Chest pain can occur due to various diseases; it is sometimes difficult even for a doctor to understand it right away, so patients with such complaints usually undergo additional examination. Chest pain can manifest as diseases of the heart, respiratory system, gastrointestinal tract, spine, mediastinum, and central nervous system. All human internal organs are innervated by the autonomic nervous system, the trunks of which arise from the spinal cord. When approaching the chest, the nerve trunk gives off branches to individual organs. That is why sometimes pain in the stomach can be felt like pain in the heart - they are simply transmitted to the common trunk, and from it to another organ. Moreover, the spinal nerve roots contain sensory nerves that innervate the musculoskeletal system. The fibers of these nerves are intertwined with the fibers of the nerves of the autonomic nervous system, and therefore a completely healthy heart can respond with pain in various diseases of the spine.
Finally, chest pain may depend on the state of the central nervous system: with constant stress and high neuropsychic stress, a malfunction occurs in its functioning - neurosis, which can also manifest itself as pain in the chest.
Some chest pains are unpleasant, but not life-threatening, but there are chest pains that need to be relieved immediately - a person’s life depends on it. In order to figure out how dangerous chest pain is, you need to see a doctor. Perhaps this will save your life or calm you down if no serious problems with your health are found.
Causes of chest pain
- Heartburn. Acidic stomach acid that flows from the stomach into the esophagus (the tube that connects the mouth to the stomach) can cause heartburn, a painful burning sensation in the chest. It is often combined with a sour taste and belching. Heartburn chest pain is usually associated with food intake and can last for hours. This symptom most often occurs when bending or lying down. Taking antacids relieves heartburn.
- Panic attacks. If you experience attacks of unreasonable fear, combined with chest pain, rapid heartbeat, hyperventilation (rapid breathing) and profuse sweating, you may be suffering from “panic attacks” - a unique form of dysfunction of the autonomic nervous system.
- Pleurisy. Sharp, localized chest pain that gets worse when you inhale or cough may be a sign of pleurisy. The pain occurs due to inflammation of the membrane lining the inside of the chest cavity and covering the lungs. Pleurisy can occur with various diseases, but most often with pneumonia.
- Tietze syndrome. Under certain conditions, the cartilaginous parts of the ribs, especially the cartilage that attaches to the sternum, can become inflamed. Pain in this disease can occur suddenly and be quite intense, simulating an attack of angina. However, the location of pain may vary. With Tietze syndrome, pain may increase when pressure is placed on the sternum or ribs near the sternum. Pain during angina pectoris and myocardial infarction does not depend on this.
Osteochondrosis of the cervical and thoracic spine leads to so-called vertebrogenic cardialgia, which resembles angina pectoris. In this condition, there is intense and prolonged pain behind the sternum, in the left half of the chest. There may be irradiation into the arms and interscapular area. The pain increases or decreases with changes in body position, head turns, and arm movements. The diagnosis can be confirmed by performing an MRI of the spine. Magnetic resonance imaging of the spine will help determine the cause of pain in the chest if it is caused by pinched nerve roots or the presence of herniated intervertebral discs.
- Pulmonary embolism. This type of embolism occurs when a blood clot enters the pulmonary artery, blocking the flow of blood to the heart. Symptoms of this life-threatening condition may include sudden, sharp chest pain that occurs or gets worse with deep breathing or coughing. Other symptoms are shortness of breath, palpitations, anxiety, loss of consciousness.
- Other lung diseases. Pneumothorax (collapsed lung), high pressure in the blood vessels supplying the lungs (pulmonary hypertension), and severe asthma may also cause chest pain.
- Muscle diseases. Pain caused by muscle diseases usually begins to bother you when you turn your body or raise your arms. Chronic pain syndrome such as fibromyalgia. May cause persistent chest pain.
- Damage to ribs and pinched nerves. Bruises and fractures of the ribs, as well as pinched nerve roots, can cause pain, sometimes very severe. With intercostal neuralgia, pain is localized along the intercostal spaces and intensifies with palpation.
- Diseases of the esophagus. Some diseases of the esophagus can cause difficulty swallowing and therefore chest discomfort. Esophageal spasm can cause chest pain. In patients with this disease, the muscles that normally move food down the esophagus work uncoordinated. Since esophageal spasm can resolve after taking nitroglycerin - just like angina - diagnostic errors often occur. Another swallowing disorder known as achalasia can also cause chest pain. In this case, the valve in the lower third of the esophagus does not open as it should and does not allow food to pass into the stomach. It remains in the esophagus, causing discomfort, pain and heartburn.
