged second tone, after which an echo of the first appears - an additional pathological tone. A three- or four-part “gallop rhythm” occurs with severe myocardial damage. In this case, the blood quickly stretches the thinned walls of the ventricle and their vibrations give rise to an additional tone.
An increase in all heart sounds at all points of auscultation occurs in children and asthenic people, since their anterior chest wall is thin and the heart lies quite close to the phonendoscope membrane. The pathology is characterized by an increase in the volume of individual tones in a certain location:
- A loud first sound at the apex occurs with narrowing of the left atrioventricular orifice, sclerosis of the mitral valve leaflets, tachycardia;
- A loud second sound in the 2nd intercostal space on the left indicates an increase in pressure in the pulmonary circulation, which leads to stronger collapse of the pulmonary valve leaflets;
- A loud second sound in the 2nd intercostal space on the left indicates increased pressure in the aorta, atherosclerosis, and hardening of the aortic wall.
Arrhythmic tones indicate a disturbance in the conduction system of the heart. Heart contractions occur at different intervals, since not every electrical signal passes through the entire thickness of the myocardium. Severe atrioventricular block, in which the work of the atria is not coordinated with the work of the ventricles, leads to the appearance of a “gun tone”. It is caused by a simultaneous contraction of all chambers of the heart.
Double tone is the replacement of one long sound with two short ones. It is associated with desynchronization of the valves and myocardium. The splitting of the first tone occurs due to:
- Non-simultaneous closure of the mitral and tricuspid valves with mitral/tricuspid stenosis;
- Disturbances in the electrical conductivity of the myocardium, due to which the atria and ventricles contract at different times.
The bifurcation of the second tone is associated with a discrepancy in the time of collapse of the aortic and pulmonary valves, which indicates:
- Excessive pressure in the pulmonary circulation;
- Arterial hypertension;
- Left ventricular hypertrophy with mitral stenosis, due to which its systole ends later and the aortic valve closes late.
With ischemic heart disease, changes in heart sounds depend on the stage of the disease and the changes that have occurred in the myocardium. At the onset of the disease, pathological changes are mild and heart sounds remain normal during the interictal period. During an attack, they become muffled, irregular, and a “gallop rhythm” may appear. The progression of the disease leads to persistent myocardial dysfunction with the preservation of the described changes even outside of an angina attack.
It should be remembered that a change in the nature of heart sounds does not always indicate pathology of the cardiovascular system. Fever, thyrotoxicosis, diphtheria and many other causes lead to changes in heart rhythm, the appearance of additional tones or their muffling. Therefore, the doctor interprets auscultatory data in the context of the entire clinical picture, which makes it possible to most accurately determine the nature of the emerging pathology.
Lecture 6. Auscultation of the heart. Normal and pathological heart sounds
Auscultation of the heart. Normal and pathological heart sounds.
Ex. questions:
1. The mechanism of formation of the first tone, its characteristics in a healthy person, physiological variants.
2. The mechanism of formation of the second tone, its characteristics in a healthy person, physiological variants.
3. The mechanism of formation of the III and IV physiological heart sounds, their characteristics.
4. Reasons for strengthening and weakening of the first heart sound in pathology.
5. Reasons for strengthening and weakening of the second heart sound in pathology.
6. Reasons for strengthening and weakening of both heart sounds in normal and pathological conditions.
7. Splitting and bifurcation of the first tone: causes, mechanisms of formation in pathology.
8. Splitting and bifurcation of the second tone: causes and mechanisms of occurrence in normal and pathological conditions.
9. Pathological III and IV tones: causes and mechanisms of formation, clinical characteristics, FCG diagnostics.
10. Mitral valve opening tone: causes and mechanism of formation, clinical characteristics, FCG diagnostics
11. Gallop rhythm: variants, causes and mechanisms of occurrence, clinical characteristics, FCG diagnostics.
12. Pendulum-shaped rhythm, causes and mechanism of formation, clinical characteristics, diagnostic significance.
Auscultation of the heart.
There are two main phases of the cardiac cycle: systole and diastole.
Systole is the contraction of the ventricles. By the time of systole, the ventricles are filled with blood, the AV valves are open, and the semilunar valves are closed.
