Inflammatory heart diseases: causes
Among the causes of inflammatory heart diseases, the following are usually identified:
- infectious - diseases can be caused by a wide variety of viruses, microbes, rickettsia, fungi and protozoa; In recent years, increasing importance has been attached to viral infections, with Coxsackie A and B viruses, enteroviruses and influenza viruses coming to the fore;
- toxic - inflammation occurs as a reaction to various toxins, toxins can be very different. This also includes a number of medications (most often used for chemotherapy).
- allergic (immunopathological) - a secondary reaction to the use of certain medications, serums, vaccines, reactions after transplantations;
- infectious-toxic, infectious-allergic - with simultaneous exposure to several different infections, when one of them creates conditions for myocardial damage, and the other is the direct cause of the disease;
- autoimmune - the body’s reaction to the accumulation of antibodies in the tissues of the heart (with rheumatism, connective tissue diseases);
- metabolic – for metabolic disorders (uremic pericarditis with gout);
- physical - trauma or the presence of a tumor (metastatic lesion) - characteristic of pericarditis.
Inflammatory heart diseases: symptoms
The clinical picture of inflammatory heart disease depends on which tissues are involved in the pathological process: inflammation of the heart muscle itself (myocarditis), inflammation of the inner lining of the heart (endocarditis) or inflammation of the pericardial sac (pericarditis). Common symptoms may be prolonged pain in the heart, shortness of breath, palpitations, and often (with an infectious process), an increase in body temperature to febrile levels. At the first suspicion of heart problems due to any infectious disease, you should contact a cardiologist
. Some forms of inflammatory heart disease are acute and lead to very serious consequences.
Wall of the heart: pericardial sac
The human heart is covered on the outside with a special formation: a strong and dense shell. Ancient doctors called this membrane the pericardial sac.
Why a bag? Because the dense fibrous membrane surrounding this organ really looks like a bag in which it is placed.
The pericardial sac consists of not one, but two layers, two films: the epicardium and the pericardium.
Epicard
The epicardium is the inner lining of the sac. The membrane that is directly adjacent to the heart. This is a thin, smooth, transparent, but quite strong connective tissue membrane.
The epicardium is tightly fused with the middle layer of the wall - the myocardium.
In addition to a thin transparent film, the epicardium also contains a small amount of adipose tissue. There is especially a lot of adipose tissue in the area of the apex of the heart and in the area of the grooves and depressions surrounding the heart.
In places where there is adipose tissue (that is, in the apical region and in the region of the grooves), the fusion of the epicardium with the myocardium is less strong.
Pericardium
But the heart is a very important organ. Therefore, its protection from the vicissitudes of the surrounding world should be quite reliable. One thin and delicate film is probably not enough for this. Therefore, its wall is equipped not only with the epicardium, but also with the second part of the pericardial sac. This is a more superficial and thicker layer of it - the pericardium.
What is pericardium
In fact, the endocardium and pericardium are two parts, two films of the pericardial sac. This is the same film that envelops the heart twice. In this case, the inner leaf passes into the outer leaf. This transition occurs at the base of the organ.
The site where the pericardium transforms into the epicardium is called the pericardial volvulus.
The pericardium is a denser and thicker layer. It does not merge with the heart, but freely envelops it.
To avoid confusion, I will say right away that in everyday work, doctors almost always call both layers of the pericardium the pericardium. In other words, the pericardial sac is often called the pericardium, although this is not correct.
Pericardial cavity
The two layers of the pericardial sac (epicardium and pericardium) are not fused to each other over their entire surface. They grow together only at the base of the heart, where one leaf passes into another. This is where the great vessels leave the heart.
Therefore, between the two layers of the pericardial sac there is a slit-like space called the pericardial cavity.
But that is not all. In this cavity or in the pericardial space there is a small amount of fluid that is evenly distributed throughout the cavity.
Human circulatory system
What does a human heart look like?
Where is the human heart?
What's Below the Heart?
Heart cavity
Chambers of the human heart
Human right atrium
Right ventricle of the heart
Left atrium
Left ventricle of the heart
Atrioventricular orifices
How many valves are there in the heart?