- Shingles. This infection, caused by the herpes virus and affecting the nerve endings, can cause severe chest pain. The pain can be localized in the left half of the chest or be of a girdling nature. This disease can leave behind a complication - postherpetic neuralgia - the cause of prolonged pain and increased skin sensitivity.
- Diseases of the gallbladder and pancreas. Gallstones or inflammation of the gallbladder (cholecystitis) and pancreas (pancreatitis) can cause pain in the upper abdomen that radiates to the heart.
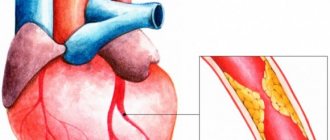
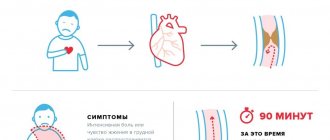
- Myocardial infarction - a blood clot that blocks the movement of blood in the arteries of the heart can cause pressing, squeezing chest pain that lasts more than a few minutes. The pain can radiate to the back, neck, lower jaw, shoulders and arms (especially the left). Other symptoms may include shortness of breath, cold sweats, and nausea.
- Angina pectoris. Over the years, fatty plaques can form in the arteries of your heart, limiting the flow of blood to the heart muscle, especially during exercise. It is the restriction of blood flow through the arteries of the heart that causes attacks of chest pain - angina. Angina is often described by people as a feeling of tightness or tightness in the chest. It usually occurs during physical activity or stress. The pain usually lasts about a minute and goes away with rest.
- Other causes of chest pain include inflammation of the lining of the heart (pericarditis), most often due to a viral infection. Pain with pericarditis is most often acute, stabbing in nature. Fever and malaise may also occur. Less commonly, the pain may be caused by a dissection of the aorta, the main artery in your body. The inner layer of this artery can separate under blood pressure and the result is sharp, sudden and severe pain in the chest. Aortic dissection can be the result of chest trauma or a complication of uncontrolled hypertension.
Because chest pain can have many different causes, do not self-diagnose, self-medicate, or ignore severe or prolonged pain. The cause of your pain may not be so serious - but in order to establish it, you need to contact a specialist.
When should you see a doctor?
Pain in the heart area is a dangerous symptom that always requires additional diagnostics and a search for its causes. It is important to understand that diseases of all organs and systems require appropriate attention and treatment. But in some cases, you can independently determine the danger of a developing condition.
For the first time in life, an acute attack of pain in the heart area always requires contacting emergency medical services. The same applies to people with previously diagnosed angina pectoris (a form of angina in which pain occurs only against the background of a trigger and is eliminated by taking nitroglycerin) if taking a previously effective dose of nitrates did not relieve the pain within 15 minutes of taking the drug.
The absence of a serious danger may be indicated by pain or discomfort behind the sternum, which occurs immediately after a sharp turn or tilt of the body, eating or taking a horizontal position after eating. This also includes short-term attacks of mild pain that occur against the background of strong experiences or stressful situations. In such cases, a scheduled visit to the doctor is recommended.
Important! Regardless of the characteristics of the pain, the presence or absence of radiation, other symptoms or provoking factors, diagnosis is necessary. Only a doctor's examination, laboratory tests, ECG and other studies can help accurately determine the origin of pain and exclude life-threatening conditions.
Chest pain caused by changes in the central nervous system
Chest pain can also occur with other diseases. One of the most common diseases that causes frequent and prolonged pain in the chest is cardioneurosis, which develops against the background of a temporary functional disorder of the central nervous system. Neuroses are the body’s response to various mental shocks (intense, short-term or less intense, but long-lasting).
Pain due to cardioneurosis can have a different character, but most often it is constant, aching and is felt in the area of the apex of the heart (in the lower part of the left half of the chest). Sometimes pain due to cardioneurosis may resemble pain due to angina pectoris (short-term acute), but taking nitroglycerin does not relieve it. Often attacks of pain are accompanied by reactions from the autonomic nervous system in the form of facial flushing, moderate heartbeat, and a slight increase in blood pressure. With cardioneurosis, other signs of neuroses are almost always present - increased anxiety, irritable weakness, etc. Helps with cardioneurosis are the elimination of traumatic circumstances, the correct daily routine, sedatives, and for sleep disorders - sleeping pills.
