General information about the disease
Arterial hypertension (AH) affects a significant portion of the world's population (1 billion people, according to WHO).
Arterial hypertension is divided into two groups.
Essential (primary) hypertension
This is an independent pathology that develops against the background of the patient’s general good health. Causes:
- heredity;
- lack of physical activity;
- passive lifestyle;
- improper study and rest regime;
- constant stress, which develops against the background of increased psychological stress (poor relationships with peers, poor performance despite great effort, etc.);
- disrupted metabolic processes. Source: I.P. Bryazgunov Primary arterial hypertension in children and adolescents // Issues of modern pediatrics, 2003, vol. 2, no. 3, pp. 68-71
Essential hypertension usually develops after 6 years of age. Often the impetus for the development of the disease is stress at school, problems in the family, or a strong quarrel. Children who have this disease are prone to increased anxiety, depression, and fearfulness.
Hypertension also occurs in adolescents who start smoking and drinking alcohol.
Symptomatic (secondary) hypertension
This form of pathology manifests itself against the background of:
- kidney diseases;
- disturbances in the functioning of the endocrine system;
- taking medications that interfere with maintaining blood pressure at the desired level and/or raise it;
- neurological disorders.
The disease is dangerous due to many complications, including:
- hypertensive crisis (can lead to loss of consciousness);
- blood clots in blood vessels;
- heart failure;
- stroke;
- myocardial infarction;
- deterioration of vision due to damage to the blood vessels of the fundus;
- renal failure.
In the vast majority of cases, children develop hypertension of the second type - symptomatic . Its main cause at an early age is kidney pathologies (anomalies in vascular development, autoimmune pathologies, underdeveloped kidneys, Wilms tumor). Also common in children are: bronchopulmonary dysplasia, obstructive sleep apnea syndrome (stopping for 10 seconds or more or a sharp slowdown in breathing during sleep against the background of snoring), closure or narrowing of the aortic lumen. Source: N.N. Arkhipova Secondary arterial hypertension in children // Practical Medicine, 2011, No. 5(53), pp. 20-24
Among the youngest children at risk are children with diseases of the ENT organs (chronic tonsillitis, adenoids), obesity, and pathologies of the skull. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860989/ Anusha Uddaraju and C. Venkata S. Ram Hypertension in children, not a “small” problem // Indian Heart J. 2013 Sep; 65(5): 501–503.
Often in children and adolescents, blood pressure rises sharply, which can be accompanied by convulsions, headache, nausea and vomiting. Such an attack can easily be confused with a migraine, which the child may “outgrow,” so parents are not always vigilant enough. It is very important to measure blood pressure at such times.
Figures of increased systolic pressure at different ages
| Blood pressure, mmHg | Child's age |
| From 104 | From a week to 1 month |
| From 112 | From a month to 2 years |
| From 116 | From 3 to 6 years |
| From 122 | From 6 to 10 years |
| From 126 | From 10 to 13 years |
| From 136 | From 13 to 16 years old |
| From 142 | From 16 to 18 years old |
Remember that a home blood pressure monitor does not give accurate results. Therefore, if you have symptoms, you should consult a doctor, and in case of a severe attack, call an ambulance.
Diagnosis and treatment of arterial hypertension in childhood
Arterial hypertension (AH) is a major socioeconomic and medical problem, remaining the main risk factor for coronary heart disease and brain diseases, the share of mortality from which in the structure of overall mortality exceeds 50%.
Numerous clinical and epidemiological studies have established that the “origins” of hypertension are in childhood and adolescence. Hypertension is registered in 4% to 18% of children, depending on the age group and selected diagnostic criteria. In the absence of timely prevention and adequate therapy, hypertension transforms into hypertension in 30–40% of cases [1, 2, 3].