Valve apparatus of the heart
Mitral valve
Tricuspid valve
Semilunar valves
Endocardium: the inner lining of the heart
Inflammatory heart diseases - myocarditis
Myocarditis - what is it? Inflammatory damage to the heart muscle, which is manifested by impaired cardiac activity (excitability, conductivity and contractility). Most often it is of a viral nature (half of all cases of myocarditis). The disease affects middle-aged people (30–40 years old, slightly more often women). By origin, myocarditis is:
- rheumatic;
- infectious (viral, bacterial, etc.);
- allergic (medicinal, post-vaccination, transplant);
- for diffuse connective tissue diseases;
- due to exposure to physical factors (trauma, burns, exposure to ionizing radiation);
- idiopathic (unexplained nature) Abramov-Fiedler myocarditis.
The course of myocarditis can be acute, subacute, chronic (recurrent).
Myocarditis: symptoms and diagnosis
Symptoms of myocarditis are often associated with an infectious disease - ARVI, tonsillitis, etc. (in the background or shortly after it). The most common signs of the disease are malaise, weakness, fatigue, shortness of breath, palpitations, heart rhythm disturbances, sometimes discomfort and pain in the chest, and rarely, pain in the joints. In infectious myocarditis, symptoms of an infectious disease usually dominate (fever, increased body temperature, general signs of intoxication). The onset of myocarditis can be asymptomatic, with low-grade or normal temperature; palpitations, “interruptions” in the heart’s function, and shortness of breath are often noted. The severity of symptoms depends on the prevalence and severity of the inflammatory process. Without treatment, signs of heart failure will increase. It is necessary to urgently consult a medical specialist! Timely diagnostic studies ( ultrasound of the heart
,
ECG
, radiography) can reveal:
- increase in heart size;
- heart rhythm disturbances (tachycardia, less often bradycardia, various arrhythmias);
- intracardiac conduction disorders.
Diagnosis of myocarditis often requires an integrated approach. In addition to physical examination, the following are usually used:
- clinical and biochemical blood test;
- electrocardiography
(ECG); - echocardiography
(ultrasound of the heart); - chest x-ray
; - isotope study of the heart;
- MRI of the heart;
- endomyocardial biopsy;
- cultures of blood and other biological fluids;
- comprehensive study of immunological parameters.
By contacting the Energo clinic for help, you will have the opportunity in one place to undergo all the tests necessary for the correct diagnosis of inflammatory heart diseases. You can make an appointment at the Energo clinic using the form on the website or by calling the phone number listed on the page.
How to treat myocarditis?
Mild myocarditis, which occurs without complications, can be treated on an outpatient basis. In more severe cases, hospitalization, mandatory bed rest, etiotropic, anti-inflammatory and symptomatic therapy are required. Etiotropic therapy - treatment of the infection that caused myocarditis (viral, bacterial, fungal, etc.), and maintenance therapy of the primary disease (rheumatism, SLE, thyrotoxicosis, etc.).
Risk factors for developing myocarditis
The development of inflammatory heart diseases is provoked by:
- decreased immunity;
- viral infections and acute infectious diseases (ARVI, tonsillitis);
- foci of chronic infection (caries, tonsillitis);
- hereditary predisposition to inflammatory heart diseases;
- parasitic and fungal diseases.
Why does the heart wall need a pericardial sac?
The pericardial sac is of great importance for the normal functioning of the heart. It performs not one, but several functions.
Limiting and supporting function
The heart is a soft and pliable organ, completely devoid of such support as dense bones. Therefore, the pericardial sac, as a dense and strong formation, maintains its shape and protects it from stretching.
Protective function
Of course, despite all its strength, the heart sac will not be able to protect an important organ from a knife strike or a bullet. But it protects him well from infection.
It is this formation that protects against the spread of infection from the lungs or mediastinal organs to the heart and vice versa.
In other words, the pericardial sac does not allow infection to reach the heart from neighboring organs. But even from the heart, the infection cannot spread to the organs adjacent to it.
