Acute coronary syndrome (ACS) is a serious condition caused by impaired coronary circulation and myocardial ischemia. When the blood supply to the heart muscle completely stops, hypoxia occurs, which is the direct cause of heart attack and death. This deadly pathological process is popularly called a pre-infarction condition or a heart attack. ACS is a general concept that includes a number of processes that are equal in origin and similar in course, but differ in prognosis and likelihood of cure.
Diseases of the cardiovascular system, which are based on coronary insufficiency syndrome, are designated by the term ACS. This is what clinicians call heart diseases in which its blood supply deteriorates: myocardial infarction and unstable angina. These diseases have similar initial manifestations, pathophysiological mechanisms and some treatment principles. That is why the concept of “acute coronary syndrome” was introduced into medical practice. It is used to make a preliminary diagnosis, when all the characteristics of the patient’s pathological process are not fully clarified.
Acute coronary syndrome has an ICD-10 code of 124.9 and the name “Acute coronary heart disease, unspecified.” The causes of the pathology most often are: thrombosis and thromboembolism caused by rupture of an atherosclerotic plaque or erosion of the endothelium of the coronary artery. There is a special form of the syndrome that is of allergic origin. It is associated with excess production of inflammatory mediators by mast cells. Symptoms of the syndrome are: shortness of breath, irregular heart rhythm, pressing chest pain that occurs at rest or with minor physical stress. The most dangerous sign of ACS is sudden cardiac arrest. This diagnosis is usually made in the intensive care unit.
Coronary disease occurs with pronounced periods of exacerbation and remission. IHD worsens under the influence of provoking factors. In this case, its mild form develops - unstable angina or a severe form - myocardial infarction. In the first case, acute ischemia of the heart muscle does not lead to necrosis. Due to narrowing or blockage of the coronary arteries, trophic changes occur that develop gradually, slowly, in steps. After exposure to the trigger factor, an attack of ACS occurs. With myocardial infarction, irreversible cell death occurs. This pathology is much more dangerous - it is accompanied by severe chest pain, impaired breathing and consciousness, and an avalanche-like death of cardiomyocytes. Destruction of large areas is manifested by the most severe symptoms. With angina pectoris, there are no ECG signs of myocardial necrosis and specific biochemical markers in the blood. It is possible to transition from one clinical form of IHD to another.
The characteristic clinical picture of the syndrome allows you to quickly make a diagnosis and help the patient. To save his life, you should know the algorithm for providing emergency medical care and be able to carry out all the necessary measures before the arrival of qualified specialists. Emergency treatment of ACS will help avoid the development of serious complications and death. It is effective only if diagnosed early. General therapeutic measures prescribed to patients depend on clinical manifestations, the severity of pathological changes and the general well-being of the patient.
Currently, acute coronary syndrome is a pressing medical problem. This is due to the high frequency of its occurrence and the need for preventive measures. The development and implementation of a new medical strategy can save the lives of patients with ACS.