In accordance with the recommendations of the American Working Group on High Blood Pressure in Children and Adolescents, experts from the All-Russian Scientific Society of Cardiologists, the Association of Pediatric Cardiologists of Russia and the Russian Medical Society for Arterial Hypertension, the normal level of blood pressure (BP) in children is considered to be the value of systolic blood pressure (SBP) and diastolic Blood pressure (DBP) is less than the 90th percentile for the corresponding age, sex and height (see table on pages 34–35) “SBP and DBP levels in boys aged 1 to 17 years depending on the height percentile distribution” and “SBP and DBP levels in girls aged 1 to 17 years depending on the height percentile distribution”). To indicate a SBP or DBP level between the 90th and 95th percentile, or greater than 120/80 mmHg. Art., but not exceeding the 95th percentile, the concept of “high normal blood pressure” was introduced. Blood pressure values exceeding the 95th percentile are taken as hypertension [4, 5].
In establishing the diagnosis of hypertension in pediatrics, special tables are used based on the results of population studies, and the diagnostic process itself consists of the following stages:
- determination of the height percentile corresponding to the patient’s sex and age using special tables (
) [6]; - calculation of average SBP and DBP values based on three blood pressure measurements taken at intervals of several minutes;
- comparison of the average values of the patient's SBP and DBP, obtained from the results of three measurements of blood pressure at one visit, with the 90th and 95th percentiles of blood pressure corresponding to the patient's gender, age and height percentile;
- comparison of the average values of SBP and DBP recorded for the patient at three visits with an interval between visits of 10–14 days, with the 90th and 95th percentiles of blood pressure corresponding to the patient’s sex, age and height percentile [5].
If three average values of SBP and DBP, determined at three visits with an interval of 10–14 days, meet the criteria for normal BP, high normal BP or hypertension, an appropriate diagnosis is established [4].
In children and adolescents, it is advisable to distinguish two stages of hypertension:
- Stage I - average SBP and/or DBP levels are in the range from the 95th percentile to the 99th percentile plus 5 mmHg. Art. for the corresponding sex, age and height percentile.
- Stage II - average levels of SBP and/or DBP are more than 5 mm Hg above the 99th percentile. Art., for the corresponding sex, age and height percentile [5].
The stage of hypertension is established by a higher value of systolic or diastolic blood pressure and is determined in patients not receiving antihypertensive therapy.
The classification of hypertension is based on the identification of primary or essential hypertension and secondary or symptomatic forms of high blood pressure. The latter are caused by renal, endocrine, neurogenic and cardiovascular etiology, and in their therapy the treatment of the underlying disease comes to the fore. The most common known causes of hypertension, in order of their relative prevalence in different age periods, are presented in
[7]. Approximately 60–80% of secondary hypertension are caused by parenchymal renal diseases [7]. According to most experts, the term essential hypertension is a misnomer, implying that high blood pressure is somehow an essential component of the patient's life. Due to its imprecision, this term is not currently used.
Correct diagnosis and differential diagnosis of the disease is based on a thorough history taking, detailed clinical examination and the use of modern laboratory and instrumental research methods.
When collecting anamnesis, you should pay attention to the following information:
- complaints (headache, vomiting, sleep disturbances);
- blood pressure level and duration of hypertension;
- pathology of pregnancy and childbirth;
- traumatic brain injury and abdominal injury;
- premature sexual development (appearance of secondary sexual characteristics in girls under 8 years old, in boys under 10 years old);
- pyelonephritis (can be assumed by episodes of unmotivated increase in body temperature, a history of leukocyturia, dysuria);
- previous antihypertensive therapy;
- excessive consumption of table salt (tendency to add salt to already cooked food), changes in body weight, level and nature of physical activity;
- drinking alcohol, smoking;
- family history of hypertension, other cardiovascular diseases, diabetes mellitus (the presence of these diseases in parents aged <55 years);
- psychological and environmental factors: the nature of study and work, the atmosphere in the family, the socio-economic indicators of the family, living conditions, the nature of the parents’ work, the level of mutual understanding [4].