Motor function
The human heart is in constant motion. Throughout our lives, it tirelessly makes certain movements that cause blood to rush through the blood vessels.
When moving, the outer shell of the bag (pericardium) easily slides along the surface of the heart, which is covered, adhered to it, by the inner shell of the bag (epicardium).
Why does this sliding occur easily and with minimal energy expenditure? Because between the two layers, between the epicardium and the pericardium, there is a narrow space - the pericardial space.
But that is not all. This space contains a certain amount of liquid, which acts as a lubricant. This “lubricant” prevents the sheets from rubbing against each other. It does not allow the heart to rub against other organs.
This makes the work much easier and easier. And the heart slides easily and naturally inside the pericardial sac.
Inflammatory heart diseases - endocarditis
Endocarditis - what is it? Inflammation of the inner lining of the heart (endocardium), including the heart valves, most often caused by infection. Acute and subacute bacterial endocarditis (infective endocarditis), caused mainly by a bacterial infection, is of independent importance. Endocarditis is often of a secondary nature (it is a consequence of the development of another disease). Secondary endocarditis develops as an inflammatory reaction to immune complexes localized in the endocardium, often combined with myocarditis (characteristic of diffuse connective tissue diseases, rheumatism and other damaging factors). Infective endocarditis is a very dangerous disease. Without treatment, mortality approaches 100%. Infectious endocarditis is often associated with the problem of intravenous drug addiction, when a bacterial agent enters the blood during an intravenous injection, with a complete lack of compliance with the rules of asepsis and antisepsis.
Endocarditis: symptoms
The clinical picture of the disease consists of symptoms of an infectious process, immune disorders and signs of damage to the heart valves:
- with acute onset of endocarditis - symptoms of general intoxication: fever, temperature 38.5 - 39.5 ° C), chills, profuse sweating, pain in joints and muscles, weakness, weight loss;
- with a long course, a grayish with a slight yellowish color of the skin appears (the color “coffee with milk”), on the hands and feet - Osler’s nodes, small hemorrhages in the mucous membranes, a symptom of “drum fingers” - the terminal phalanges of the fingers and toes thicken, the nails become similar with watch glasses;
- development of hepatosplenomegaly is characteristic; possible manifestations of kidney damage (hematuria, proteinuria);
- rough heart murmurs associated with damage to the valve apparatus are heard; later signs of heart failure appear, usually as valvular heart disease progresses;
- characteristic changes develop in the clinical and biochemical blood test (leukocytosis, acceleration of ESR, increase in acute phase indicators - CRP, fibrinogen).
Endocarditis: diagnosis
The diagnosis can be made by a medical specialist when signs of damage to the valvular apparatus of the heart are combined with fever, enlarged liver and spleen, hematuria, skin hemorrhages, anemia, and increased ESR. To verify the diagnosis, blood cultures, ECG and echocardiography are prescribed. Comprehensive examination and treatment is possible only in a hospital setting.
Endocarditis: treatment
The basis of treatment for bacterial endocarditis is early and long-term administration of effective doses of antibiotics, in parallel, symptomatic treatment is carried out. In some cases, it is necessary to resort to surgical treatment methods - valve replacement. It is possible to cure endocarditis with early, properly selected antibiotic therapy, but irreversible changes in the valvular apparatus of the heart can still develop. Prevention of endocarditis consists of timely and correct treatment of infectious diseases, timely sanitation of foci of chronic infection, and compliance with medical recommendations for people with heart defects.
Risk factors for developing endocarditis
The development of inflammatory diseases of the endocardium is provoked by:
- decreased immunity;
- foci of chronic infection in the body (dental caries, periodontitis, chronic tonsillitis, chronic pyelonephritis, chronic thrombophlebitis, furunculosis);
- history of rheumatism;
- history of heart disease;
- bad habits (drug addiction, alcohol abuse, smoking).