Systole begins with a phase of asynchronous contraction of the ventricles, when only individual myocardial fibers contract, which leads to an increase in pressure in the ventricular cavity and closure of the AV valves.
After the closure of the atrioventricular valves (the period of closed valves), the phase of isometric ventricular tension begins, as a result of which intraventricular pressure significantly increases and the semilunar valves of the aorta and pulmonary artery open.
A period of rapid expulsion of blood from the ventricles into the great vessels begins. At the beginning of the ejection period, the pressure in the ventricles is much higher than in the large vessels. Then, with an increase in blood volume in the great vessels, the pressure in the ventricles decreases, and in the great vessels increases. This leads to a gradual decrease in the speed of blood movement from the ventricles to the aorta and pulmonary artery, and the slow expulsion phase begins.
By the end of systole, the pressure in the vessels is higher than in the ventricles, which forms a reverse flow of blood in the vessels, while the leaflets of the semilunar valves fill with blood and slam shut. From the moment the semilunar valves close, ventricular diastole begins.
After the closure of the semilunar valves, the phase of isometric ventricular relaxation begins. At this point, the atria are filled with blood, the ventricles are empty, and the valves are closed (closed valve period). According to the pressure gradient, blood from the atria rushes into the ventricles, and the AV valves open.
The period of ventricular filling begins. At the beginning of this period, blood quickly moves along a pressure gradient into the ventricles (a period of rapid passive ventricular filling). As the ventricles fill with blood, the flow rate decreases—a phase of slow passive ventricular filling. To move additional blood volume, atrial systole (a period of rapid active filling of the ventricles) occurs at the very end of diastole.
During the work of the heart, sound phenomena occur that can be detected by auscultation. These are heart sounds. The opening of the heart valves is normally not accompanied by the appearance of sound; heart sounds are formed by the closing of the valves and vibrations of the myocardium and blood vessels. When auscultating the heart, 2 tones are normally heard at all points of auscultation.
The first sound is called systolic, as it is heard at the beginning of systole. According to the mechanism of formation, it consists of 4 components:
1. the main component is the valve component, formed by the sound of the closing of the mitral and tricuspid valves at the beginning of systole - in the phase of asynchronous contraction, and the mitral valve closes first, and a little later the tricuspid valve. But the time between the closure of the mitral and tricuspid valves is 0.02 s and is not distinguishable by the ear: this is the time of physiological asynchrony.
2. muscular component – caused by fluctuations of the ventricular myocardium in the phase of isometric ventricular tension;
3. vascular component - caused by fluctuations in the initial parts of the aorta and pulmonary artery under the influence of the blood flow moving from the ventricles to the great vessels in the rapid expulsion phase.
4. atrial component – caused by vibrations of the ventricular myocardium during atrial systole. This component precedes the valve component of the first tone.
The second sound is called diastolic; it is heard at the beginning of diastole.
Consists of 2 components:
1. the valve component is formed by the sound of the slamming of the valves of the semilunar valves of the aorta and pulmonary artery;
2. the vascular component is associated with vibration of the walls of the aorta and pulmonary artery under the influence of the blood flow directed towards the ventricles.
The semilunar valves do not close simultaneously; the time between the closure of the aortic and pulmonary valves is also 0.02 s - this is the time of physiological asynchrony.
When analyzing heart sounds, it is necessary to be able to distinguish between the first and second sounds:
· The first tone occurs after a longer pause, i.e. diastole, II tone - after a short pause, i.e. systole.
· The first sound is louder than the second at the apex and at the 4th point of auscultation (there is a projection of the mitral and tricuspid valves, the closure of which produces the first sound). The first tone is longer and lower. The second sound is louder than the first at the base of the heart - at the 2nd and 3rd points of auscultation (projection points of the semilunar valves), it is shorter and higher.
· In case of tachycardia, especially in children, when systole is equal to diastole, the following technique will help to distinguish sounds I and II: auscultation in combination with palpation of the pulse in the carotid artery; the tone that coincides with the pulse in the carotid artery is I.
III and IV physiological tones.
