What is the atherogenic coefficient in a blood test?
The atherogenic coefficient is the balance of “good” cholesterol and total cholesterol, which in the future can go into a bound state (LDL), and represents their proportional ratio.
What is this coefficient? At a general, everyday level, everyone knows that there is “bad” (or LDL cholesterol) and “good” (HDL cholesterol) cholesterol. Complex molecules of good cholesterol are too large to be absorbed into tissues; they “collect” molecules of “bad” fatty alcohol and transport them to the liver for processing. On the contrary, “bad” cholesterol settles on the walls of blood vessels and forms plaques that narrow the lumen of the blood vessel and impair blood circulation. In addition, total cholesterol also circulates in the blood, that is, the substance in an unbound state.
At the moment, this is the most accurate indicator of the state of lipid (fat) metabolism in the body and assessing the risk of atherosclerosis and other cardiovascular diseases (although the role of fatty alcohol in the development of pathologies of this kind is controversial).
In addition, the definition of this indicator can be informative in the following cases:
- Diagnosis of thyroid and liver diseases;
- Controlling cholesterol dynamics (with drug therapy);
- During the initial preventive examination of the patient.
Reasons for a reduced atherogenic index
A decrease in the atherogenicity rate in people belonging to various population groups does not occur very often. There are several reasons that can reduce performance:
- regular use of statins - the most popular drugs today to reduce the concentration of lipoproteins in the body;
- the patient regularly performs feasible sports activities, which is almost impossible for the cardiologist’s regular clients who are overweight;
- the patient was on a low-cholesterol diet for a long period of time before donating blood for analysis to determine the atherogenic coefficient;
- the patient took estrogens, antifungals, erythromycin, which helps reduce this index.
Norm of atherogenic coefficient
When calculating the atherogenicity coefficient, experts use a simple formula:
Atherogenicity coefficient (Atherogenicity Index) = (Total cholesterol - HDL) / HDL
* HDL - high density lipoproteins.
The norm of the atherogenic index varies from laboratory to laboratory; in general, this indicator is normal in the range from 2 to 2.5 units (but not higher than 3.2 for women and 3.5 for men). An indicator above the specified norm may indicate the presence of atherosclerosis. However, the coefficient alone does not allow us to accurately state the presence of the disease.
If the atherogenic index is below the specified norm, this is not a cause for concern. This result does not matter.
Reasons for the downgrade
Why there is a reduced atherogenicity coefficient has not been sufficiently studied, despite the seriousness of such a deviation from the norm. Among the main reasons are:
- liver disease, which synthesizes 80% of all cholesterol;
- artificial restriction of animal fats in the diet - diets, therapeutic fasting, vegetarianism;
- problems with the digestive system, as a result of which the absorption of fats in the intestines is impaired;
- hyperthermia against the background of infectious processes in the body, requiring large energy costs;
- anemia, as a consequence of insufficiency of the circulatory system;
- stress;
- intoxication, food poisoning;
- incorrect or uncontrolled use of statins;
- excessive physical activity, including sports;
- taking medications: estrogens, antimycotics, antibiotics.
Increased atherogenicity coefficient, what to do?
If the results of laboratory tests reveal a high coefficient, this indicates that the body produces predominantly “bad” cholesterol. Despite the lack of evidence about the direct and main role of fatty alcohol in the formation of cardiovascular diseases and pathologies, it is not worth the risk. Measures should be taken immediately to normalize the indicator.
You can do this in two ways:
- Change your lifestyle and diet.
- Start taking specialized medications.
Lifestyle
The increase in the index is due to a number of reasons:
- Presence of bad habits (smoking, alcohol abuse, drug use). Psychoactive substances “inhibit” normal fat metabolism and disrupt fat synthesis.
- Sedentary lifestyle. Physical inactivity leads to stagnant processes. Fats and fatty complexes are synthesized too actively.
From this we can conclude that to normalize the index you need:
- Lead a more active lifestyle. Strong physical activity can normalize the concentration of cholesterol in the blood and lipid metabolism. A healthy person is recommended to do 4 sessions during the week, 35-40 minutes each. If you have a history of diseases, you should consult a doctor to exclude contraindications and select the optimal physical activity regimen.