Added codes
A09.0 A09.9 A92.5 A97 A97.0 A97.1 A97.2 A97.9 B17.9 B33.4† B98 B98.0 B98.1 C00-C75 C80.0 C80.9 C81.4 C82. 3 C82.4 C82.5 C82.6 C84.6 C84.7 C84.8 C84.9 C85.2 C86 C86.0 C86.1 C86.2 C86.3 C86.4 C86.5 C86.6 C88.4 C90.3 C91.6 C91.8 C92.6 C92.8 C93.3 C94.6 C96.4 C96.5 C96.6 C96.8 D46.5 D46.6 D47.4 D47.5 D68.5 D68. 6 D89.3 E16.4 E88.3 G14 G21.4 G23.3 G83.5 G83.6 G90.4 G90.5 G90.6 G90.7 H54.9 I27.2 I48.0 I48.1 I48.2 I48.3 I48.4 I48.9 I72.5 I72.6 I98.3* J09 J12.3 J21.1 J98.7 K02.5 K12.3 K22.7 K31.7 K35.2 K35.3 K35.8 K43.2 K43.3 K43.4 K43.5 K43.6 K43.7 K52.3 K55.3 K58.1 K58.2 K58.3 K58.8 K63.5 K64 K64.0 K64.1 K64.2 K64 .3 K64.4 K64.5 K64.8 K64.9 K66.2 K75.4 K85.0 K85.1 K85.2 K85.3 K85.8 K85.9 L89.0 L89.1 L89.2 L89.3 L89.9 L98.7 M31.7 M72.6 M75.6 M79.7 N18.1 N18.2 N18.3 N18.4 N18.5 N42.3 O14.2 O43.2 O60.0 O60.1 O60. 2 O60.3 O94 O96.0 O96.1 O96.9 O97.0 O97.1 O97.9 O98.7 P35.4 P91.6 P91.7 Q31.5 R17.0 R17.9 R26.3 R29.6 R50.2 R50.8 R57.2 R63.6 R65 R65.0 R65.1 R65.2 R65.3 R65.9 R95.0 R95.9 T76 U04 U06 U07 U82 U83 U84 U85 W26.0 W26.8 W26. 9 W46 X34.0 X34.1 X34.8 X34.9 X59.0 X59.9 Z52.6 Z52.7 Z58.7
Changed codes
How to recognize and what to do if acute coronary syndrome occurs
A00-B99 A02.1 A02.2 A04 A04.7 A05 A06.4† A06.5† A08 A08.1 A09 A09.0 A09.9 A15-A19 A18.1 A18.5 A18.6 A18.8 A22.7 A24.0 A24.1 A24.4 A26.7 A32.7 A40 A40.0 A40.1 A40.2 A40.3 A40.8 A40.9 A41 A41.0 A41.1 A41.2 A41.3 A41.4 A41.5 A41.8 A41.9 A42.7 A48.3 A49.0 A49.1 A49.2 A49.3 A52.1 A54.2 A54.8 A56. 1 A75 A79.8 A81 A81.8 A81.9 A92-A99 A93.8 A97.0 A98 A98.5 B00.5 B00.7 B00.8 B02.3 B07 B15-B19 B16.9 B17.0 B17.9 B18 B18.1 B19.0 B19.9 B20-B24 B20.1 B20.2 B20.6 B34.0 B34.1 B34.2 B34.3 B34.4 B37.4 B37.7 B57.2 B59† B60 B67 .4 B71.1 B81 B81.3 B81.8 B83.2 B90-B94 B91 B95-B98 B95.2 B96 B96.5 B97.8 C00-C97 C00-D48 C26.1 C69.4 C69.9 C71.0 C76 C77 C78.2 C78.7 C79 C79.9 C80 C80.9 C81 C81-C96 C81.0 C81.1 C81.2 C81.3 C81.4 C81.7 C81.9 C82 C82.0 C82.1 C82. 2 C82.7 C82.9 C83 C83.0 C83.1 C83.3 C83.5 C83.7 C83.8 C83.9 C84 C84.4 C84.5 C85 C85.7 C86.6 C88 C88.0 C88.2 C88.3 C90 C90.0 C90.1 C90.2 C91 C91.0 C91.1 C91.3 C91.5 C91.7 C91.8 C92 C92.0 C92.1 C92.2 C92.3 C92.4 C92. 5 C92.7 C93 C93.0 C93.1 C94 C94.0 C94.2 C94.4 C94.7 C95 C95.0 C96 C96.0 C96.2 D07.5 D29.1 D31.4 D31.9 D45 D46 D46 .0 D46.1 D46.2 D46.7 D47 D47.0 D47.1 D47.2 D47.7 D56.1 D57 D57.2 D57.3 D63.8* D64 D68.3 D68.8 D70 D72 D75.1 D76 D76.1 D80-D89 D89 D89.3 E10 E11 E12 E13 E14 E16.8 E21.2 E64 E64.3 E66.2 E68 E71.3 E72.0 E72.3 E74.0 E83.3 E84.1 E84. 8 E88 E88.0 F02.8* F03 F05.1 F05.8 F06.3 F07.2 F10-F19 F31 F31.8 F31.9 F45.0 F48.8 F50.5 F52.1 F54 F80.1 F80. 2 F84.4 G04.8 G05.1* G09 G10-G14 G11 G23 G23.1 G23.2 G23.8 G25.8 G31.0 G31.8 G51.0 G61.0 G63.8* G73.1* G80 G80.0 G80.1 G80.2 G80.3 G80.8 G80.9 G81 G82 G91 G98 G99.8* H02.5 H18.1 H31.8 H32.8* H50.2 H50.4 H54 H54.0 H54 .1 H54.2 H54.3 H54.4 H54.5 H54.6 H59.0 H59.8 H65 H66 H67.1* I05 I07 I08 I08.0 I10-I15 I12 I20-I25 I20.8 I21.4 I22 I25 .4 I27.0 I27.8 I32.8* I34 I35 I36 I37 I38 I41.1* I42.0 I42.5 I45.8 I47 I47.1 I48 I49 I49.8 I50.1 I50.9 I60 I60.9 I62 .0 I63 I67.1 I68.8* I69 I70 I72 I72.0 I72.1 I72.2 I72.3 I72.4 I72.5 I72.8 I72.9 I77.2 I77.8 I84.3 I87.0 I95 .1 I98.2* I98.3* J00-J99 J02.8 J04.0 J06 J09 J09-J18 J10 J10.0 J10.1 J10.8 J12 J15.6 J18 J22 J34.1 J38 J40-J47 J44.0 J44.8 J60 J61 J62 J63 J64 J68.1 J84.1 J85.1 J95.4 J96 K04.0 K08.8 K09.0 K09.1 K09.8 K10.2 K12.3 K14 K22.0 K22.1 K22 .2 K29 K29.6 K30 K35.0 K35.3 K35.9 K43 K43.0 K43.1 K43.9 K51.0 K51.4 K51.5 K51.9 K52.1 K52.3 K52.8 K52.9 K55-K64 K55.2 K56 K56.6 K59.3 K62 K62.8 K63.0 K63.1 K64.4 K70-K77 K72 K72.0 K73.2 K75 K75.0 K75.4 K76.0 K76.8 K77 .0* K85 K92.1 L08.0 L20-L30 L70.5 L82 L88 L89 L90.0 L91.0 L97 L98.4 L98.5 M00 M00-M99 M10.3 M14.6* M24.8 M30-M36 M36 .1* M43.6 M45 M51.1† M62.2 M65.8 M70 M72.4 M72.8 M72.9 M79.0 M85.8 M86.9 M87 M89.0 M89.6 M91 M94.0 N00-N08 N03 N05 N08.0* N08.1* N08.5* N10-N16 N16.0* N17 N18 N18.1 N18.4 N18.5 N18.9 N19 N20 N20.9 N26 N28.1 N29.8* N32. 