Their appearance is associated with vibrations of the ventricular myocardium under the influence of blood moving from the atria to the ventricles during ventricular diastole. The conditions for the occurrence of III and IV physiological tones are high myocardial tone. These tones can be heard in adolescents and young adults with a thin chest wall and a hyperkinetic type of hemodynamics (increased speed and increased strength during physical and mental stress). They are better heard by direct auscultation at the apex of the heart.
The third sound is protodiastolic, it appears at the beginning of diastole 0.14-0.20 s after the second sound. With high myocardial tone in the phase of rapid passive filling of the ventricles, the myocardium begins to oscillate and vibrate under the influence of blood flow. It is a weak, low, short sound.
The IV tone is presystolic, it appears at the end of diastole and precedes the I tone. Very quiet, short sound. It is heard in individuals with high ventricular myocardial tone and increased tone of the sympathetic nervous system. The IV tone is caused by vibrations of the ventricular myocardium when blood enters them in the phase of atrial systole - the phase of active filling of the ventricles (as the 4th component of the I tone). Most often heard in an upright position in athletes and after emotional stress. This is due to the fact that the atria are sensitive to sympathetic influences, therefore, with an increase in the tone of the sympathetic nervous system, there is some advance of contractions of the atria from the ventricles and therefore the fourth component of the 1st sound begins to be heard separately from the 1st tone and is called the 4th tone.
Changes in the sonority of heart sounds.
The simultaneous strengthening or weakening of sounds I and II is primarily due to extracardiac reasons.
The reasons for the increase in both tones are normal:
1. Thin chest wall – with poor development of muscles and pancreas
2. Physical and emotional stress, while heart rate increases, diastole shortens, and diastolic filling of the ventricles decreases. The force of contraction of the ventricles and the speed of blood flow increase, which leads to increased sounds.
In pathology, the intensification of both tones is due to extracardiac reasons:
1. Reduced airiness of the lung tissue at the site of the projection of the heart onto the chest wall - pneumosclerosis, inflammatory infiltration.
2. An air resonating cavity in the lung adjacent to the heart - sound amplification occurs in it.
3. Tumor of the posterior mediastinum, in which the heart approaches the chest wall.
4. Increase in heart rate during fever, thyrotoxicosis - diastolic filling of the ventricles decreases.
The reasons for the weakening of both tones are normal:
1. Thick chest wall - with excessive development of muscles and adipose tissue.
2. In a dream. At the same time, heart rate decreases, diastolic filling of the ventricles increases, and blood flow speed decreases. In the supine position, the heart moves away from the anterior chest wall and the sonority of the tones weakens.
In pathology, weakening of the 1st and 2nd sounds is mainly due to extracardiac reasons:
1. Increased airiness of the lung tissue at the site of the projection of the heart onto the chest wall - with pulmonary emphysema.
2. Left-sided exudative pleurisy or pneumothorax, moving the heart away from the anterior chest wall.
3. Effusion pericarditis.
The intracardial reason for the simultaneous weakening of both tones is a decrease in the contractility of the ventricular myocardium. Causes: myocardial dystrophy, myocarditis, myocardiopathy, cardiosclerosis. At the same time, the speed of blood flow and the force of myocardial contraction decrease, which leads to a weakening of the first sound, the volume of blood entering the aorta and pulmonary artery decreases, which means that the second sound weakens.
Auscultation of the heart is performed at the following points:
1. the area of the apex of the heart, which is determined by the location of the apex beat. This is the projection point of the mitral valve;
2. II intercostal space at the right edge of the sternum. The aortic valve is heard here;
3. II intercostal space at the left edge of the sternum. The pulmonary valve is heard here;
4. Place of attachment of the xiphoid process to the body of the sternum. The tricuspid valve is heard here
5. Botkin-Erb point – III intercostal space 1-1.5 cm outward from the left edge of the sternum. Here, sound vibrations are heard that occur during the operation of the aortic valve, and less commonly, the mitral valve.
During auscultation, the points of maximum sound of heart sounds are determined:
I tone – area of the apex of the heart (I tone is louder than II)
II tone – area of the base of the heart.
The sonority of the second tone to the left and right of the sternum is compared.
In healthy children, adolescents, and young people of asthenic body type, an increase in the second tone on the pulmonary artery is observed (quieter on the right than on the left). With age, an increase in the second tone above the aorta (second intercostal space on the right) is observed.