- Give up bad habits.
Diet
It is advisable to limit consumption or completely avoid the following foods:
- Sausages;
- Fatty fermented milk products (sour cream, cream, butter);
- Products rich in trans fats (margarine, palm oil spreads, etc.)
On the contrary, you should include in your diet:
- Fish. Cod, hake, flounder and others. Frying should be avoided, giving preference to boiling.
- Nuts (almonds, walnuts). Nuts contain monosaturated fatty compounds and can reduce the amount of cholesterol in the blood.
- Fruits vegetables. Especially beets. Potatoes are not recommended.
- Chocolate and green tea.
- Garlic.
- Cereals.
As well as other products containing fats of vegetable rather than animal origin.
Read more: How to lower cholesterol at home, without drugs?
Taking medications is another way to reduce the atherogenic index. However, statins (cholesterol-lowering drugs) have many side effects and should be taken strictly on the advice of a doctor and in a very limited number of cases.
What analysis determines
Monitoring the state of lipid metabolism is necessary to exclude atherosclerosis as a provoking factor of cardiovascular diseases or infertility in the case of low blood cholesterol. Low cholesterol levels are no less dangerous than high cholesterol levels, since there are no symptoms of hypocholesterolemia in the early stages, laboratory diagnosis remains the only way to identify the pathological process. Lipoproteins of any density, the atherogenic index is determined by a biochemical blood test independently, but more often as part of a complex lipid profile or lipidogram.
Preparing for the test
Pre-preparation for a laboratory blood test is standard, but mandatory, since it helps to minimize possible factors of unreliable results:
- in contrast to the detection of hypercholesterolemia, the diet before taking the test if low cholesterol is suspected is prescribed only the day before: you need to refrain from fatty foods, make dinner as light as possible;
- the day before testing, you should not overexert yourself physically, if possible, do not overexert yourself mentally or emotionally;
- alcohol is not consumed one day before taking a blood test, smoking is strictly prohibited one hour before the test;
- Blood is donated in the morning, on an empty stomach, in a comfortable sitting position;
- The doctor must be warned about all medications the patient is taking.
If other tests are scheduled on the same day, ultrasound, for example, they are performed after the blood test. To ensure reliability, doctors recommend duplicating the analysis in another medical laboratory.
Progress of the study
If low cholesterol is suspected, an express diagnostic method is often used. It's convenient and fast. The analyzer resembles a glucometer. Battery operated. To determine cholesterol levels, a strip test and a drop of the patient’s blood (after puncturing the skin of the finger with a special lancet) is sufficient. Three seconds, the answer is ready. The analyzer memory is designed for 100 previous results. The mini-device can be used at home.
Of course, this is an indicative analysis, but it makes it possible to make a decision about the need for further examination of the patient or records the cholesterol level that does not cause concern. In the latter case, the patient is recommended to self-monitor lipids or regularly take a rapid test at the clinic. If cholesterol levels rise or fall, a detailed examination is carried out.
In the laboratory, blood is taken from a vein, with the patient always sitting (standing or lying down affects the reliability of the results). The answer is ready in a maximum of three days.
Interpretation of results
The atherogenicity coefficient is not often reduced. But if it is determined and does not tend to increase on its own, the patient must be treated. To make a diagnosis, the reliability of the analysis results is very important. The following can affect the decrease in KA:
- newfangled diets based on fasting;
- impaired absorption of fats in the gastrointestinal tract due to digestive problems;
- burns of any origin: from solar with a large area of damaged surface to thermal and electrical injuries;
- hypothyroidism;
- multiple myeloma;
- thalassemia;
- megaloblastic anemia;
- infections of various etiologies;
- sepsis;
- cirrhosis of the liver in the terminal stage;
- malignant tumors of the liver, biliary system;
- tuberculosis, severe lung pathologies;
- taking estrogen (contraceptive pills, a course of therapeutic, replacement therapy);
- physical and emotional stress.