Sometimes cardioneurosis is difficult to distinguish from coronary heart disease (CHD); the diagnosis is usually made based on careful observation of the patient, since there may be no changes on the ECG in either case.
A similar picture can be caused by changes in the heart during menopause. These disorders are caused by changes in hormonal levels, resulting in neurosis and metabolic disorders in the heart muscle (menopausal myocardiopathy). Pain in the heart is combined with the characteristic manifestations of menopause: flushing of the face, bouts of sweating, chills and various sensory disturbances in the form of “goosebumps”, insensitivity of certain areas of the skin, etc. Just as with cardioneurosis, heart pain is not relieved by nitroglycerin; sedatives and hormone replacement therapy help.
How to assess lung function after coronavirus?
A breath test should be performed. You can do it yourself at home:
- take a deep breath through your nose,
- hold your breath for ten seconds,
- exhale slowly.
In the absence of any discomfort, cough or sore throat, the lungs are healthy. If your health worsens and these symptoms occur, you should immediately seek medical help. You can find a video on the forum on how to properly do a lung assessment.
Chest pain due to diseases of the spine and ribs
Chest pain, very similar to heart pain, can occur with various diseases of the spine, for example, with osteochondrosis, herniated discs, ankylosing spondylitis, etc. Osteochondrosis is dystrophic (metabolic) changes in the spine. As a result of poor nutrition or high physical activity, bone and cartilage tissue, as well as special elastic pads between individual vertebrae (intervertebral discs), are gradually destroyed. Such changes cause compression of the spinal nerve roots, which causes pain. If changes occur in the thoracic spine, the pain may be similar to pain in the heart or pain in the gastrointestinal tract. The pain can be constant or in the form of attacks, but it always intensifies with sudden movements. Such pain cannot be relieved with nitroglycerin or antispasmodics; it can only be relieved by painkillers or heat. Pain in the chest area can occur when a rib is fractured. These pains are associated with injury and intensify with deep breathing and movement.
Prevention
Prevention of pain in the heart area when inhaling is complex and is aimed at strengthening the entire body as a whole and the cardiovascular system in particular. First of all, this is a healthy lifestyle: a rational schedule of work and rest, proper nutrition and moderate physical activity. Cardio training and yoga help control breathing and strengthen the heart muscle.
However, if you have concomitant diseases, it is important to coordinate all your actions with your doctor. For example, the doctor will help you control the level of fat and cholesterol you consume. This is important because they are part of cell membranes, and completely avoiding their consumption can be harmful.
Chest pain due to lung diseases
The lungs occupy a significant part of the chest. Chest pain can occur against the background of inflammatory diseases of the lungs, pleura, bronchi and trachea, with various injuries to the lungs and pleura, tumors and other diseases.
Chest pain occurs especially often when there is a disease of the pleura (the serous sac that covers the lungs and consists of two layers, between which the pleural cavity is located). With inflammation of the pleura, pain is usually associated with coughing, deep breathing and accompanied by fever. Sometimes such pain can be confused with heart pain, for example, with pain due to pericarditis. Very severe chest pain occurs when lung cancer grows in the pleural area.
In some cases, air (pneumothorax) or fluid (hydrothorax) enters the pleural cavity. This can happen with a lung abscess, pulmonary tuberculosis, etc. With spontaneous (spontaneous) pneumothorax, sharp sudden pain appears, shortness of breath, cyanosis, and blood pressure decreases. The patient has difficulty breathing and moving. The air irritates the pleura, causing severe stabbing pain in the chest (in the side, on the affected side), radiating to the neck, upper limb, and sometimes to the upper abdomen. The patient's chest volume increases and the intercostal spaces widen. Help for such a patient can only be provided in a hospital.
Sources
- Trukhan D.I., Davydov E.L. “Chest pain: current issues in clinical diagnosis and treatment of angina” // Consilium Medicum – No. 17(10) – 2015.
- Yu. V. Vasiliev “Pain behind the sternum: differential diagnosis, treatment” // Cardiology - 2006.