8 N36.3 N39.3 N39.4 N40 N48.0 N48.6 N80.8 N81.0 N85 N87.0 O00-O99 O08.0 O08.3 O10 O11 O13 O14 O14.0 O15 O16 O22 O23 O24 O24. 0 O24.1 O26.6 O29.0 O33.7 O60 O60.0 O60.1 O60.2 O62.0 O69.2 O69.8 O70 O70.0 O71.4 O71.5 O72.0 O73.0 O74. 0 O75.3 O80-O84 O85 O86 O87 O88.1 O89.0 O94 O94-O99 O96 O96.0 O96.1 O96.9 O97 O98 O98.7 O99.6 O99.7 O99.8 P00-P96 P00.2 P04 P08.1 P28.3 P28.4 P28.8 P29.3 P35-P39 P37 P52.2 P59.2 P70.0 P70.1 P75* P76 P76.0 P76.8 P78.3 P78.8 P93 P96. 1 P96.4 Q01 Q03 Q13.8 Q15.0 Q18.1 Q21.8 Q24.1 Q25.3 Q25.6 Q31 Q35-Q37 Q35.1 Q35.3 Q35.5 Q35.9 Q36.1 Q37.0 Q37 .1 Q37.2 Q37.3 Q37.4 Q37.5 Q37.8 Q37.9 Q39.4 Q40.2 Q61 Q61.0 Q61.1 Q61.2 Q61.4 Q75.4 Q77.4 Q87.0 Q89. 3 Q93.5 R00.0 R00.1 R01.1 R03.1 R06 R06.1 R10.1 R12 R17 R19.5 R45.8 R46.8 R52 R53 R55 R57 R63.6 R64 R65.1 R68.3 R71 R75 R90.8 R95 R96.0 S00-S09 S00-T98 S05.9 S37 S37.8 S43.4 S46.0 S76.1 S78 S79 S82.1 S83.6 S86 T14.6 T31 T32 T36-T50 T40 T42 T43 T44 .5 T48.6 T56 T56.8 T60.2 T60.4 T71 T75.8 T78.9 T79 T80.2 T80.6 T81 T81.1 T81.4 T82.8 T88.0 U00-U49 U04.9 U07. 0 U07.1 U07.2 U82-U85 V01-V99 W00-W19 W13 W17 W23 W25 W26 W27 W45 W80 W84 W85-W99 X09 X25 X37 X38 X39 X40-X49 X47 X53 X54 X59 X67 Y10-Y34 Y17 Y35 Y35.0 Y3 5 .1 Y35.2 Y35.3 Y35.4 Y36.2 Y45.8 Y60-Y69 Y70-Y82 Y83-Y84 Y85-Y89 Z21 Z45.0 Z51.3 Z52.0 Z58.1 Z74.0 Z80.9 Z83. 0 Z83.3 Z85.9
Symptoms
Nephrotic syndrome and nephritic syndrome difference
Chest pain or cardialgia is the main clinical sign of ACS. This symptom occurs first, is paroxysmal in nature and radiates to the shoulder or arm. With angina, the pain is squeezing, burning, pressing, short-lived, and with a heart attack it is intense, stabbing and cutting, leading to painful shock and requiring immediate hospitalization. The pain is so severe that it prevents you from moving or breathing normally. Persons with ACS cannot find a comfortable position, rush about and are afraid of dying.
Anginal pain is often associated with previous physical or emotional stress. During a heart attack, it lasts more than an hour and brings severe suffering to the patient. With angina pectoris, the attack lasts ten minutes and is repeated periodically. The pain is practically not relieved by nitroglycerin. To relieve it, narcotic analgesics are used.
Symptoms that accompany chest pain and are not mandatory:
- Cold sweat,
- Fluctuations in blood pressure,
- Euphoria and motor overexcitation,
- Worry and anxiety
- Blackout,
- Panic and fear
- Presyncope or syncope,
- Pale skin
- Cyanosis of the nasolabial triangle,
- Shortness of breath, suffocation,
- Cough,
- Nausea and vomiting,
- Heartburn,
- Abdominal pain
- Dizziness,
- Causeless weakness.
The presented points are the basis of coronary syndrome. Manifestations of the disease may not be the same in all people. Their combination allows experienced specialists to quickly and correctly make a preliminary diagnosis. Symptoms may differ depending on the gender and age of the patient, the degree of circulatory disorders and the individual characteristics of the body, as well as the presence of concomitant diseases. Such a clinical picture should alert the patient and force him to see a doctor. You should take the symptoms of ACS very seriously, as this condition is life-threatening.