Complexes with this research
Stress complex Assessment of the state of the body during stress 4,310 RUR Composition
Anti-aging diagnostics in postmenopause Control of age-related changes during the postmenopausal period 12,630 RUR Composition
Advanced male anti-aging diagnostics Advanced monitoring of key indicators in men aged 40+ RUR 33,710 Composition
IN OTHER COMPLEXES
- Healthy interest 4,250 RUR
- Male anti-aging diagnostics RUB 13,300
- Fitness monitoring 6,780 RUR
- Nutritionist recommends RUB 7,570
- Lipidogram. Diagnosis of atherosclerosis 480 R
Should I raise
If the atherogenicity index is lowered, this is very bad, because with a 100% guarantee it warns of the possibility of developing many serious diseases, a significant increase in the risk of developing alcoholism or drug addiction. From this point of view, you need to pay attention to the following symptoms, which correspond to decreased KA:
- a sharp decrease in appetite;
- muscle weakness;
- fat in the stool (steatorrhea);
- sudden mood swings;
- decreased sexual activity;
- decreased tactile sensitivity;
- enlarged lymph nodes for no apparent reason.
All these are indications for taking a biochemical analysis. Detection of a reduced atherogenic index requires correction. It seems that you can self-medicate by enhancing your daily diet with animal fats. But this is a dangerous misconception. One wrong step, and a person faces fatal complications against the background of apparent health. Only a doctor can prescribe adequate therapy. The first person to contact in case of low KA is an endocrinologist, then a cardiologist, nutritionist, and therapist.
There are no special medications that raise cholesterol levels today. The solution is a diet that will stop the decline in indicators (ideally, prevent them). The rules are very simple:
- complete taboo on alcohol, cigarettes, drugs;
- introduction into the diet of seafood, fatty varieties of sea fish, offal, pork, beef, lamb, fatty cheeses, eggs in all varieties, butter, olives, olive oil;
- To neutralize LDL (“bad” cholesterol), unlimited quantities of vegetables and fruits, greens – everything that contains vitamin C (a natural antioxidant) are required.
Movement is another way to normalize lipid metabolism. Normal cholesterol levels are the main goal for the doctor and the patient.
The importance of cholesterol in the body
To maintain your health, you need to understand the importance of fats in the human body and their origin. At the same time, you need to know which fat compounds are dangerous and which perform beneficial functions. So, what is the atherogenic coefficient and why might it be elevated?
Cholesterol performs many functions in the body: it imparts rigidity to phospholipid molecules
, participates in the synthesis of sex hormones, is the basis of bile acids and vitamin D, and takes part in regulating cell permeability.
A notable feature of cholesterol is its inability to dissolve in water, so it cannot be transported to cells by blood. Therefore, cholesterol is found in special compounds that tend to dissolve well and be transported with protein. Such compounds are called lipoproteins. They come in different types and differ depending on the mass and degree of solubility:
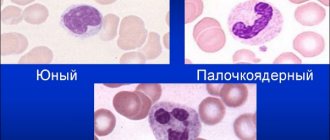
• high molecular weight (high density lipoprotein HDL), • low molecular weight (low density lipoprotein LDL), • very low molecular weight (very low density lipoprotein VLDL).
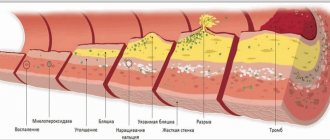
LDL and VLDL are compounds that are poorly soluble, and the cholesterol found in them is prone to precipitation, which leads to the formation of atherosclerotic plaques in the blood vessels. Due to this division and the properties of some cholesterol compounds, it is generally accepted that low molecular weight and very low molecular weight lipoproteins are “bad” fats.
Numerous compounds confirm the existence of a relationship between the content of various types of fatty compounds and basic indicators of human health. This dependence leads to the presence of a large amount of OPNP in the blood, which contributes to the development of atherosclerosis in the body.
To assess the threat of developing this disease, in medicine there is a special value - the atherogenic coefficient (AC), the norm of which implies a proportional ratio of “bad” fats to their total amount. Today, this indicator can most accurately tell about the state of fat metabolism, and with its help it is possible to assess the risks of atherosclerosis and the occurrence of other pathologies of the human vascular system.