- Ruigomez A., Rodriguez LA, Wallander MA et al “Chest pain in general practice: incidence, comorbidity and mortality” // Fam. Pract. – Vol. 23 – 2006
- A.N. Belovol, I.I. Knyazkova “Clinical approaches to the diagnosis of chest pain” // Current preparations and technologies – No2 (78) – 2011 r.
- Nilsson S., Scheike M., Engblom D. et al. “Chest pain and ischemic heart disease in primary care” // Br. J.Gen. Pract. – Vol. 53 – 2003.
Self-diagnosis problems
Difficulty breathing, for example, during nasal congestion and when the functioning of the lungs is impaired, are completely different things. It is impossible to figure out the cause of shortness of breath on your own.
treatment of shortness of breath due to coronavirus
You should seek medical help from your family doctor or pulmonologist. You should not self-medicate.
Treatment of shortness of breath after suffering from covid-19
Shortness of breath after coronavirus, what to do ? If you have difficulty taking a deep breath, after additional diagnostics, doctors prescribe:
- drug therapy,
- oxygen therapy,
- inhalations,
- physiotherapy,
- breathing exercises.
Later in the article we will talk in more detail about each treatment method.
Medicines for shortness of breath
Many people are interested in the question: how to treat shortness of breath with coronavirus ? To relieve symptoms, doctors prescribe drugs from the following groups:
- bronchodilators,
- expectorants,
- antiviral drugs,
- immunomodulators,
- antibacterial drugs.
The doctor selects the drug and its dosage individually depending on the severity of the symptoms, the clinical picture and the presence of concomitant pathology in the individual patient.
Oxygen therapy (oxygenation)
It is an oxygen inhalation, which is used in case of shortness of breath without coronavirus . Oxygen is introduced into a person's respiratory tract using a special tube.
Oxygenation is used only in patients with severe forms of pathology, with extensive lung damage. If all medical recommendations are followed, the risk of such complications is minimal.
Inhalation therapy
It is used using a Nebulizer, which allows you to administer drugs in the form of microparticles dissolved in the air into the patient’s respiratory tract. A good effect can be achieved by using:
- phlegm thinners,
- sea water,
- saline solutions,
- antiseptics,
- bronchodilators,
- expectorants.
This method should be used only as prescribed by a doctor so as not to harm the functioning of the lungs.
Physiotherapy
In order to accelerate the resorption of pathological foci and relieve inflammation after suffering from covid-19, the following should be carried out:
- chest massage,
- electrophoresis,
- SMT,
- UHF therapy.
Please note that you should complete the full course of procedures to achieve a good treatment result.
Breathing exercises
It is worth doing the exercise both during the disease itself and after it has been cured and a negative test has been received. These exercises will strengthen your chest muscles and increase blood flow to your lungs.
Can I improve my lung function on my own?
Can! There are quite simple methods for this:
- It is necessary to consume fresh vegetables and fruits as much as possible. Tomatoes, blueberries, nuts, onions and citrus fruits are especially beneficial for the lungs. Fatty foods, spices and smoked foods should be avoided.
- You shouldn't smoke. Tobacco smoke provokes the occurrence of inflammatory diseases, while the resistance of the lungs to viral and bacterial pathologies weakens. The relationship between tobacco smoke and the occurrence of cancer has also been proven. To speed up the process of recovery of lung tissue, you should abstain from smoking.
- Cardio exercise (this can be jogging at a moderate speed, walking at speed, jumping rope). They should be performed if you feel well. They help strengthen the heart muscle, normalize blood circulation, increase the respiratory volume of the lungs and build endurance. Training should be done outdoors. Increase the load gradually. If you feel the slightest deterioration in health, the training should be interrupted.
- Eliminate negative environmental factors and smoke. After suffering from covid-19 with accompanying symptoms ( shortness of breath, coronavirus pneumonia ) in the early period after the disease, you should not be in polluted conditions. If there are harmful professional conditions, it is better to take a vacation. Spend more time outdoors, ideally visit a sanatorium or health resort in a pine forest or on the seashore.
Anyone who listens to the doctor’s recommendations, takes medications on time, eats right, engages in dosed physical activity and walks in the fresh air will quickly get rid of the consequences of covid-19. Be attentive to your health and seek specialized medical help when the first symptoms of illness appear.