Treatment
The therapy program for patients with acute coronary syndrome is selected individually, depending on the severity of the pathological process; hospitalization and strict bed rest are required.
The patient’s condition may require measures to provide emergency first aid, which include the following:
- provide the patient with complete rest and access to fresh air;
- put a nitroglycerin tablet under your tongue;
- Call emergency medical services and report your symptoms.
Treatment of acute coronary syndrome in a hospital may include the following therapeutic measures:
- oxygen inhalation;
- administration of medications.
As part of drug therapy, the doctor may prescribe the following drugs:
- narcotic or non-narcotic painkillers;
- anti-ischemic;
- beta blockers;
- calcium antagonists;
- nitrates;
- disaggregants;
- statins;
- fibrinolytics.
In some cases, conservative treatment is not enough or is not appropriate at all. In such cases, the following surgical intervention is performed:
- stenting of the coronary arteries - a special catheter is passed to the site of narrowing, after which the lumen is expanded using a special balloon, and a stent is installed at the site of narrowing;
- coronary artery bypass grafting - the affected areas of the coronary arteries are replaced with shunts.
Coronary artery bypass grafting
Such medical measures make it possible to prevent the development of myocardial infarction from ACS.
In addition, the patient must follow general recommendations:
- strict bed rest until stable improvement;
- complete elimination of stress, strong emotional experiences, nervous tension;
- exclusion of physical activity;
- as the condition improves, daily walks in the fresh air;
- exclusion from the diet of fatty, spicy, too salty and other heavy foods;
- complete exclusion of alcoholic beverages and smoking.
You need to understand that acute coronary syndrome, if the doctor’s recommendations are not followed, can lead to serious complications at any time, and the risk of death in case of relapse always remains.
Separately, diet therapy for ACS should be highlighted, which implies the following:
- limiting the consumption of animal products;
- the amount of salt should be limited to 6 grams per day;
- exclusion of overly spicy, seasoned dishes.
It should be noted that compliance with this diet is necessary constantly, both during the treatment period and as a preventative measure.
Diagnostics
Vertebral artery syndrome with cervical osteochondrosis - symptoms. how to treat vertebral artery syndrome at home
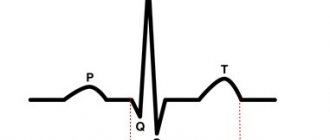
In an emergency, electrocardiography (ECG) is the most effective diagnostic test for angina. ECG changes that may be observed during anginal episodes include the following:
- Transitional ST segment elevations
- Dynamic T wave changes: inversions, normalizations, or hyperacute changes
- ST depressions: they can be connective, oblique or horizontal
Laboratory tests that may be helpful include the following:
- Study of levels of creatine kinase isoenzyme MB (CK-MB)
- Cardiac troponin level test
- Myoglobin level test
- General blood analysis
- Basic Metabolic Panel
Possible diagnostic methods that may be prescribed:
- Chest X-ray
- Echocardiography
- Myocardial perfusion tomography
- Cardiac angiography
- Computed tomography, including CT coronary angiography and CT analysis of the coronary artery
Development mechanism
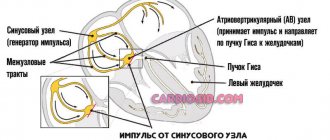
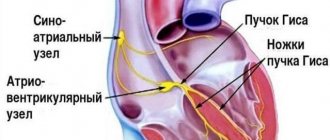
The essence of the pathological process is approximately the same, regardless of the type. As already mentioned, there are two types of the described situation: angina pectoris and heart attack. They are similar in nature.
In both cases, there is a disruption in the nutrition of the muscular layer of the heart as a result of stenosis or occlusion (blockage) of the coronary arteries. Often this is a consequence of atherosclerotic changes, less often congenital or acquired defects.
As a result of a decrease in blood flow intensity, toxins accumulate in the organ structures, which inhibit normal myocardial contractility.
On the other hand, the muscle layer cannot work due to ischemia. Accordingly, the chambers of the heart are also unable to function adequately. The left ventricle does not eject blood into the systemic circle with sufficient force.
Hence the drop in oxygen saturation, poor supply to the brain, distant organs and systems.
This situation is not normal. Over time, death inevitably occurs. Recovery requires urgent action.
Pathogenesis
ACS is a deadly condition that requires emergency medical care and emergency resuscitation measures. The disease, caused by primary damage to the coronary arteries or secondary changes in them, occurs in various clinical forms that have similar diagnostic and therapeutic features. The slightest delay or incorrect first aid actions can lead to death.
Pathogenetic links of ACS:
- Impact of etiological factors,
- Coronary thrombosis,
- Isolation of biologically active substances from platelets - thromboxane, histamine,
- Arterial spasm,
- A decrease in the intensity of blood flow in the heart,
- Deterioration of blood supply to the myocardium,
- Accumulation of toxins that inhibit contractility,
- Hyperproduction of adrenaline and calcium ions,
- Persistent narrowing of the coronary vessels,
- Blocking the anticoagulant system,
- The release of enzymes into the blood that destroy cells in the necrosis zone,
- Scar formation in the heart muscle
- Impaired contractile function of the heart,
- Inability of the heart chambers to function adequately,
- A drop in oxygen saturation,
- Poor nutrition of the brain, distant organs and systems.