The physical examination should begin with weight and height. Obesity is an important risk factor for hypertension. Regardless of the child's age, blood pressure should be measured in at least one leg to rule out coarctation of the aorta. Normally, blood pressure in the legs is 10–20 mm higher than in the arms.
Many children have normal clinical examination results, which may require additional laboratory tests. During instrumental and laboratory examinations, the child’s age, medical history, results of physical examination and the severity of increased blood pressure must be taken into account. Diagnostic procedures recommended for children with hypertension are listed in
[8].
Special and specific studies are carried out if appropriate data from the anamnesis, physical examination and screening tests are available. For example, the level of thyroid hormones is determined if the child has corresponding symptoms of thyroid pathology.
The evaluation of a child with hypertension would not be complete without testing the target organs of hypertension. Should be excluded: left ventricular hypertrophy, hypertensive nephropathy, microalbuminuria and thickening of the walls of the carotid arteries [9, 10, 11, 12]. If these disorders are observed, the child should receive antihypertensive therapy.
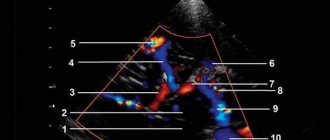
All children with hypertension should undergo echocardiography and fundus examination. 24-hour blood pressure monitoring is increasingly used in children to detect white-coat hypertension [13]. The obtained data, in combination with anamnesis and physical examination, allow us to determine the severity of hypertension, which is necessary for treatment planning and monitoring [14].
There is no doubt that the prevention and treatment of hypertension is more effective in the early stages of its development, i.e. in childhood, and not at the stage of stabilization and organ damage. The goal of hypertension treatment is to achieve sustainable normalization of blood pressure to reduce the risk of developing early cardiovascular diseases.
Objectives of treatment of hypertension:
- achieving the target blood pressure level, which should be <90th percentile for a given age, sex and height;
- improving the patient's quality of life;
- prevention of damage to target organs or reverse development of changes in them;
- prevention of hypertensive crises [4].
Therapeutic tactics in the management of children with high blood pressure are determined by the level of blood pressure, its persistence, and data from additional studies indicating the involvement of other organs in the process or the absence thereof.
Treatment of hypertension in children and adolescents should begin primarily with non-drug methods of influencing high blood pressure.
Of the variety of non-medicinal methods used in practical healthcare, only scientifically based methods are used. These include:
- dietary correction of excess body weight, water-salt metabolism, a significant reduction in table salt consumption (less than 5 g per day) and sufficient potassium intake (3-5 g per day);
- optimization of physical activity: brisk walking and/or running, swimming, inclusion of physical activity in leisure hours and daily activities;
- normalization of the daily routine, rational distribution of free time;
- rational psychotherapy, self-improvement, auto-training, development of resistance to stressful situations;
- therapeutic massage: in the area of the spine and cervical-collar area, segmental, 15–20 procedures per course;
- physiotherapy (electrophoresis with Eufillin, magnesium, calcium, bromine, electrosleep, inductothermy, sinusoidally modulated currents to the sinocarotid zone). The purpose of physiotherapy: to improve the central regulation of vascular tone, general and regional hemodynamics, normalize the functional state of the autonomic nervous system, reduce blood pressure, peripheral vascular resistance, increase the level of compensatory and adaptive processes;
- Spa treatment.
In case of grade I hypertension without left ventricular hypertrophy, obesity, dyslipoproteinemia and carbohydrate metabolism disorders, non-drug correction of high blood pressure can be recommended as the main and even the only method of treating hypertension in children and adolescents. Drug therapy is prescribed if non-drug treatment is ineffective within 6 months.
Prescribing medications for high normal blood pressure is also inappropriate.