How to be vegetarians
Since our liver is capable of producing cholesterol itself, some people have decided that it is possible and necessary to do without animal fats of exogenous origin. They are called vegetarians. But despite scientific research that proves the complete chemical and biological identity of exo- and endogenous fatty alcohol (this is what the human body synthesizes), doctors are not supporters of a complete rejection of dietary fats of animal origin.
This position is explained simply: the quantity, quality and ratio of vegetable and animal fats in the diet affects the activity of the brain, which itself consists of 60% cholesterol. The nervous system especially needs unsaturated fatty acids omega-3. They enter the body only with seafood, fatty fish (mackerel, tuna, halibut, salmon, herring, trout, salmon), olives, walnuts, and flaxseed.
If these acids are not enough, a real disaster occurs in the body. The most emotional children and pregnant women are the first to suffer:
- memory is impaired;
- lack of concentration;
- a person is “covered” by a feeling of despondency, depression, and lack of energy.
Vegetable fats and endogenous analogues are not able to solve the problem. Therefore, not everyone can be vegetarian. For those who do not consume animal fats, the atherogenic coefficient automatically decreases. This means it needs to be raised. But in such a strict restrictive framework, this is problematic.
Men are especially affected, whose blood vessels, unlike women's, are defenseless from any fluctuations in HDL and LDL. Essentially, men need to eat high-calorie foods because they burn calories more actively than women. But they are a priori deprived of it. The recommendations in this situation are clear:
- before becoming vegetarians, it would be a good idea to check the state of your lipid metabolism and clarify the atherogenicity index;
- if the decision is made, regular monitoring of the LDL to HDL ratio is necessary to avoid the risk of fatal complications;
- in the event of a sharp drop in the atherogenic coefficient, a specialist’s consultation is needed; you may have to forget about vegetarianism in order to restore the energy reserves necessary for work, an active family, and social life.
Some are trying to “gain fat” and return to vegetarianism. This is the worst option, which in practice ends in AMI. Fluctuations in the “cholesterol pendulum” have the most negative effect on blood vessels and the heart.
What is the danger
An increased coefficient of atherogenicity is an unfavorable sign, but it can fluctuate throughout life. KA levels may vary among different people with the same level of total cholesterol. This depends on the predominance of low- or high-density lipoproteins in the bloodstream. Bad cholesterol (LDL and VLDL) always causes an increase in the atherogenic index. This is, in fact, a prognostic sign that assesses the risk of either atherosclerosis in general or its complications in particular.
The latency and asymptomatic nature of atherosclerosis for many years has been its main danger to humans. If the disease is diagnosed only by its complications, most likely the outcome will be tragic.
The most dangerous complication of atherosclerosis, which can be prevented by knowing the patient’s atherogenicity index at the very beginning of the pathology, is myocardial infarction.
All tissues and organs receive a sufficient amount of blood with nutrients and oxygen only if the heart muscle functions normally. The narrowing of the coronary arteries as a result of the formation of cholesterol plaques in them disrupts the nutrition of the heart itself, reduces its contractility, causes tissue hypoxia, and insufficient supply of nutrients to them. When the coronary lumen is blocked by only 15%, there is already a risk of angina pectoris, tachycardia, and weakened myocardial contractility. When the cholesterol supply to the heart is blocked, a heart attack develops with a possible fatal outcome.
Unbearable pain in the chest, fear of death, cold sweat - signs of necrosis of the heart muscle, requiring immediate medical intervention. What is the role of the spacecraft in this case? It's hard to overestimate her. A high atherogenic index warns a person about this scenario. Everything else depends on the behavior of the patient himself, on how he manages the information received. Compliance with the doctor’s recommendations, developed individually for each specific person with high KA, literally prolongs his life.
The second severe complication of high coronary artery disease, and therefore atherosclerosis, is stroke. The brain, like no other organ, needs constant nutrition, glucose and oxygen. Any deviation from the norm causes irreparable changes in neurocytes. Atherosclerosis of the cerebral arteries is manifested by shortness of breath, severe headaches, loss of consciousness, difficulty swallowing, paralysis, coma. The outcome of untimely intervention by doctors is death. KA also warns a person about such a scenario, forcing him to take care of his own health.