The degree of blocking of the heart vessels by a plaque or thrombus largely determines the mechanism of development of the syndrome:
- Partial narrowing of the lumen - periodic attacks of angina pectoris,
- Complete occlusion - the appearance of dystrophic foci in the myocardium, quickly transforming into necrosis,
- Sudden ischemic changes—ventricular fibrillation and death.
The essence of the pathology, regardless of the type and form of the process, is a malnutrition of the heart muscle caused by stenosis or blockage of the coronary arteries. The main reason that triggers a complex cascade of pathogenetic reactions is atherosclerosis, congenital or acquired defects. Acute coronary syndrome over time can lead to the death of the patient. Recovery requires urgent action.
Other forms of acute coronary heart disease (I24)
Excluded:
- angina (I20.-)
- transient neonatal myocardial ischemia (P29.4)
Coronary (artery) (vein):
- embolism
- occlusion
- thromboembolism
https://www.youtube.com/watch?v=ytcopyrightru
not leading to myocardial infarction
Excluded: chronic coronary thrombosis or an established duration of more than 4 weeks (more than 28 days) from onset (I25.8)
Coronary:
- failure
- inferiority
In Russia, the International Classification of Diseases, 10th revision (ICD-10) has been adopted as a single normative document for recording morbidity, reasons for the population's visits to medical institutions of all departments, and causes of death.
ICD-10 was introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2017-2018.
With changes and additions from WHO.
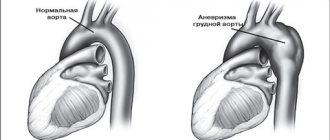
The acute form of coronary vascular insufficiency syndrome (ACS) can develop into a complicated form of pathology and appear with the following consequences:
- Heart muscle rhythm disorders - arrhythmia;
- Transition of pathology into an acute form of failure with a fatal outcome;
- Inflammation of the cardiac pericardium - pericarditis;
- The disease is an aortic aneurysm;
- Coronary artery rupture in ACS.
In order to prevent the transition of coronary insufficiency (ACS) to a complicated form of pathology, it is necessary to strictly follow all the recommendations of the treating doctor.
Possible complications
Acute coronary insufficiency syndrome can lead to the following:
- heart rhythm disturbance in any form;
- development of acute heart failure, which can lead to death;
- inflammation of the pericardium;
- aortic aneurysm.
It should also be understood that even with timely medical measures, there remains a high risk of developing the above complications. Therefore, such a patient should be systematically examined by a cardiologist and strictly follow all his recommendations.
Varieties
The use of the results of a comprehensive examination provides the basis for creating a classification of any ailment or pathology. OK syndrome is no exception.
To classify it, the results of the electrocardiogram are taken as a basis, and to be more precise, the position of the ST segment, which is clearly visible at the moment when the right and left cardiac ventricles are in the systole phase. Based on these indicators, there is the following division of syndrome types:
- The ST segment is in a raised position. This type is characterized by the development of lumen occlusion in the coronary artery.
- There is no elevation of the segment.
This classification is considered quite approximate. The reason for this is that it is impossible to draw a clear line between ischemic heart disease and unstable angina.
It is especially difficult to settle on one of the diseases at the initial stage. To do this, it is necessary to decipher the data obtained after the electrocardiogram.
Diagnostics
It is carried out under the supervision of a cardiologist. If the patient was transported to a hospital, there was minimal time for examination.
Limited to visual data and indicators of blood pressure and heart rate. Occasionally they resort to electrocardiography, but more often every minute counts.
The task is to first stabilize the patient, then engage in diagnostic research.
An approximate therapeutic regimen after restoration of body functions and relief of an attack:
- Oral questioning of the patient, collection of anamnesis.
- Measurement of blood pressure and heart rate. 24-hour Holter monitoring is much more effective. That is, recording indicators for 24 hours. It may be repeated.
- Electrocardiography. Assessment of functional activity of the heart.
- Echocardiography. Tissue visualization.
- General blood test, biochemical, hormones.
- Clinical examination of urine. First of all, we are interested in kidney function and the presence of sugar, as a sign of diabetes.
Unfortunately, most manifestations are smoothed out in bright moments. Only in case of relapse of coronary syndrome they are updated again.
Thrombolysis: what is it and why is it needed?
The term usually refers to the introduction into the patient’s body of a drug that can dissolve a blood clot. This procedure should begin within the first 120 minutes from the onset of ACS symptoms. Thrombolysis is carried out by strictly qualified doctors.
Streptokinase is used for intravenous administration. If 12 hours or more have passed since the onset of ACS, thrombolysis is absolutely ineffective - the formed blood clot cannot be dissolved with medications. Medicines containing streptokinase must be administered through a drip into a vein in a hospital setting. The best prognosis is for those patients who received the drug by drip in the first half hour after admission to the intensive care unit. It is unacceptable to perform the thrombolysis procedure under the following conditions:
- high blood pressure;
- previous stroke;
- bleeding;
- cranial injuries sustained in the last quarter of the year;
- the presence of a malignant neoplasm in the brain.