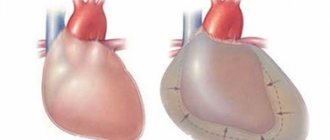
Inflammatory heart diseases - pericarditis
Pericarditis - what is it? Inflammation of the pericardium, the serous membrane of the heart; occurs most often as a complication of one or another disease, less often as an independent disease. The causes of pericarditis are as varied as with other inflammatory heart diseases. In principle, infectious (bacteria, viruses, protozoa and even some types of fungi) and non-infectious (connective tissue diseases, tumors, injuries, post-operative) are distinguished. In form - acute (dry, exudative, with or without cardiac tamponade) and chronic. Pericarditis is manifested by an increase in the volume of fluid in the cavity of the pericardial sac or the formation of fibrous strictures that impede the functioning of the heart.
Pericarditis: symptoms
There are no specific symptoms of pericarditis; in the acute process, heart failure develops. Pericarditis usually causes pain in the chest and left arm, vaguely reminiscent of myocardial infarction, but on the ECG with pericarditis, sufficient R amplitude remains, there is no pathological Q wave, changes concern the final part of the ventricular complex (ST segment and T wave). In addition to pain, there are complaints of shortness of breath, palpitations, general weakness, weight loss, a dry cough may develop, in severe cases - hemoptysis, a feeling of heaviness in the right hypochondrium, an increase in abdominal circumference (a consequence of the progression of heart failure). Acute dry pericarditis often occurs suddenly - with a sharp increase in temperature, stabbing pain in the heart area, and a feeling of heart failure. Exudative pericarditis can develop gradually; the more fluid accumulates in the pericardial sac, the more pronounced the symptoms of pericarditis are: swelling of the neck veins, swelling in the legs, cyanosis of the face, suffocation, swallowing disorders, ascites (accumulation of free fluid in the abdominal cavity), tachycardia .
Pericarditis: diagnosis
If there is any suspicion of cardiac dysfunction, you should urgently consult a specialist. Cardiologist
can make a presumptive diagnosis already during a physical examination.
Auscultatory confirmation of the diagnosis will be the absence or displacement of the apical impulse and percussion expansion of the borders of the heart, muffled heart sounds or pericardial friction noise (with dry pericarditis). Instrumental diagnostics - ECG
,
echocardiography
- will allow you to verify the diagnosis. Pericardial diseases are dangerous, so it is unacceptable to self-medicate or drink “something for the heart.” Without correct and quick diagnosis of the disease, serious consequences are possible.
Pericarditis: treatment
Treatment of inflammatory heart diseases is carried out under the supervision of a doctor, usually in a hospital. Only in some mild cases, outpatient treatment is acceptable. The priority direction of therapy for pericarditis is treatment of the underlying disease. Diuretics may be prescribed to reduce the volume of fluid in the pericardium. If there is a threat of tamponade (compression of the cavities of the heart), a percutaneous puncture is performed and the contents are evacuated. Treatment of compressive (constrictive) pericarditis is only surgical.
Risk factors for developing pericarditis
The development of inflammatory diseases of the serous membrane of the heart is provoked by:
- rheumatism;
- systemic autoimmune diseases;
- severe pneumonia;
- chronic renal failure;
- tuberculosis, brucellosis;
- tendency to allergic reactions.
Prevention of inflammatory heart diseases
Primary prevention of most inflammatory heart diseases consists of two simple rules:
- increasing the body's resistance to infections (hardening, healthy lifestyle);
- timely treatment of focal infections (tonsillitis, caries, sinusitis, furunculosis, etc.).
Secondary prevention of inflammatory heart diseases consists of preventing relapses of the disease, taking measures to monitor patients, and following the recommendations of the attending physician for the treatment of the underlying disease (if any).
Causes and treatment of pericarditis
The article was prepared by cardiologist Ksenia Nshanovna Borel
The pericardium (translated from Greek as “around the heart”) is a double-walled sac surrounding the heart and its large vessels.
The pericardium consists of two layers: one of them is internal, which is tightly adjacent to the heart, and the other is external. Between these sheets there is a cavity filled with a moderate amount of liquid (normally 10-50 ml), which in composition resembles blood plasma. This liquid is necessary to reduce the friction force during heart contractions.