The causes of an isolated change in the sonority of the first or second tone are often intracardial.
Strengthening of the first tone is associated primarily with a decrease in diastolic filling of the ventricles. Causes:
- mitral stenosis. Thickening of the mitral valve leaflets leads to an increase in the sonority of the valve component of the first sound, a decrease in the diastolic blood volume in the LV leads to an increase in the rate of myocardial contraction and an increase in the muscular and vascular components of the first sound. The first sound in mitral stenosis is called the flapping first sound.
- tachycardia
- extrasystole. Strengthening of the first tone is determined at the moment of extraordinary contraction of the heart after a short diastole.
- atrial fibrillation, tachyform. Shortening of diastole.
- complete AV block, when there is a complete separation in time of contraction of the ventricular myocardium and the atrium myocardium. At the moment when the contraction of the atria coincides with the contraction of the ventricles, the first sound is intensified - the Strazhesko cannon tone.
If at the top the 1st tone is equal in volume to the 2nd or quieter than the 2nd tone, the 1st tone is weakened. Causes:
- mitral or tricuspid valve insufficiency. The absence of a period of closed valves leads to a sharp weakening of the valve component. Diastolic overflow of the ventricles leads to a weakening of the muscular and vascular components of the first sound.
- aortic valve insufficiency - in diastole more blood enters the left ventricle - the speed of its contraction and the speed of blood flow decreases.
- stenosis of the aortic mouth - the first sound weakens due to pronounced hypertrophy of the LV myocardium, a decrease in the rate of myocardial contraction due to the presence of increased afterload.
- diseases of the heart muscle, accompanied by a decrease in myocardial contractility (myocarditis, cardiomyopathies, cardiosclerosis), but if cardiac output decreases, then the second tone also decreases.
— myocardial hypertrophy, for example, with hypertension, hypertrophic cardiomyopathy. At the same time, the rate of myocardial contraction decreases.
Changing the volume of tone II.
Normally, the sonority of the second tone at the second and third points of auscultation is the same. This is explained by the fact that although the pressure in the aorta is higher than the pressure in the pulmonary artery, the aortic valve is located deeper. If at the second or third points of auscultation there is an increase in the II tone, this is called an accent of the II tone. It may be over the aorta or pulmonary artery.
Reasons for the accentuation of the second tone over the pulmonary artery:
1. Physiological reason - in children and young people under 25 years of age. The reason is the more superficial location of the pulmonary valve and the higher elasticity of the aorta, lower pressure in it. With age, blood pressure in the BCC increases; The PA moves posteriorly, the accent of the 2nd tone above the LA disappears.
2. In pathology, an increase in the second tone over the PA is caused by an increase in pressure in the ICC and is observed with mitral heart defects, chronic respiratory diseases, and primary pulmonary hypertension.
Reasons for the accentuation of the second tone over the aorta:
- increased blood pressure
- atherosclerosis of the aorta, increased tone II appears due to sclerotic compaction of the aortic valve leaflets and aortic walls.
Reasons for weakening of the second tone
to LA:
– insufficiency of the pulmonary valve, stenosis of the orifice of the pulmonary artery.
Above the aorta:
- severe arterial hypotension
- insufficiency of the aortic valve - in this case, the leaflets of the aortic valve do not close, therefore, the valve component of the second tone is weakened.
- stenosis of the aortic mouth - as a result of a decrease in the speed of blood flow through the narrowed opening of the aortic valve, the vascular component of the second sound is weakened.
Splitting and splitting tones.
In healthy people, there is asynchronism in the work of the right and left ventricles; normally it does not exceed 0.02 seconds; this difference is indistinguishable by the ear, and we hear one tone.
If the time between contraction of the right and left ventricles increases by more than 0.02 s, then each tone is not perceived as a single sound. If the asynchronism time increases within 0.02-0.04 seconds, this is splitting. If the asynchronism time is 0.05 sec. and more - this is a bifurcation - a more noticeable doubling of tone.
The reasons for splitting and splitting tones are the same, the only difference is time.