OKS: features
The pathological condition manifests itself as severe, acute pain. Seizures are possible. With angina pectoris, patients describe attacks as short-term, burning, as if the chest is squeezing. A heart attack is accompanied by a painful shock. The patient needs urgent hospitalization.
OKS manifests itself:
- cold sweat;
- excitement;
- panic fear;
- pale skin.
With such symptoms, it is important not only to call an ambulance in a timely manner, but also to stay with the patient until the doctors arrive. You should not leave the patient alone - this significantly increases the risk of death
You need to be especially attentive to a person who is nauseous and vomiting, as well as prone to loss of consciousness.
If, based on the results of assessing the patient’s condition, it was decided to resort to surgery, the most appropriate method for the case is chosen. Stenting is an intervention in which they identify where the artery is narrowed, insert a catheter using a small balloon, and expand the lumen of the blood vessel. For fixation, a stent is used - a special mesh that is not rejected by the tissues of the human body.
If bypass surgery is indicated, then part of the coronary arteries is removed and implants are installed instead. Timely and correctly performed surgery is the best way to prevent a heart attack.
Healing procedures
Acute coronary syndrome is a serious pathological condition that requires emergency medical care aimed at stabilizing the patient’s condition, preserving life and preventing further progression of myocardial ischemia and necrosis.
Before the ambulance arrives, the patient needs to measure blood pressure and pulse, open the window for fresh air, sit him down and give him Nitroglycerin. Currently, there are fast-acting remedies for relieving anginal pain - Nitromint and Nitrosorbide sprays. One injection under the tongue is enough to provide relief. The patient is monitored, excluding all possible risk factors.
Inpatient treatment is considered radical. It is selected individually, depending on the severity of the pathology. Patients are prescribed strict bed rest, oxygen inhalations, and medications. Diet therapy is of great importance. Patients should avoid animal products, fatty, spicy and salty foods.
Drug treatment regimen for a patient with ACS:
- Narcotic or non-narcotic painkillers - “Morphine”, “Fentanyl”, “Promedol”,
- Beta blockers – “Atenolol”, “Propranolol”, “Metoprolol”,
- Calcium antagonists - Nifedipine, Amlodipine, Verapamil,
- Nitrates – “Nitroglycerin”, “Erinit”, “Nitromint”,
- Disaggregants – “Plavix”, “Aspirin-Cardio”, “Cardiomagnyl”,
- Statins – “Atoris”, “Simvastatin”, “Cardiostatin”,
- Fibrinolytics – “Urokinase”, “Fibrinolysin”,
- Cardioprotectors - Mildronate, Riboxin, Preductal.
If there is no effect from conservative therapy, patients undergo surgery:
- Stenting of the coronary arteries - expansion of the lumen of the vessel using a balloon and installation of a stent in the narrowed vessel,
- Coronary artery bypass grafting is the replacement of affected areas of blood vessels with special shunts, the creation of an alternative route for blood flow bypassing pathologically altered arteries, and the restoration of coronary circulation.
There are traditional medicine recipes that improve the trophism of the heart muscle. These include: decoctions of nettle or eryngium, infusion of centaury or oat grains.
Experts give patients clinical recommendations that allow the body to recover faster from illness and prevent relapse of the syndrome:
- Eliminate psycho-emotional stress,
- Limit physical activity
- Take a walk in the fresh air every day,
- Eat properly,
- Don't drink or smoke,
- Lead a healthy lifestyle,
- Normalize body weight,
- Monitor blood pressure, cholesterol and blood sugar levels.
Establishing diagnosis
Patients with suspected ACS are examined, their complaints are analyzed, the heart is auscultated and percussed, and blood pressure and pulse are measured.
Electrocardiographic examination is the main diagnostic method for ACS. An ECG should be done as soon as possible after the onset of cardialgia. This technique involves recording the electrical activity of the heart using electrodes attached to the skin. First, electrical impulses in the form of waves are displayed on a monitor and then printed on paper. When the myocardium is damaged, its conductive function is impaired. The ECG shows the form of ACS - angina or heart attack.
As soon as the patient’s condition becomes satisfactory, you can move on to a full diagnostic program, including:
- 24-hour Holter monitoring – measuring blood pressure and pulse over 24 hours.
- General blood test, blood for hormones - general examination of the body.
- Clinical examination of urine to determine the functional state of the kidneys.
- BAC - detection of the level of cholesterol, glucose, as well as enzymes that, during the development of myocardial infarction, are released from damaged cardiomyocytes into the blood.
- Coagulogram is an assessment of the functional state of the blood coagulation system.
- Echocardiography is an ultrasound examination of the heart to detect lesions. Ultrasound waves are sent from the device's sensor to the heart and then returned back. The received signals are processed by a computer, and a video image is formed on the monitor screen.
- X-ray examination of the chest cavity - determining the size and shape of the heart and large blood vessels.