Pericardial fluid is produced by the inner pericardial layer. Any impact on the pericardium is accompanied by increased production of fluid, which does not have time to be evacuated from the cavity and accumulates in it, which is also a manifestation of pericarditis.
The function of the pericardium and pericardial cavity is great.
- Firstly, due to the negative intracavitary pressure, the collapse of the pulmonary veins, which do not have an elastic frame in their wall and which flow into the left atrium, delivering enriched arterial blood, is prevented.
- Secondly, the pericardium delimits the heart from other organs located nearby.
- Thirdly, the pericardium prevents the spread of infection to the heart if it develops in the lungs or pleural cavities.
- Fourthly, the pericardium protects the heart from excessive stretching during the diastole phase.
Pericardial diseases (pericarditis) are found not only in the practice of a cardiologist. Doctors of any specialty may encounter symptoms of pericarditis, since most often damage to the pericardial layers is a symptom and even a complication of other diseases.
Men under 65 years of age are more susceptible to developing pericarditis than women.
The main causes of pericarditis can be divided into 2 large groups: infectious and non-infectious.
Exposure to specific agents can often cause excessive production of pericardial fluid and its excessive accumulation in the pericardial cavity at varying rates. The more intense and rapid the increase in fluid volume occurs, the faster the situation develops, which can be life-threatening.
Infectious pericarditis can be caused by any viral or bacterial agent, parasites or fungi.
Non-infectious (so-called “aseptic”) pericarditis can develop against the background of rheumatic and oncological diseases, with chronic renal and heart failure, with hypothyroidism, after radiation therapy and exposure to radiation, after a myocardial infarction and after open heart surgery, with injuries nearby organs, when taking certain medications (especially antitumor drugs).
Pericarditis can be acute, chronic and recurrent , depending on the timing of development and the duration of symptoms. A separate group of pericardial diseases is exudative pericarditis (also edematous, effusion), which is characterized by excessive accumulation of fluid between the layers of the pericardium.
Symptoms of pericarditis can also be divided into 2 groups: symptoms of the underlying disease and symptoms of pericardial damage.
Depending on the specific cause that provoked the development of pericarditis, the symptoms of the underlying disease can vary: from signs of viral and bacterial inflammation to endocrinological deficiency in thyroid pathology.
It is always necessary to find out the possible cause of pericarditis, since symptomatic therapy has only a temporary effect, and complete resolution of the disease can only be achieved by acting on its cause.
Symptoms of damage to the pericardial layers may be as follows.
- Pain in the heart area, not associated with breathing, sometimes worsens in a horizontal position, weakens in a sitting position, bending forward.
- Sometimes shortness of breath and decreased blood pressure may occur.
- In severe cases, loss of consciousness develops.
How to recognize pericarditis?
The standard for examining patients with suspected pericarditis includes the following diagnostic methods:
- ECG
- Ultrasound of the heart
- MRI of the heart
- chest x-ray
- blood test to determine if there is inflammation and damage to the heart muscle
How to treat pericarditis?
Not all cases of pericarditis require active medical intervention. In some situations, observation is sufficient. If we are talking about severe acute clinical manifestations, accompanied by a systemic inflammatory reaction, pronounced accumulation of fluid in the pericardial cavity, insufficient effectiveness of taking anti-inflammatory drugs and some other unfavorable signs, then in such situations hospitalization may be required.
As we have already discussed above, in such cases you should look for the cause and act on it.
In addition to cause-related therapy, nonspecific therapy is used, which is effective in most cases of pericarditis.
If we are talking about the presence of a large amount of fluid in the pericardial cavity, then pericardial puncture may be required to evacuate it. If the amount of fluid is small, then they are limited to active observation and treatment of the underlying disease.
Sometimes, as a result of pericarditis, especially with repeated episodes of inflammation and lack of treatment, the pericardial layers can “stick together” and thicken with the formation of the so-called “shell heart”. This is a severe pathology with the development of severe heart failure. The only effective treatment in this case is surgical removal of the pericardium.
Be attentive to your heart! Take care of him!
MAKE AN APPOINTMENT WITH A CARDIOLOGIST