Physiological cause of splitting and bifurcation of the first tone:
- can be heard at the end of expiration, when intrathoracic pressure rises and blood flow from the ICC vessels to the left atrium increases, resulting in increased blood pressure on the atrial surface of the mitral valve. This slows down its closure, which leads to auscultation of the cleft.
Pathological bifurcation of the first tone occurs when:
- blockade of one of the bundle branches, this leads to a delay in the contraction of one of the ventricles.
- ventricular extrasystole. In this case, the ventricle in which the impulse originated contracts faster.
- Severe myocardial hypertrophy, more often of the left ventricle (with aortic hypertension, aortic stenosis). In this case, the hypertrophied ventricle contracts more slowly.
Splitting and bifurcation of the second tone.
Functional splitting or bifurcation of the second tone is observed more often than the first; it occurs in young people at the end of inhalation or the beginning of exhalation, during physical activity. The reason is the non-simultaneous end of systole of the left and right ventricles.
Pathological splitting or bifurcation of the second tone is more often observed in the pulmonary artery. The mechanism is associated with an increase in pressure in the ICB and a delay in the closure of the pulmonary valve compared to the aortic valve. Causes: mitral valve defects, primary pulmonary hypertension, emphysema and other chronic respiratory diseases. As a rule, an increase in the II tone on the LA is accompanied by splitting or bifurcation of the II tone on the LA.
Pathological III and IV tones. The condition for their occurrence is a sharp decrease in the contractility of the myocardium - “flabby myocardium”.
The third tone appears after 0.12-0.20 seconds. after the second sound, that is, at the beginning of diastole, in the phase of rapid filling of the ventricles. If the ventricular myocardium has lost its tone, when the ventricular cavity is filled with blood, the muscle easily and quickly stretches, the ventricular wall vibrates, and sound is produced. The diagnostic value of a pathological III tone is severe myocarditis, myocardial dystrophy.
Pathological IV sound occurs before the I tone at the end of diastole during atrial systole. The conditions for its occurrence are: a sharp decrease in the tone of the ventricular myocardium and the presence of overcrowded atria. Rapid stretching of the wall of the ventricles, which have lost their tone, when a large volume of blood enters them in the atrial systole phase causes myocardial vibrations and a fourth pathological tone appears.
III and IV sounds are better heard at the apex of the heart, on the left side. The emergence of a gallop rhythm is associated with the appearance of III and IV pathological tones.
The gallop rhythm was first described by Obraztsov in 1912 - “the cry of the heart for help.” It is a sign of a sharp decrease in myocardial tone and a sharp decrease in the contractility of the ventricular myocardium. So named because it resembles the rhythm of a galloping horse.
Signs:
- tachycardia,
- weakening of I and II tones,
- the appearance of pathological III or IV tones.
Highlight:
· protodiastolic gallop rhythm – three-part rhythm due to the appearance of the third pathological tone,
Presystolic – due to the appearance of IV pathological tone,
· mesodiastolic – when an additional tone appears in the middle of diastole (with severe tachycardia, sounds III and IV merge, a summation tone is heard in the middle of diastole).
Mitral valve opening tone.
– a sign of mitral stenosis. With mitral stenosis, the cusps of the mitral valve are fused with each other; when blood flows from the atria into the ventricles, the opening of the mitral valve is accompanied by a strong tension of the cusps, a sound is formed - the tone of the opening of the mitral valve, it appears 0.07-0.12 seconds after the second sound.
The quail rhythm, or melody of mitral stenosis, is a rhythm caused by the appearance of the opening tone of the mitral valve, including:
- loud, clapping I tone,
- accent and splitting or bifurcation of the second tone on LA,
- tone of mitral valve opening.
The quail rhythm is best heard at the apex of the heart.
Pendulum rhythm.
The condition for its occurrence is a sharp decrease in myocardial tone. In this case, both phases of cardiac activity - systole and diastole - are balanced in time. This occurs either due to shortening of diastole or due to lengthening of systole. I and II tones are weakened and are equal in sonority to each other. The pendulum-like rhythm is reminiscent of the sound of a clock pendulum swinging. If the pendulum-like rhythm is accompanied by tachycardia, this indicates embryocardia, that is, the melody resembles the heartbeat of a fetus.