- Coronary angiography is an invasive test that identifies the location and extent of narrowing or occlusion of the coronary arteries. A long catheter is inserted into the heart vessels through the large arteries of the arms or legs. The vascular bed is filled with a liquid contrast agent and a series of x-rays are taken, in which the areas of narrowing are clearly visible. During the catheter procedure, the doctor can use tiny balloons to relieve the narrowing. They are introduced into the affected vessel and inflated. At the same time, the narrowing expands and the occlusion is eliminated. To prevent repeated spasm, a stent - a mesh tubular frame - is installed in the artery.
- Scintigraphy – detection of coronary blood flow disorders. Radioactive substances are injected into the blood, and special cameras monitor their uptake by the myocardium. Thus, where blood flow is obstructed, less radioactive material passes through. In the resulting image, such zones appear as dark spots.
- Computed tomography with contrast is performed in difficult diagnostic cases when other methods cannot determine the cause of anginal pain. Before the examination, the patient is injected with a contrast agent intravenously, and then the CT scanner takes a series of images, from which the computer creates a three-dimensional image of the heart. CT scans allow doctors to evaluate the condition of the arteries and detect narrowing or blockages in them.
- Bicycle ergometry is a stress test that is performed after acute signs of cardiac pathology have been removed. This technique allows you to determine the reaction of the heart and blood vessels to physical stress.
- Pulse oximetry - determining the level of oxygen in the blood.
ACS on ECG
All diagnostic measures are carried out under the constant supervision of a cardiologist. If the patient’s condition is serious, he is not examined comprehensively, but is limited only to visual examination data, pulse and pressure indicators, and ECG results. After stabilizing the patient’s well-being, they proceed to diagnostic measures.
Etiology
Various provoking factors and pathological processes lead to the development of acute coronary syndrome.
Atherosclerosis of the coronary arteries is the main cause of the disease. The fatty substances that form the plaque narrow the blood vessels and impede the flow of blood through the narrowed area. The heart stops fully pumping oxygen-rich blood. This leads to chest pain and heart attack. At early stages of the process, lipid structures are highly soluble. As the pathology progresses, they calcify and become rock-hard. You can only get rid of such formations surgically.
When the surface of an atherosclerotic plaque ruptures, a blood clot forms at the site of damage, the lumen of the vessel narrows, and its patency is impaired. These morphological elements of the disease reduce coronary blood flow and disrupt the blood supply to the myocardium. Blood stops circulating normally, and the heart rate increases to compensate for the resistance. Patients' blood pressure rises and their pulse quickens. If the blood flow completely stops due to a plaque or thrombus blocking the vascular lumen, an irreversible process develops - myocardial infarction, and generalized vascular dysfunction occurs.
Currently, there is no unified theory of the origin of acute coronary syndrome. Using statistical and experimental data, scientists were able to identify the main factors that most often lead to the development of coronary diseases.
Factors that trigger the atherosclerotic process and predispose to the development of the syndrome:
- Stress, psycho-emotional stress, nervous shock,
- Persistent spasm of blood vessels of various origins,
- Postoperative complications
- Coronary artery embolism,
- Inflammation of the vascular wall,
- Congenital anomalies of cardiac structures,
- Overweight,
- Smoking,
- Drug use
- Lack of physical activity
- Imbalance of fats in the blood,
- Alcoholism,
- Genetic predisposition to cardiovascular pathologies,
- Increased blood clotting
- High blood pressure,
- Diabetes,
- Autoimmune or infectious vasculitis,
- General hypothermia of the body,
- Taking certain medications
- Age over 55 years.
There are secondary provoking factors that lead to the development of ACS and are not associated with ischemia of the heart muscle. These are non-atherosclerotic causes of the disease that can cause myocardial infarction. These include:
- Traumatic injury
- Long-term insolation,
- Hyperfunction of the thyroid gland,
- Arteritis.
How to warn?
Prevention of ACS involves giving up bad habits and switching to a limited diet with the exception of fatty, salty, and spicy foods. You should constantly give yourself physical activity, avoid stress and overwork. Persons for whom the risk of ACS is increased is recommended to go for walks on weekends, you can even go on non-sports hikes - these are regularly organized by amateurs in almost any city in our country.
Persons classified as at risk for ACS should have a tonometer at home and monitor blood pressure readings, and regularly donate blood to detect cholesterol concentrations. At the appointment, the therapist will tell you which specialized doctors you will need to see for examination, and how often you need to visit doctors. To prevent ACS, you will have to follow the advice. Any identified diseases, especially those affecting the blood vessels and heart, must be treated promptly.
Prevention
You can prevent the development of cardiovascular diseases if you follow the following doctor’s recommendations in practice:
- complete cessation of smoking, moderate consumption of alcoholic beverages;
- proper nutrition;
- moderate physical activity;
- daily walks in the fresh air;
- elimination of psycho-emotional stress;
- control of blood pressure indicators;
- control blood cholesterol levels.
In addition, we should not forget about the importance of a preventive examination by specialized medical specialists and compliance with all doctor’s recommendations regarding the prevention of ailments that can lead to acute coronary insufficiency syndrome.