If a child or adolescent is diagnosed with stage I high-risk hypertension (left ventricular hypertrophy, obesity, dyslipoproteinemia, impaired carbohydrate metabolism) or grade II hypertension, drug treatment is prescribed simultaneously with non-drug therapy [4]. In case of established hypertension, non-drug methods of treatment and prevention are not an alternative to drug treatment, but an integral component of complex treatment. Its advantages are obvious from the point of view of physiology, simplicity, accessibility, cost-effectiveness, absence of undesirable effects, etc. The introduction of non-drug methods for correcting high blood pressure provides the child and his parents with an active role in promoting health, which, from the point of view of the whole organism, makes it possible to more fully comply with the basic principles of medicine: to treat not the disease, but the patient and do no harm.
So, if non-drug intervention is ineffective within 6 months, and in patients with stage II hypertension or high-risk stage I hypertension, drug treatment is immediately prescribed. In this case, the least number of drugs should be used and in small doses while continuing non-drug treatment and lifestyle changes.
The choice of drug is carried out taking into account the individual characteristics of the patient, age, concomitant conditions: obesity, diabetes mellitus, functional state of the kidneys, dysfunction of the autonomic nervous system and others. In the presence of manifestations of hypersympathicotonia, emotional disorders (neurotic and psychopathic personality development, neurosis, psycho-emotional stress), sedatives are prescribed (preparations of valerian, hawthorn, motherwort; herbal collection - valerian, motherwort, hawthorn, sage, wild rosemary, St. John's wort) and/or nootropic drugs , anxiolytics (Phenibut, Pantogam). These drugs reduce tension, anxiety, fear, improve sleep, which makes them prescribed to patients with asthenoneurotic complaints. The duration of therapy is from 1 to 3 months [8].
In the treatment of autonomic disorders, physiotherapeutic procedures are used: galvanization, diathermy of the sinocarotid zone; electrophoresis according to Vermeule (with 5% sodium bromide solution, 4% magnesium sulfate, 2% Eufillin solution, 1% papaverine solution); electrosleep with a pulse frequency of 10 Hz, massage, acupuncture, water treatments (carbon dioxide, sulfide, pearl baths; Charcot shower, circular shower). Drug treatment of dysfunction of the autonomic nervous system includes drugs that improve cerebral hemodynamics (Vinpocetine, Cinnarizine). The drugs are prescribed in courses lasting at least 1 month. Courses are held 2 times a year.
Read more in the next issue.
L. I. Agapitov , Candidate of Medical Sciences, Research Institute of Pediatrics and Pediatric Surgery of Rosmedtekhnologii , Moscow
Alarming symptoms
If blood pressure is slightly higher than normal, then general health is satisfactory. External manifestations may include irritability and fatigue.
If the blood pressure numbers are very high, then the child feels unwell, he has pain and dizziness, the heart rate increases, pain occurs in the chest, and memory often deteriorates.
There is also malignant AD. In this form, the pressure is very high, and treatment is often ineffective. The risk to health and life is extremely high.
However, the most dangerous situation is the absence of symptoms, which delays diagnosis and treatment.
As you age, your blood pressure may remain above average or rise steadily.
Treatment of hypertension
A moderate form of the disease does not require serious intervention. Usually no medications are prescribed for it. To eliminate symptoms and improve well-being, stress is eliminated from the child’s life both at home and at school, parents monitor and, if necessary, adjust sleep and nutritional patterns. As for nutrition, with hypertension you need to minimize the consumption of salty foods.
One of the reasons for high blood pressure is obesity in any form. In this case, a weight loss diet is selected.
For any type of hypertension, light physical activity will be beneficial: exercise therapy, swimming, walking.
If you notice that your child has started drinking alcohol and smoking, you must immediately eliminate these bad habits.
If the form of the disease is more severe or there is no effect from non-drug treatment, then drugs identical to those prescribed for adults are used. First, the child should take them in small doses, and if the response is insufficient, in higher doses. Every six months, the child needs to be examined by a therapist and/or a pediatric cardiologist. Specialists will adjust the therapy if necessary.