Application of a minimum of recommendations in practice will help prevent the development of complications caused by acute coronary syndrome.
Diagnosis of acute coronary syndrome
The diagnosis of acute coronary syndrome is made when there is not yet sufficient information for a final judgment about the presence or absence of foci of necrosis in the myocardium. This is a working and legitimate diagnosis in the first hours and days from the onset of the disease.
The diagnoses of “myocardial infarction” and “unstable angina” are made when there is enough information to make them. Sometimes this opportunity is already available during the initial examination, when electrocardiography and laboratory test data make it possible to determine the presence of foci of necrosis. More often, the possibility of differentiating these conditions appears later, then the concepts of “myocardial infarction” and various variants of “unstable angina” are used when formulating the final diagnosis.
The defining criteria for the diagnosis of acute coronary syndrome at the initial stage are the clinical symptoms of an anginal attack and electrocardiography data, which should be performed within the first 10 minutes after the first visit. Subsequently, based on the electrocardiographic picture, all patients are divided into two groups:
- patients with acute coronary syndrome with ST segment elevation;
- patients with acute coronary syndrome without ST segment elevation. This division determines further treatment tactics.
It should be remembered that a normal electrocardiogram in patients with symptoms suggestive of acute coronary syndrome does not exclude it. It should also be taken into account that in young (25-40 years) and elderly (> 75 years) patients, as well as patients with diabetes mellitus, manifestations of acute coronary syndrome may occur without a typical anginal status.
The final diagnosis is most often made retrospectively. It is almost impossible to predict at the initial stages of the disease how an exacerbation of coronary heart disease will end - stabilization of angina, myocardial infarction, sudden death.
The only method for diagnosing one or another variant of ACS is recording an ECG. When ST segment elevation is detected, myocardial infarction with a Q wave develops in 80-90% of cases. In patients without persistent ST segment elevation, ST segment depression, negative T waves, pseudonormalization of inverted T waves, or ECG changes are absent (in addition, approximately 10% of patients with ACS without persistent ST elevation experience episodes of transient ST segment elevation). The probability of myocardial infarction with a Q wave or death within 30 days in patients with ST segment depression averages about 12%, with negative T waves - about 5%, in the absence of ECG changes - from 1 to 5%.
[], [], [], [], [], []
Myocardial infarction with Q wave
Myocardial infarction with a Q wave is diagnosed by ECG (appearance of a Q wave). To detect MI without a Q wave, it is necessary to determine markers of myocardial necrosis in the blood. The method of choice is to determine the level of cardiac troponins T or I. In second place is the determination of the mass or activity of the MB fraction of creatine phosphokinase (MB CPK). A sign of MI is considered to be a troponin T level of more than 0.1 µg/l (troponin I - more than 0.4 µg/l) or an increase in CPK MB by 2 times or more. In approximately 30% of patients with increased levels of troponins in the blood (“troponin-positive” patients), CPK MB is within normal limits. Therefore, when using troponin determination, the diagnosis of MI will be made in a larger number of patients than when using MB CPK. It should be noted that an increase in troponins can also be observed in non-ischemic myocardial damage, for example, in PE, myocarditis, heart failure and chronic renal failure.
For rational implementation of treatment measures, it is advisable to assess the individual risk of complications (MI or death) in each patient with ACS. The level of risk is assessed by clinical, electrocardiographic, biochemical parameters and response to treatment.
The main clinical signs of high risk are recurrent myocardial ischemia, hypotension, heart failure, and severe ventricular arrhythmias.
ECG: low risk - if the ECG is normal, without changes or there are minimal changes (reduced T wave, T wave inversion less than 1 mm deep); intermediate risk - if there is ST segment depression of less than 1 mm or negative T waves of more than 1 mm (up to 5 mm); high risk if there is transient ST segment elevation, ST depression greater than 1 mm, or deep negative T waves.
Troponin T level: less than 0.01 mcg/l - low risk; 0.01-0.1 µg/l - intermediate risk; more than 0.1 µg/l – high risk.
The presence of high-risk signs is an indication for an invasive treatment strategy.
[], [], [], [], [], []
Forecast
The prognosis for ACS is ambiguous. It depends on the impact of provoking factors, the general condition of the body, age, existing concomitant diseases and structural and functional disorders of the cardiovascular system.
- The prognosis for unstable angina is determined by the location of the lesion: narrowing of the proximal arteries ends in death, and the distal ones are more favorable. With the development of left ventricular failure, the prognosis becomes more complicated.
- Myocardial infarction with ST segment elevation has a benign course. In the absence of this ECG sign, the area of the lesion is important - the larger it is, the more severe the patient’s condition.
Acute coronary syndrome is a dangerous pathology that, if medical instructions are not followed, can lead to serious complications: arrhythmia, persistent cardiac dysfunction, pericarditis, rupture of the dilated aorta, cardiac arrest, stroke, cardiogenic shock, and death. Even with timely and adequate treatment, there remains a high risk of complications. To avoid this, you need to monitor your health, regularly visit a cardiologist and strictly follow all his recommendations.