Prevention
- Normalization of the psychological situation at school, creation of a calm atmosphere and home comfort.
- Maintaining an age-appropriate daily routine.
- Limit watching movies and computer games (especially in the evening before bed).
- Elimination of physical and mental overload, alternation of work and rest.
- Distribution of teaching load.
- Regular exercise.
- Daily stay in the fresh air for at least 2 hours and walking for 30 minutes.
- A nutritious diet, 4-5 meals a day.
- Massage of the collar area.
Read more about pediatric cardiology at the YugMed clinic
Prevention of arterial hypertension
Measures to prevent this serious disease come down to lifestyle adjustments:
- reduction and maintenance of normal body weight;
- proper, balanced nutrition according to the regime, reducing the amount of salty, smoked foods, pickled vegetables in the diet;
- light physical activity of half an hour every day;
- avoidance of stress, conflicts and other heavy psycho-emotional stress;
- timely diagnosis and treatment of pathologies that cause increased blood pressure. Source: V.P. Bulatov, T.P. Makarova, D.I. Sadykova, G.M. Farkhutdinova, R.T. Ganieva Arterial hypertension in children and adolescents // Kazan Medical Journal, 2006, v. 87, no. 4, pp. 300-303
Advantages of contacting SM-Clinic
Our clinic employs some of the best pediatric cardiologists and pediatricians in the Northern capital. We have modern diagnostic equipment that allows us to accurately and quickly make diagnoses. Based on the results of the examinations, the specialist will prescribe effective therapy for your child, which will restore good health and eliminate risks in the future.
Sources:
- N.N. Arkhipova. Secondary arterial hypertension in children // Practical Medicine, 2011, No. 5(53), pp. 20-24
- I.P. Bryazgunov. Primary arterial hypertension in children and adolescents // Issues of modern pediatrics, 2003, vol. 2, no. 3, pp. 68-71.
- V.P. Bulatov, T.P. Makarova, D.I. Sadykova, G.M. Farkhutdinova, R.T. Ganieva. Arterial hypertension in children and adolescents // Kazan Medical Journal, 2006, v. 87, no. 4, pp. 300-303.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860989/
Anusha Uddaraju and C. Venkata S. Ram. Hypertension in children, not a “small” problem // Indian Heart J. 2013 Sep; 65(5): 501–503.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Causes
Primary hypotension
- Hereditary predisposition.
- Internal and external influences.
- Perinatal pathology: birth trauma, increased intracranial pressure, etc.
- Frequent respiratory infections in a child.
- Sedentary lifestyle.
- The presence of chronic foci of infection.
- Non-compliance with the daily routine.
- Mental, psychological overload and stress.
- Excessive physical activity.
Secondary hypotension
- Hypothyroidism (lack of synthesis of thyroid hormones).
- Insufficient production of pituitary hormones.
- Diabetes.
- Infectious diseases and intoxications.
- Allergic reactions of the body.
- Heart diseases (heart defects, myocarditis, heart failure).
- Traumatic brain injuries.
- Blood loss (including due to heavy and prolonged menstrual bleeding).
- Anemia (“anemia”).
- Lack of vitamins.
- Hypotrophy (lack of body weight).
- Side effect of drug treatment.
- Somatic diseases: bronchial asthma, neurodermatitis, chronic tonsillitis.
Causes of primary hypertension:
- Hormonal changes in the body during puberty.
- Violation of the daily routine.
- Insufficient sleep duration.
- Increased physical (for example, sports) activity.
- Excessively long time spent at the computer, psycho-emotional trauma and stressful situations.
Causes of secondary hypertension:
- Diseases of the endocrine system.
- The influence of the autonomic nervous system.
- Renal pathology.
- Cardiovascular pathology.
- Brain lesions.
- Poisoning.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a cardiologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Electrocardiography (ECG) | 1400 rub. |
| Echocardiography (ultrasound of the heart) | 3500 rub. |